Abstract
Background:
Critically ill children are prone to nosocomial infections, which may lead to adverse outcome. Low serum concentrations upon admission to the pediatric intensive care unit (PICU) of the mannan-binding lectin (MBL)-associated serine protease (MASP)-3 protein of the lectin pathway of complement activation have been associated with risk of infection and prolonged need for intensive care. We hypothesized that also a low upon-admission concentration of collectin-L1 (CL-L1), a novel member of this pathway, is independently associated with these adverse outcomes.
Methods:
We quantified the serum concentrations of CL-L1 in 81 healthy children and in 700 critically ill children upon PICU admission.
Results:
CL-L1 concentrations were significantly lower in the critically ill children as compared with the healthy children. However, corrected for baseline characteristics, risk factors and several lectin pathway proteins, a higher CL-L1 concentration upon PICU admission was independently associated with an increased risk of acquiring a new infection and with a prolonged time to PICU discharge. In contrast, a low MASP-3 concentration remained independently associated with these adverse outcomes.
Conclusion:
A high serum CL-L1 concentration in critically ill children upon PICU admission is associated with an increased risk of infection and prolonged need of intensive care, and counteracts the protective effect of having a high MASP-3 concentration.
Similar content being viewed by others
Main
Critically ill children are particularly vulnerable to potentially life-threatening nosocomial infections. Indeed, secondary infections of diverse origins have been reported to occur in approximately 30% of the patients (1). The innate immune system is an ancient, conserved defense mechanism, which provides the immediate response that is of paramount importance for the protection against invading pathogens as well as for the repair of tissue damage (2). The complement system, which consists of soluble proteins acting as pattern recognition receptors, proenzymes, cell surface complement receptors, and regulatory proteins, is an essential part of innate immunity (3). The complement system is important for fighting infections, for clearing immune complexes and cellular waste, and for linking innate to adaptive immunity. Insufficient as well as excessive activation of this system can be detrimental, and thus, health depends on a subtle balance (4). Defects in components of the inflammatory complement system have been linked to increased susceptibility to infections in young children with associated pathologies (5,6). Also, depletion of complement factors has been shown to be associated with adverse outcome in abdominal sepsis (7,8). On the other hand, excessive inflammation, induced by trauma or infection, has also been linked to worsening of organ function and shock (9,10).
The complement system is redundant and may be activated in different ways. One way is via the so-called lectin pathway, which recognizes patterns of foreign carbohydrate structures (e.g., on pathogens). This pathway may be initiated by different pattern recognition molecules, including mannan-binding lectin (MBL), one of the ficolins (H-, M-, and L-ficolin) and the collectins (11,12). This pathway also exhibits the duality of the system, as both insufficient and excessive activation may be detrimental. For example, an increased susceptibility to secondary infections or complications was shown with deficiency in MBL or ficolins in children with cancer and in neonates with necrotizing enterocolitis (6,13,14). In contrast, increased levels of these innate immunity proteins, which could possibly be explained by genetic polymorphism, may contribute to exaggerated inflammatory responses as seen in the acute respiratory distress syndrome (15,16). Overall, data on the lectin pathway of complement activation in critically ill children are scarce.
We previously studied MBL, M- and H-ficolin, and their MBL-associated serine proteases (MASPs) in a large group of critically ill children (17). Serum concentrations of these proteins were lower in critically ill children upon admission to the pediatric intensive care unit (PICU) as compared with age-matched healthy controls, except for higher concentrations of M-ficolin. In particular, a low MASP-3 level upon admission was independently associated with the risk of acquiring a new infection and with the risk of needing prolonged intensive care.
Within the last 15 y, a novel group of pattern recognition molecules has been discovered, which includes collectin-L1 (CL-L1, also named collectin-10) in addition to CL-K1 (also named collectin-11) and CL-P1 (12,18,19,20,21). So far, very little is known about the biological function of this class of collectins. CL-L1 in particular has been shown to activate complement (22). Elevated circulating CL-L1 concentrations have been observed in the early phase of acute liver failure and in cirrhosis (23). Also, evaluation of CL-L1 as a screening marker for colorectal cancer showed that higher levels of CL-L1 were associated with lower odds of colorectal cancer (24).
