Abstract
Objective
Metabolic and bariatric surgery (MBS) is associated with decreased bone mineral density (BMD) in adults. The long-term impact of MBS during adolescence on BMD is unknown. We report bone health status 5 to 11 years after Roux-en-Y gastric bypass (RYGB) and vertical sleeve gastrectomy (VSG) from the Teen-LABS study cohort.
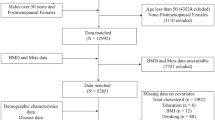
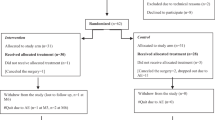
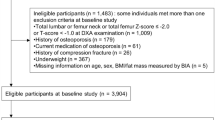
Methods
Between 2016 and 2022, BMD was measured by dual energy x-ray absorptiometry (DXA) in 106 young adults who had undergone MBS as adolescents. Volumetric BMD by peripheral quantitative computed tomography was measured on a subset. Ninety-one controls who had not undergone MBS were recruited for comparison.
Results
In cases (RYGB: mean age 26.8 ± 1.9 years, mean BMI 42.1 ± 9.9 kg/m2, VSG: mean age 25.1 ± 2.1 years, mean BMI 37.1 ± 8.4 kg/m2), compared to controls (mean age 26.5 ± 2.7 years, mean BMI 40.2 ± 8.7 kg/m2) (age p < 0.001, BMI p = 0.02), adjusted mean DXA-BMD (g/cm2) of the RYGB (n = 58) and VSG (n = 48) groups were lower at the hip (−10.0% and −6.3%), femoral neck (−9.6% and −5.7%) and ultra-distal radius (−7.9% and −7.0%; all p < 0.001), respectively. DXA-BMD did not differ between RYGB and VSG groups. Trabecular volumetric BMD at the radius and tibia were lower in the RYGB (−30% and −26%) and VSG (−15% and −14%) groups compared to the control group (p < 0.001). Greater time since MBS was associated with lower BMD Z-scores at the hip (p = 0.05) and femoral neck (p = 0.045). Percent change in body mass index (BMI) from baseline or in the first year after MBS were not associated with bone measures at a median of 9.3 years post MBS.
Conclusion
BMD, especially of the hip and femoral neck, was lower in young adults who underwent MBS during adolescence compared to matched peers who had not undergone MBS. BMD Z-scores of the femoral neck were inversely associated with time since MBS but were not associated with BMI change.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Michalsky MP, Inge TH, Jenkins TM, Xie C, Courcoulas A, Helmrath M, et al. Cardiovascular Risk Factors After Adolescent Bariatric Surgery. Pediatrics. 2018;141:e20172485.
Stanford FC, Mushannen T, Cortez P, Campoverde Reyes KJ, Lee H, Gee DW, et al. Comparison of short and long-term outcomes of metabolic and bariatric surgery in adolescents and adults. Front Endocrinol (Lausanne). 2020;11:157.
Ryder JR, Xu P, Inge TH, Xie C, Jenkins TM, Hur C, et al. Thirty-year risk of cardiovascular disease events in adolescents with severe obesity. Obesity (Silver Spring). 2020;28:616–23.
Kim J, Nimeri A, Khorgami Z, El Chaar M, Lima AG, Vosburg RW. Metabolic bone changes after bariatric surgery: 2020 update, American Society for Metabolic and Bariatric Surgery Clinical Issues Committee position statement. Surg Obes Relat Dis. 2021;17:1–8.
Beamish AJ, Harper ER, Järvholm K, Janson A, Olbers T. Long-term outcomes following adolescent metabolic and bariatric surgery. J Clin Endocrinol Metab. 2023;108:2184–92.
Casagrande DS, Repetto G, Mottin CC, Shah J, Pietrobon R, Worni M, et al. Changes in bone mineral density in women following 1-year gastric bypass surgery. Obes Surg. 2012;22:1287–92.
Yu EW, Bouxsein ML, Putman MS, Monis EL, Roy AE, Pratt JS, et al. Two-year changes in bone density after Roux-en-Y gastric bypass surgery. J Clin Endocrinol Metab. 2015;100:1452–9.
Fleischer J, Stein EM, Bessler M, Della Badia M, Restuccia N, et al. The decline in hip bone density after gastric bypass surgery is associated with extent of weight loss. J Clin Endocrinol Metab. 2008;93:3735–40.
