Abstract
Analysis of urine samples using liquid chromatography-tandem mass spectrometry (LC-MS/MS) has previously revealed high rates of non-adherence to antihypertensive medication. It is unclear whether these rates represent those in the general population. This study aimed to investigate whether it is feasible to collect urine samples in a primary care setting and analyse them using LC-MS/MS to detect non-adherence to antihypertensive medication. This study used a prospective, observational cohort design. Consecutive patients were recruited opportunistically from five general practices in UK primary care. They were aged ≥65 years with hypertension and had at least one antihypertensive prescription. Participants were asked to provide a urine sample for analysis of medication adherence. Samples were sent to a laboratory via post and analysed using LC-MS/MS. Predictors of adherence to medication were explored with multivariable logistic regression. Of 349 consecutive patients approached for the study, 214 (61.3%) gave informed consent and 191 (54.7%) provided a valid urine sample for analysis. Participants were aged 76.2 ± 6.6 years and taking a median of 2 antihypertensive medications (IQR 1–3). A total of 27/191 participants (14.2%) reported not taking all of their medications on the day of urine sample collection. However, LC-MS/MS analysis of samples revealed only 4/27 (9/191 in total; 4.7%) were non-adherent to some of their medications. Patients prescribed more antihypertensive medications were less likely to be adherent (OR 0.24, 95%CI 0.09–0.65). Biochemical testing for antihypertensive medication adherence is feasible in routine primary care, although non-adherence to medication is generally low, and therefore widespread testing is not indicated.
Similar content being viewed by others
Introduction
The population is ageing [1] and the number of people living with age-related chronic conditions is increasing [2]. This is accompanied by more prescriptions of long-term medications. More than one in three adults aged ≥75 years are prescribed five or more medications [3], a situation known as polypharmacy [4]. Polypharmacy is associated with partial or non-adherence to medications, particularly those prescribed for the prevention of disease [5,6,7]. Non-adherence to medications used for the prevention of cardiometabolic diseases is important since this can significantly increase an individual’s risk of future events [8, 9]. However, identifying non-adherence can be difficult [10]. Information about an individual’s medication adherence can be captured through direct questioning [11], questionnaires [12, 13], directly observed dosing [14], prescription refill data, pill counts, and electronic ‘event’ monitoring [11], but used in isolation, these approaches have limitations which affect their ability to accurately confirm medication adherence in routine clinical practice [15, 16].
New methods for identifying non-adherence now exist using liquid chromatography-tandem mass spectrometry (LC-MS/MS) to detect a number of medications measurable in an individual’s urine [17]. This approach has revealed high rates (25–42%) of previously unrecognised non-adherence to medication in hypertensive patients [6, 17]. However, most previous studies utilising this approach have enroled complex hypertensive patients from clinics where individuals have been referred due to suspected non-adherence or suboptimal blood pressure control [6, 17, 18]. It is unclear whether the medication adherence rates seen in these complex patients are representative of those in the general population presenting in primary care, or even whether patients would be willing to provide urine samples for assessment of adherence in this setting. The present study, therefore, aimed to investigate whether it is feasible to collect urine samples in a primary care setting and analyse them using the LC-MS/MS method to measure adherence to antihypertensive medication.
Methods
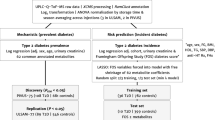
Study design
This study used a prospective, observational cohort design, enroling participants in primary care aged ≥65 years with hypertension and prescribed at least one blood pressure lowering medication. Patients attending the practice were asked to give informed consent and provide a urine sample for researchers to examine whether antihypertensive medications were present in their system. Anonymised data were collected for patients declining to participate in the study for comparison to those who did participate. Ethical approval for this study was given by South Central—Oxford A Research Ethics Committee (ref: 18/SC/0647). Detailed methods are given in the Supplementary appendix.
Study participants
Consecutive patients aged ≥65 years with an electronic medical record coded diagnosis of hypertension and prescribed at least one blood pressure lowering medication were approached opportunistically. Participating general practices were located in the Thames Valley region of England.
Participating general practitioners (GPs) were asked to identify patients attending routine medication reviews or chronic disease management clinics meeting the eligibility criteria. Consent and sample collection took place directly after each routine appointment to ensure the subsequent assessment of medication adherence was representative of an individual’s true drug-taking behaviour.