As the collectins have been shown to bind to different microorganisms and altered/exposed structures in the body (25), this new group of collections may also play a role in inflammatory conditions. In this study, we quantified serum concentrations of CL-L1 in children admitted to the pediatric intensive care unit (PICU), in comparison with those of healthy children, and explored the potential association with baseline characteristics and clinical outcomes of the critically ill children. We focused on the risk of acquiring a new infection and prolonged need for intensive care in view of the association we previously observed for low MASP-3 levels with these outcomes. We thus hypothesized that low levels of CL-L1 upon PICU admission, possibly induced by surgical, traumatic, or other stress, are associated with a higher risk of acquiring a new infection and with a prolonged need for intensive care.
Results
Serum Concentrations of CL-L1 in Critically Ill Children and in Healthy Children
In propensity-matched cohorts of 81 critically ill and 81 healthy children, serum concentrations of CL-L1 were significantly lower in the critically ill children as compared with the healthy children (452 (372–541) ng/ml vs. 561 (518–601) ng/ml, (median (interquartile range (IQR))), P < 0.0001). The CL-L1 concentration in the propensity score-matched critically ill children did not differ from that in the nonmatched children (466 (379–564) ng/ml, P = 0.51). In the total group of critically ill children, the median CL-L1 serum concentration upon PICU admission was 466 (378–562) ng/ml. The CL-L1 concentration increased gradually during ICU stay to levels comparable with those in the healthy children ( Figure 1 ).
CL-L1 serum concentrations during critical illness. Time profiles of serum concentrations of CL-L1 are shown for 40 critically ill children, with CL-L1 concentrations measured upon pediatric intensive care unit (PICU) admission (adm), day 2 (D2), day 4 (D4), day 8 (D8), and last day in PICU. Data are expressed as box plots, where the central lines indicate the medians, the boxes represent the interquartile ranges, and the whiskers represent the 10th and 90th percentiles.
CL-L1 Serum Concentrations Upon PICU Admission in Relation to Baseline Characteristics
CL-L1 serum concentrations did not differ according to age, BMI, or medical history of diabetes or malignancy (data not shown). Cardiac surgery patients presented with higher baseline CL-L1 levels than patients admitted to the PICU for any other reason (469 (386–567) ng/ml in cardiac patients vs. 441 (351–528) ng/ml in noncardiac patients, P = 0.02). CL-L1 concentrations upon PICU admission weakly correlated inversely with severity of illness, as evaluated by modified PRISM score (ρ = −0.200, P < 0.0001), PELOD score (ρ = −0.106, P = 0.006), or baseline concentrations of glucose (ρ = −0.137, P = 0.0004), lactate (ρ = −0.257, P < 0.0001), troponin (ρ = −0.152, P = 0.004) or heart-type fatty acid binding protein (HFABP, ρ = −0.317, P < 0.0001). CL-L1 concentrations correlated directly with the concentrations of the other lectin pathway proteins (MBL, MASP-1, MASP-2, MASP-3, MAp44, M- and H-ficolin (17)) ( Table 1 ), and inversely with C-reactive protein (CRP) (ρ = −0.136, P = 0.0006). The correlation was particularly strong for MASP-1, MASP-3, and MAp44, which are three alternative splice products encoded by the same gene, MASP1.
Association of CL-L1 Serum Concentrations Upon PICU Admission With Outcome of Critical Illness
In a multivariable logistic regression analysis, correcting for baseline characteristics, risk factors, and the other lectin pathway proteins, a higher CL-L1 concentration upon PICU admission was independently associated with an increased risk of acquiring a new infection (odds ratio (OR): 1.241 (95% confidence interval (CI): 1.031–1.494), P = 0.02) ( Table 2 ). A low MASP-3 concentration upon PICU admission was independently associated with a higher risk of infection in this model (OR: 0.701 (95% CI: 0.562–0.864), P = 0.001). This confirmed the association we previously observed for MASP-3, with an even lower odds ratio than in the model without CL-L1 (OR: 0.809 (95% CI: 0.675–0.959), P = 0.02) (17). The independent associations of CL-L1 and MASP-3 with infection were maintained with the addition of the interaction between both protein concentrations to the model, with a P value of 0.06 for the interaction variable ( Table 2 ).