Lindeman KG, Greenblatt LB, Rourke C, Bouxsein ML, Finkelstein JS, Yu EW. Longitudinal 5-year evaluation of bone density and microarchitecture after roux-en-y gastric bypass surgery. J Clin Endocrinol Metab. 2018;103:4104–12.
Lindeman KG, Rushin CC, Cheney MC, Bouxsein ML, Hutter MM, Yu EW. Bone density and trabecular morphology at least 10 years after gastric bypass and gastric banding. J Bone Miner Res. 2020;35:2132–42.
Reyes ML, Hernandez M, Samso C, Palma MP, Escobar R, Holmgren LJ. Quality of life assessment (PedsQL) in children at risk of disuse osteoporosis: Decreases of appendicular bone mineral density is associated to a greater body pain. Bone. 2007;40:S73–S.
Ebadinejad A, Ahmadi AR, Ghazy F, Barzin M, Khalaj A, Valizadeh M, et al. Changes in bone turnover markers after roux-en-y gastric bypass versus sleeve gastrectomy: a systematic review and meta-analysis. Obes Surg. 2023;33:1259–69.
Hofsø D, Hillestad TOW, Halvorsen E, Fatima F, Johnson LK, Lindberg M, et al. Bone mineral density and turnover after sleeve gastrectomy and gastric bypass: a randomized controlled trial (oseberg). J Clin Endocrinol Metab. 2021;106:501–11.
Raoof M, Näslund I, Rask E, Szabo E. Effect of gastric bypass on bone mineral density, parathyroid hormone and vitamin d: 5 years follow-up. Obes Surg. 2016;26:1141–5.
Ieong K, Ardila-Gatas J, Yang J, Zhang X, Tsui ST, Spaniolas K, et al. Bone mineral density changes after bariatric surgery. Surg Endosc. 2021;35:4763–70.
Sperb LF, Leotti VB, Silveiro SP, de Azevedo MJ, Viana LV. Long-term changes in bone density and bone metabolism after gastric bypass surgery: a retrospective cohort study. Obes Surg. 2023;33:911–9.
de Holanda NCP, Baad VMA, Bezerra LR, de Lima SKM, Filho JM, de Holanda Limeira CC, et al. Secondary hyperparathyroidism, bone density, and bone turnover after bariatric surgery: differences between roux-en-y gastric bypass and sleeve gastrectomy. Obes Surg. 2021;31:5367–75.
Paccou J, Tsourdi E, Meier C, Palermo A, Pepe J, Body JJ, et al. Bariatric surgery and skeletal health: A narrative review and position statement for management by the European Calcified Tissue Society (ECTS). Bone. 2022;154:116236.
Rousseau C, Jean S, Gamache P, Lebel S, Mac-Way F, Biertho L, et al. Change in fracture risk and fracture pattern after bariatric surgery: nested case-control study. BMJ. 2016;354:i3794.
Yu EW, Lee MP, Landon JE, Lindeman KG, Kim SC. Fracture risk after bariatric surgery: Roux-en-Y gastric bypass versus adjustable gastric banding. J Bone Miner Res. 2017;32:1229–36.
Robinson DE, Douglas I, Tan GD, Delmestri A, Judge A, Cooper C, et al. Bariatric surgery increases the rate of major fracture: self-controlled case series study in UK Clinical Practice Research Datalink. J Bone Miner Res. 2021;36:2153–61.
Khalid SI, Omotosho PA, Spagnoli A, Torquati A. Association of bariatric surgery with risk of fracture in patients with severe obesity. JAMA Netw Open. 2020;3:e207419.
Ahlin S, Peltonen M, Sjöholm K, Anveden Å, Jacobson P, Andersson-Assarsson JC, et al. Fracture risk after three bariatric surgery procedures in Swedish obese subjects: up to 26 years follow-up of a controlled intervention study. J Intern Med. 2020;287:546–57.
Kaulfers AM, Bean JA, Inge TH, Dolan LM, Kalkwarf HJ. Bone loss in adolescents after bariatric surgery. Pediatrics. 2011;127:e956–61.
Beamish AJ, Gronowitz E, Olbers T, Flodmark CE, Marcus C, Dahlgren J. Body composition and bone health in adolescents after Roux-en-Y gastric bypass for severe obesity. Pediatr Obes. 2017;12:239–46.