Data collection
For all patients approached to participate in the study, members of the care team extracted anonymised data from their electronic health record, detailing basic patient characteristics and medical history. Data included information relating to patient characteristics, blood pressure, medical history, and all antihypertensive medications prescribed. Prior to collecting the urine sample, all consenting participants were asked the question “Have you taken all of your blood pressure pills today?” and responses were categorised as “all medications”, “some medications”, or “no medications”.
Urine sample collection and analysis
Participants were informed from the outset that the study was investigating the feasibility of collecting urine samples and testing whether patients had taken all of their medications as prescribed. They were reassured that this information would remain entirely confidential and members of the care team would not be made aware of the results of the urine test. A 10 ml urine sample was collected in a standard plastic container immediately after informed consent had been obtained. Each sample was transferred from the clinic site to the laboratory at University Hospitals of Leicester at room temperature, via a post office next day delivery service. We have previously demonstrated that samples remain stable for 72 h after collection [19].
All samples received by the laboratory were stored at −80 °C and then batch analysed at the end of the study. LC-MS/MS was performed to detect all antihypertensive drug classes, using an Agilent Technologies 1200 series High Pressure Liquid Chromatograph interfaced with an Agilent Technologies 6410 Triple Quad Mass Spectrometer fitted with a Jetstream electrospray (ESI) source [17]. The test is a standard laboratory test that is accredited by United Kingdom Accreditation Service (UKAS). All samples were destroyed at the end of the study, after the analysis had been completed.
Sample size calculation
The study aimed to collect anonymised data from approximately 285 patients, gathering urine samples from at least 200 consenting participants. This assumed 70% [20] of those approached would give informed consent for their samples to be collected and analysed, allowing a recruitment rate of 70% to be estimated with an accuracy of ±6% (95% confidence interval of 64% to 75%). Recruitment of at least 200 participants was estimated to be sufficient to calculate a medication adherence of 75% to within ±7%.
Statistical analysis
The primary outcome of this study was to determine the proportion of patients attending a routine medication review or check-up in primary care (denominator population) who gave informed consent to provide a urine sample for analysis of medication adherence (numerator). We did not pre-specify feasibility criteria for this study, and so have applied criteria previously described in the literature which defined feasibility as ≥50% of patients agreeing to provide a sample and 95% of collected samples being suitable for analysis [21]. Participant characteristics predicting the likelihood of consent to provide a urine sample were explored using multivariable logistic regression.
Medication adherence was defined as a binary outcome; adherent patients were those in whom all prescribed antihypertensive medications were present in their urine sample. Non-adherent patients were those in whom only some or none of their prescribed medications were detected in the urine sample. Adherence to medication was estimated using descriptive statistics, across the entire study population and sub-grouped by type of medication prescribed and whether blood pressure was controlled (±140/90 mm Hg).
Predictors of non-adherence to medication were explored with logistic regression, including age, sex, blood pressure, co-morbidities, and the number of antihypertensive medications as independent predictor variables. Sensitivity analyses were performed including blood pressure control (±140/90 mm Hg) in the model. Analyses were undertaken for descriptive purposes only, so no attempt was made to reduce the model using selection methods. All analyses were undertaken using STATA version 16.0 (MP edition, StataCorp, College Station, Texas, USA).
Results
Population characteristics
A total of 349 consecutive, eligible patients from five semi-urban general practices in areas of relatively low deprivation were approached for the study. Of these, 214 (61.3%, 95%CI 56.0% to 66.5%) gave informed consent to provide a urine sample for analysis (Fig. 1). The most common reasons for non-participation were a lack of time to attend an additional clinic appointment and provide a sample. One participant withdrew consent.
Patients were aged 76 ± 7 years, with similar proportions of men (171, 49.1%) and women (178, 50.9%), and a mean blood pressure of 135/75 mm Hg (Table 1). Of those giving informed consent, 191 (89.3%, 95% CI 84.3% to 93.1%) were able to provide a sample suitable for analysis and were included in all analyses of medication adherence. Of those not providing a sample suitable for analysis, 19 (5.4%) were unable to produce a urine sample, three (0.9%) provided an insufficient amount (i.e., <10 ml) of urine to enable analysis and one urine sample (0.3%) was lost in transit from the clinic to the laboratory.
Predictors of consent to provide urine samples
In multivariable analyses, being male (Adjusted odds ratio [OR] 1.78, 95%CI 1.09 to 2.91), having a history of arthritis (OR 4.59, 95%CI 2.61 to 8.08) and those with higher systolic blood pressure (OR 1.02, 95%CI 1.00 to 1.04) were more likely to consent to the study, although mean systolic blood pressure was broadly similar between groups (135 vs 133 mm Hg; Table 1). Patients prescribed more antihypertensive medications (OR 0.63, 95%CI 0.48 to 0.82) were less likely to give informed contested for urine sample collection (Fig. 2).
Adherence to antihypertensive medication
A total of 18 participants (9.4%, 95%CI 5.7% to 14.5%) reported not taking their medications on the day of urine sample collection, and a further 9 (4.7%, 95%CI 2.2% to 8.8%) reported that they had only taken some of their prescribed medications (Table 2). Of the 18 participants stating that they had not taken any medications yet that day, 16 (88.9%, 95%CI 65% to 98.6%) were shown to be adherent by LC-MS/MS and two (11.1%, 95%CI 1.4% to 34.7%) were taking at least one, but not all of their prescribed medications. Of the nine participants stating that they had only taken some of their prescribed medications that day, seven (77.8%, 95% CI 40.9% to 97.2%) were measured as fully adherent and two (22.2%, 95%CI 2.8% to 60.0%) were taking some of their prescribed medications.
Overall, 182 participants (95.3%, 95%CI 91.2% to 97.8%) were fully adherent to all of their antihypertensive medications, eight (4.2%, 95%CI 1.8% to 8.1%) were partially adherent (i.e., taking at least one, but not all of their medications) and only one participant was entirely non-adherent, despite reporting taking all of their antihypertensives. Loop diuretics were the most commonly prescribed antihypertensive drug class not detected in participant’s urine samples (Table 3).
Predictors of adherence to antihypertensive medication
In multivariable analyses, patients prescribed more antihypertensive medications (OR 0.24, 95%CI 0.09 to 0.65) were less likely to be adherent to antihypertensive medication (Fig. 3). No other factors predicted non-adherence to antihypertensive medication. Findings were unchanged in sensitivity analyses including blood pressure control as a variable in the model, which was not associated with medication adherence (OR 0.88, 95%CI 0.17 to 4.49).
Discussion
Summary of main findings
In this study of 349 hypertensive patients attending primary care for a routine medication review or chronic disease management clinic, almost two thirds (61%) of patients agreed to provide a urine sample to test for the presence of antihypertensive medication, suggesting patients are willing to engage with this method of measuring medication adherence in routine clinical practice. Only 89% of consenting patients were able to provide a urine sample suitable for analysis, which is lower than the 95% of samples considered to indicate the feasibility and may reflect the age of our population [21]. Amongst those 191 participants who consented and were able to provide a sample, self-reported adherence to medication did not appear to be related to biochemically determined adherence. This may have been caused by traces of drugs taken on previous days still being present in the participant’s sample as LC-MS/MS can detect medications for up to 4–6 half-lives in the urine [22]. It may also reflect uncertainty from the patient about when they last took their tablets. Overall, non-adherence to antihypertensive medication was very low (<5%), in contrast to previous studies using this approach [6, 17, 18]. This may be a conservative estimate, given the limitations of the LC-MS/MS method in terms of detecting drugs with longer half-lives, and considering that a third of patients declined to participate in the study, although the characteristics of consenting and non-consenting patients were broadly similar. Given these low rates of non-adherence, widespread testing using this approach should not be recommended in the community.
Strengths and limitations
The present study included a sample of patients broadly representative of the population approached in primary care, in terms of age, blood pressure, co-morbidities, and antihypertensives prescribed. Patients were recruited from practices of relatively low deprivation and those taking multiple antihypertensive medications were less likely to participate and so caution should be exercised when applying these findings to patients with high deprivation on multiple treatments.