Järvholm K, Janson A, Peltonen M, Neovius M, Gronowitz E, Engström M, et al. Metabolic and bariatric surgery versus intensive non-surgical treatment for adolescents with severe obesity (AMOS2): a multicentre, randomised, controlled trial in Sweden. Lancet Child Adolesc Health. 2023;7:249–60.
Misra M, Singhal V, Carmine B, Bose A, Kelsey MM, Stanford FC, et al. Bone outcomes following sleeve gastrectomy in adolescents and young adults with obesity versus non-surgical controls. Bone. 2020;134:115290.
Mitchell DM, Singhal V, Animashaun A, Bose A, Carmine B, Stanford FC, et al. Skeletal effects of sleeve gastrectomy in adolescents and young adults: a 2-year longitudinal study. J Clin Endocrinol Metab. 2023;108:847–57.
Nimmala S, Kaur S, Singhal V, Mitchell DM, Stanford FC, Bouxsein ML, et al. Changes in sex steroids and enteric peptides after sleeve gastrectomy in youth in relation to changes in bone parameters. J Clin Endocrinol Metab. 2022;107:e3747–e58.
Xanthakos SA, Khoury JC, Inge TH, Jenkins TM, Modi AC, Michalsky MP, et al. Nutritional risks in adolescents after bariatric surgery. Clin Gastroenterol Hepatol. 2020;18:1070–81.e5.
Inge TH, Courcoulas AP, Jenkins TM, Michalsky MP, Helmrath MA, Brandt ML, et al. Weight loss and health status 3 years after bariatric surgery in adolescents. N Engl J Med. 2016;374:113–23.
Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95.
Wadhwa R, Kumar M, Talegaonkar S, Vohora D. Serotonin reuptake inhibitors and bone health: A review of clinical studies and plausible mechanisms. Osteoporos Sarcopenia. 2017;3:75–81.
Lespessailles E, Toumi H. Proton Pump Inhibitors and Bone Health: An Update Narrative Review. Int J Mol Sci. 2022;23:10733.
Monadi M, Javadian Y, Cheraghi M, Heidari B, Amiri M. Impact of treatment with inhaled corticosteroids on bone mineral density of patients with asthma: related with age. Osteoporos Int. 2015;26:2013–8.
Tian Z, Fan X-T, Li S-Z, Zhai T, Dong J. Changes in bone metabolism after sleeve gastrectomy versus gastric bypass: a meta-analysis. Obes Surg. 2020;30:77–86.
Chaves Pereira de Holanda N, de Lima Carlos I, Chaves de Holanda Limeira C, Cesarino de Sousa D, Serra de Lima Junior FA, Telis de Vilela Araújo A, et al. Fracture risk after bariatric surgery: a systematic literature review and meta-analysis. Endocr Pract. 2022;28:58–69.
Saad RK, Ghezzawi M, Habli D, Alami RS, Chakhtoura M. Fracture risk following bariatric surgery: a systematic review and meta-analysis. Osteoporos Int. 2022;33:511–26.
Wren TA, Shepherd JA, Kalkwarf HJ, Zemel BS, Lappe JM, Oberfield S, et al. Racial disparity in fracture risk between white and nonwhite children in the United States. J Pediatr. 2012;161:1035–40.
Stattin K, Höijer J, Hållmarker U, Baron JA, Larsson SC, Wolk A, et al. Fracture risk across a wide range of physical activity levels, from sedentary individuals to elite athletes. Bone. 2021;153:116128.
Vandewalle S, Taes Y, Van Helvoirt M, Debode P, Herregods N, Ernst C, et al. Bone size and bone strength are increased in obese male adolescents. J Clin Endocrinol Metab. 2013;98:3019–28.
Leonard MB, Zemel BS, Wrotniak BH, Klieger SB, Shults J, Stallings VA, et al. Tibia and radius bone geometry and volumetric density in obese compared to non-obese adolescents. Bone. 2015;73:69–76.
Yu EW, Bouxsein ML, Roy AE, Baldwin C, Cange A, Neer RM, et al. Bone loss after bariatric surgery: discordant results between DXA and QCT bone density. J Bone Miner Res. 2014;29:542–50.