Biochemically determined adherence using the LC-MS/MS method can objectively determine whether a patient has taken a prescribed medication, and so is not prone the same biases that affect other methods for measuring adherence such as self-reported adherence or pill counts [15]. However, this approach only permits the assessment of medication adherence at a single moment in time. As such, it is dependent on the half-life of each individual drug examined, and the ability of the patient’s body to metabolise it. The LC-MS/MS method can detect medications for up to 4–6 half-lives in the urine. Therefore, medications taken on previous days may still have been detected, even if a patient had not taken their tablets on the day of urine sample collection. This could give the impression that an individual was adherent to therapy when in fact they had not taken their medication that day. Indeed, in the present study, there was some discrepancy between the results of the LC-MS/MS analysis and self-reported medication adherence. Thus, we would recommend a multi-method approach to determining medication adherence in routine practice, perhaps combining the LC-MS/MS method with direct questioning [11].
Opportunistic recruitment was necessary in this study to ensure patients did not modify their medication-taking behaviour in anticipation of the urine sample collection. However, this meant that some patients could not participate due to a lack of time available to stay at the clinic. Our analyses comparing the characteristics of patients consenting and not consenting suggested few important differences, except for men and those with arthritis who were more likely to participate.
In sensitivity analyses, blood pressure control was found not to be predictive of medication adherence. We defined BP control as +/− 140/90 mmHg, but for some individuals with co-morbid conditions such as diabetes, the definition of BP control may have been different [23].
Comparison with existing literature
Adherence to antihypertensive medication has been widely studied, with estimates of non-adherence varying depending on the population studied and the methods used to measure medication adherence [24, 25]. Studies in different hypertensive populations using self-report questionnaires such as the Morisky medication adherence scale [12] have found rates of non-adherence of between 31.2% (hypertensive patients with co-morbidities), 45.2% (hypertensive patients), and 83.7% (hypertensive patients with uncontrolled blood pressure) [24]. Similarly, studies using objective biochemical measures (such as the LC-MS/MS method) have observed non-adherence rates of 25–42% [6, 17].
One previous study conducted in Irish primary care [21], approaching 453 patients with apparent treatment-resistant hypertension, found this method of determining adherence was feasible in 52% of patients approached. Of these, 24% were found to have partial non-adherence to antihypertensive medication and 2% were completely non-adherent. Another study in England including 228 diabetic patients attending primary care for an annual review, found non-adherence to antihypertensives was just 8%, with the highest of non-adherence rates (10%) seen for ACE inhibitors and angiotensin II receptor blockers [26].
To our knowledge, this is the first study conducted in primary care to assess medication adherence in the general hypertensive population. It reveals lower rates of non-adherence to antihypertensive medication (<5%) than previously reported [6, 17, 18, 21] and confirms previous observations about reduced adherence in patients taking multiple medications [5,6,7]. Differences in observed rates may be due differences in the populations studied. Participants in the present study generally had well-controlled blood pressure (mean 135/75 mm Hg; 62% controlled) and were not necessarily attending routine practice to address problems with their hypertension management. In contrast, previous studies have often enroled complex hypertensive patients from clinics where individuals have been referred due to suboptimal blood pressure control [6, 17, 18, 21]. We found non-adherence was most common for loop diuretic prescriptions, which may be related to the effect they can have on urinary urgency in older patients (i.e., they are less likely to be taken on days when an individual is expecting to be out of the house for a significant period of time). Loop diuretics may also be cleared from the kidneys quicker and non-adherence to these drugs may be linked to non-adherence associated with taking multiple medications [6].
Implications for research and/or practice
The present findings highlight the discrepancy between patient self-reported adherence and actual medication-taking behaviour. However, given the low rates of non-adherence observed here, objective methods for measuring adherence (such as LC-MS/MS) may not be necessary for all patients in a primary care setting. These tests cost £40 per patient and are becoming increasingly popular in secondary care (currently 35 hypertension referral centres around the UK are using them). They are thought to be cost-effective as an intervention to improve medication adherence, particularly when targeted at groups most likely to be non-adherent [27]. The present study suggests that one such group to target may be those individuals prescribed multiple antihypertensive medications. Though not tested here, these tests might also be useful as part of the assessment of community patients with poor blood pressure control prior to intensifying therapy.
Conclusions
Biochemical testing for antihypertensive medication adherence appears to be feasible in terms of hypertensive patient acceptance for those attending routine appointments in primary care. Non-adherence is generally low amongst such patients and so widespread testing is not recommended where resources are limited. In such situations, GPs may wish to focus testing on patients with poor control prescribed more antihypertensive medications who may be less likely to be adherent to therapy.
Summary table
What is known on this topic
-
New methods for identifying non-adherence exist using liquid chromatography-tandem mass spectrometry (LC-MS/MS) to detect a number of medications measurable in an individual’s urine.
-
This approach has revealed high rates of previously unrecognised non-adherence to medication in hypertensive patients referred to specialist clinics in a secondary care setting.
-
It is unclear whether the medication adherence rates seen in these complex patients are representative of those in the general population presenting in primary care.
What this study adds
-
Biochemical testing for antihypertensive medication adherence is feasible in routine primary care, with two-thirds of patients able to provide a sample when approached opportunistically.
-
Amongst those participants who were able to provide a urine sample, self-reported adherence to medication did not appear to be related to biochemically determined adherence.
-
Overall, non-adherence to antihypertensive medication was very low (<5%), in contrast to previous studies using this approach, and therefore testing using LC-MS/MS is not recommended for widespread use in the community.
References
Office for National Statistics. Mid-year populations estimates: Aging, fastest increase in the ‘oldest old’. http://www.ons.gov.uk; 2010.
Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet . 2012;380:37–43.
NHS Digital. Health Survey for England 2016: Prescribed medicines. www.digital.nhs.uk: Health and Social Care Information Centre; 2017.
Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatrics. 2017;17:230
Al-Ramahi R. Adherence to medications and associated factors: a cross-sectional study among Palestinian hypertensive patients. J Epidemiol Glob Health. 2015;5:125–32.
Gupta P, Patel P, Strauch B, Lai FY, Akbarov A, Maresova V. et al. Risk factors for nonadherence to antihypertensive treatment. Hypertension. 2017;69:1113–20.
Foley L, Larkin J, Lombard-Vance R, Murphy AW, Hynes L, Galvin E. et al. Prevalence and predictors of medication non-adherence among people living with multimorbidity: a systematic review and meta-analysis. BMJ Open. 2021;11:e044987
Gehi AK, Ali S, Na B, Whooley MA. Self-reported medication adherence and cardiovascular events in patients with stable coronary heart disease: the heart and soul study. Arch Intern Med. 2007;167:1798–803.
Yang Q, Chang A, Ritchey MD, Loustalot F. Antihypertensive medication adherence and risk of cardiovascular disease among older adults: a population-based cohort study. J Am Heart Assoc. 2017;6:e006056.
Lam WY, Fresco P. Medication adherence measures: an overview. BioMed Res Int. 2015;2015:217047.
MacLaughlin EJ, Raehl CL, Treadway AK, Sterling TL, Zoller DP, Bond CA. Assessing medication adherence in the elderly: which tools to use in clinical practice?. Drugs Aging. 2005;22:231–55.
Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74.
Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47:555–67.
Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation. 2009;119:3028–35.
Gupta P, Patel P, Horne R, Buchanan H, Williams B, Tomaszewski M. How to screen for non-adherence to antihypertensive therapy. Curr Hypertens Rep. 2016;18:89.
Lane D, Patel P, Khunti K, Gupta P. Objective measures of non-adherence in cardiometabolic diseases: a review focused on urine biochemical screening. Patient Preference Adherence. 2019;13:537–47.
Tomaszewski M, White C, Patel P, Masca N, Damani R, Hepworth J. et al. High rates of non-adherence to antihypertensive treatment revealed by high-performance liquid chromatography-tandem mass spectrometry (HP LC-MS/MS) urine analysis. Heart. 2014;100:855–61.
Gupta P, Patel P, Strauch B, Lai FY, Akbarov A, Gulsin GS. et al. Biochemical screening for nonadherence is associated with blood pressure reduction and improvement in adherence. Hypertension. 2017;70:1042–8.
Burns AD, Lane D, Cole R, Patel P, Gupta P. Cardiovascular medication stability in urine for non-adherence screening by LC-MS-MS. J Anal Toxicol. 2018;43:325–9.
Walters SJ, Bonacho dos Anjos Henriques-Cadby I, Bortolami O, Flight L, Hind D, Jacques RM, et al. Recruitment and retention of participants in randomised controlled trials: a review of trials funded and published by the United Kingdom Health Technology Assessment Programme. BMJ Open. 2017;7:e015276.