Hernández-Martínez A, Veras L, Boppre G, Soriano-Maldonado A, Oliveira J, Diniz-Sousa F, et al. Changes in volumetric bone mineral density and bone quality after Roux-en-Y gastric bypass: A meta-analysis with meta-regression. Obes Rev. 2022;23:e13479.
Huber FA, Singhal V, Tuli S, Becetti I, Lopez Lopez AP, Bouxsein ML, et al. Two-year Skeletal Effects of Sleeve Gastrectomy in Adolescents with Obesity Assessed with Quantitative CT and MR Spectroscopy. Radiology. 2023;307:e223256.
Evans EM, Mojtahedi MC, Kessinger RB, Misic MM. Simulated change in body fatness affects Hologic QDR 4500A whole body and central DXA bone measures. J Clin Densitom. 2006;9:315–22.
Jain RK, Vokes T. Visceral adipose tissue is negatively associated with bone mineral density in NHANES 2011-2018. J Endocr Soc. 2023;7:bvad008.
Russell M, Mendes N, Miller KK, Rosen CJ, Lee H, Klibanski A, et al. Visceral fat is a negative predictor of bone density measures in obese adolescent girls. J Clin Endocrinol Metab. 2010;95:1247–55.
Gállego Suárez C, Singer BH, Gebremariam A, Lee JM, Singer K. The relationship between adiposity and bone density in U.S. children and adolescents. PLoS One. 2017;12:e0181587.
Silva BC, Bilezikian JP. Parathyroid hormone: anabolic and catabolic actions on the skeleton. Curr Opin Pharmacol. 2015;22:41–50.
Pratt JSA, Browne A, Browne NT, Bruzoni M, Cohen M, Desai A, et al. ASMBS pediatric metabolic and bariatric surgery guidelines, 2018. Surg Obes Relat Dis. 2018;14:882–901.
Acknowledgements
The authors gratefully acknowledge the commitment of the participants in the Teen-LABS study and study personnel.
Funding
This study was conducted as a cooperative agreement and funded by the National Institute of Diabetes and Digestive and Kidney Diseases (U01 DK072493, UM1 DK072493 and UM1 DK095710). The research was also supported in part by the National Center for Advancing Translational Sciences of the National Institutes of Health (Award Number UL1 TR001425). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
Halley Wasserman, MD, MS was involved in the study design, review of the DXA and pQCT scans, interpretation of the results, drafting and revising this manuscript and approval of the submitted manuscript. Todd Jenkins was responsible for the statistical analysis and creation of the tables and figures. He helped obtain funding for this work. He was involved in revising this manuscript and approval of the submitted manuscript. Thomas Inge was involved in obtaining funding for this work, study design, interpretation of results, revising this manuscript and approval of the submitted manuscript. Justin Ryder, PhD was involved in the study design, interpretation of results, revising this manuscript and approval of the submitted manuscript. Marc Michalsky, MD, MBA was involved in the data collection, interpretation of results, revising this manuscript and approval of the submitted manuscript. Stephanie Sisley, MD was involved in data collection, interpretation of results, revising this manuscript and approval of the submitted manuscript. Changchun Xie, PhD was involved in the interpretation of results, revising this manuscript and approval of the submitted manuscript. Heidi J. Kalkwarf, PhD was involved in the study design, review of DXA and pQCT scans, data analysis, interpretation of results, drafting and revising this manuscript and approval of the submitted manuscript.
Corresponding author
Ethics declarations
Competing interests
HW – Nothing to disclose. TJ – Nothing to disclose. TI – Consultant for Mediflix and receives author royalties from Wolters Kluwer for UpToDate chapter contribution. JR – Receives a donation of drug and placebo for a clinical trial from Boehringer Ingelheim. MM – Intuitive Surgical, Inc (educational honorarium), Intuitive Surgical, Inc (stock ownership – relationship terminated), Lilly USA, LLC (Pediatric Obesity Advisory Board ad hoc member). SS – Consultant for Rhythm Pharmaceuticals. CX – Nothing to disclose. HJK - Nothing to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wasserman, H., Jenkins, T., Inge, T. et al. Bone mineral density in young adults 5 to 11 years after adolescent metabolic and bariatric surgery for severe obesity compared to peers. Int J Obes 48, 575–583 (2024). https://doi.org/10.1038/s41366-023-01453-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-023-01453-8