Hayes P, Casey M, Glynn LG, Molloy GJ, Durand H, O’Brien E. et al. Measuring adherence to therapy in apparent treatment-resistant hypertension: a feasibility study in Irish primary care. Br J Gen Pract. 2019;69:e621–e8.
Hamdidouche I, Jullien V, Boutouyrie P, Billaud E, Azizi M, Laurent S. Drug adherence in hypertension: from methodological issues to cardiovascular outcomes. J Hypertens. 2017;35:1133−1144.
National Guideline Centre. National Institute for Health and Care Excellence. Hypertension in adults: diagnosis and management [NICE guideline 136]. London: Royal College of Physicians (UK); 2019.
Abegaz TM, Shehab A, Gebreyohannes EA, Bhagavathula AS, Elnour AA. Nonadherence to antihypertensive drugs: a systematic review and meta-analysis. Medicine. 2017;96:e5641
Durand H, Hayes P, Morrissey EC, Newell J, Casey M, Murphy AW. et al. Medication adherence among patients with apparent treatment-resistant hypertension: systematic review and meta-analysis. J Hypertens. 2017;35:2346–57.
Patel P, Gupta P, Burns A, Mohamed AA, Cole R, Lane D. et al. Biochemical urine testing of adherence to cardiovascular medications reveals high rates of nonadherence in people attending their annual review for type 2 diabetes. Diabetes Care. 2019;42:1132–5.
van Schoonhoven AV, van Asselt ADI, Tomaszewski M, Patel P, Khunti K, Gupta P. et al. Cost-utility of an objective biochemical measure to improve adherence to antihypertensive treatment. Hypertension. 2018;72:1117–24.
Acknowledgements
We would like to thank Rebecca Lowe for her help setting up the procedures for mailing urine samples from the study laboratory. We would also like to thank Hafiz Arif and his team at the University Hospitals of Leicester laboratory for managing and analysing the urine samples collected during the study. We also thank the patient representatives who advised on the study design and recruitment procedures. We thank the NIHR Clinical Research Network nurses (Claire Winch, Debbie Kelly, Diane Lonsdale, Heather Edwards, Katherine Priddis, Lydia Owen, and Sarah Wytrykowski) who recruited participants, collected samples, and extracted data from the electronic health records of participating patients. Finally, we thank Dr. Robin Fox (Bicester Health Centre), Dr. Thomas Morgan (The Boathouse Surgery), Dr. Christine A’Court (Broadshires Health Centre), Dr. Matthew Wallard (Gosford Hill Medical Centre), Dr. Nick Thomas (Windrush Medical Practice), and all of the staff at these practices and the patients who participated in the study.
Funding
This study was funded by the National Institute for Health Research (NIHR) Oxford and NIHR East Midlands Collaborations for Leadership in Applied Health Research and Care. JPS is funded by the Wellcome Trust/Royal Society via a Sir Henry Dale Fellowship (ref: 211182/Z/18/Z) and an NIHR Oxford Biomedical Research Centre (BRC) Senior Fellowship. RJMcM is an NIHR Senior Investigator. FDRH acknowledges part support from the NIHR SPCR, the NIHR CLAHRC Oxford, and the NIHR Oxford BRC. KK is supported by the National Institute for Health Research (NIHR) Applied Research Collaboration East Midlands (ARC EM) and the NIHR Leicester Biomedical Research Centre (BRC). This research was funded in part by the Wellcome Trust [Grant number 211182/Z/18/Z]. For the purpose of open access, the author has applied a CC BY public copyright licence to any Author Accepted Manuscript version arising from this submission.
Author information
Authors and Affiliations
Contributions
JPS conceived the study with PG, FDRH, RJM, and KK. AA managed the study. PG oversaw the sample analysis. JPS and AA undertook the statistical analyses. JPS wrote the first draft of the manuscript. All authors revised the manuscript and approved the final version. The corresponding author (JPS) attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sheppard, J.P., Albasri, A., Gupta, P. et al. Measuring adherence to antihypertensive medication using an objective test in older adults attending primary care: cross-sectional study. J Hum Hypertens 36, 1106–1112 (2022). https://doi.org/10.1038/s41371-021-00646-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-021-00646-w