In multivariable Cox proportional hazard analysis, correcting for baseline characteristics, risk factors, and the other lectin pathway proteins, a high CL-L1 concentration tended to be associated with a prolonged time to PICU discharge (P = 0.05, Table 3 ). The hazard ratio of 0.933 (95% CI: 0.867–1.002) indicated a lower likelihood of earlier alive discharge at any time with a higher CL-L1 concentration upon PICU admission. As for risk of infection, this association was in the opposite direction as that for MASP-3, showing a higher likelihood of earlier alive discharge at any time with a higher MASP-3 concentration (hazard ratio (HR) of 1.125 (95% CI: 1.046–1.205, P = 0.001). Again, this association was stronger than for the model without CL-L1 that was previously reported (HR: 1.088 (95% CI: 1.020–1.157), P = 0.01) (17). Addition of the interaction between both proteins had no major effect, with a P value of 0.92 for the interaction variable ( Table 3 ).
Discussion
In a large cohort of critically ill children, serum concentrations of CL-L1 upon PICU admission appeared to be lower than in age-, gender-, and BMI-matched healthy controls. Corrected for baseline characteristics, risk factors, and the other lectin pathway proteins, a higher CL-L1 concentration was associated with a higher risk of acquiring a new infection and with risk of a prolonged need for intensive care. The previously observed association of a low MASP-3 with a higher risk of these adverse outcomes was robustly maintained and became even stronger in this model with CL-L1.
To date, there is only very limited knowledge on the biological function of the pattern recognition molecule CL-L1. CL-L1 is encoded by the COLEC10 gene and is primarily expressed in the liver, placenta, and adrenal glands (18). Initially, CL-L1 was identified as a cytosolic protein but has now been found in the circulation, where it complexes with MBL-associated serine proteases (MASPs), the enzymes responsible for activation of complement through the lectin pathway (21,22,26). In healthy individuals, CL-L1 levels appear to be present at near adult levels at birth and show low variation (22). The few occurring fluctuations may have reflected periods of microbial challenge. The authors suggested that CL-L1 may have an important role during the first year of life, when other elements of the immune system are immature. After major surgery, a modest downregulation of CL-L1 was observed that coincided with the CRP response (22). This is in agreement with the acute decrease in serum concentrations of CL-L1 that we observed in response to the severe stress of critical illness in children and correlated, although weakly, with the rise in CRP. The drop in CL-L1 in the critically ill children was more pronounced with increasing severity of illness.
We performed multivariable analyses to assess whether the upon PICU admission serum concentration of CL-L1 is associated with risk of infection and prolonged need of intensive care. We corrected for the classical baseline characteristics and risk factors. However, the innate immune system is an extremely complex system of intertwined pathways, whose adequate function depends on a very subtle balance. An extraordinary redundancy of most of the system components may mask a deficiency or malfunctioning of an individual component. Moreover, several components display context specific properties, where they can act as dual function surveillance molecules, suppressing or enhancing inflammation, as, e.g., shown for the lung collectins (27,28). Therefore, we also corrected for the other lectin pathway proteins for which the concentrations upon PICU admission had been measured (17). These analyses revealed independent associations with infection and ICU stay for both CL-L1 and MASP-3. Intriguingly, these associations were in the opposite direction, despite both proteins being reduced in concentration upon PICU admission and a relatively strong correlation between both proteins. For CL-L1, a high concentration was associated with new infection and prolonged PICU stay, whereas for MASP-3, a low concentration was predictive for these adverse outcomes. This suggests that in the context of a sufficiently high MASP-3 concentration, having a high concentration of CL-L1 would be detrimental as it counteracts the protective effect of having a high MASP-3. This opposition by CL-L1 is further supported by the lower odds ratio for risk of infection and higher hazard ratio for time to alive discharge from PICU for MASP-3 when CL-L1 is entered in the model. Our analyses were not confounded by correlation between the variables in the model, as multicollinearity was carefully excluded. The two-sided nature of circulating CL-L1 in critical illness, being reduced as compared with healthy controls but higher concentrations being associated with infection and prolonged PICU stay, is intriguing. Unfortunately, lack of knowledge about the biological function of CL-L1 hampers speculation about the mechanisms that are involved. Clearly, basic scientific research will be needed to unravel the mechanistic processes that may underlie our observations. Also, the immediate clinical relevance of the present findings is currently unclear. However, the data nicely illustrate the complex dualism of the inflammatory cascade, where apparently opposite forces are actually complementary and regulated in a subtle balance. This insight may contribute to a future of personalized medicine, where (a panel of) biomarkers may guide therapy toward enhancing inflammation (in case of infection) or suppressing inflammation (when excessive inflammation threatens organ function).
A major strength of the present findings is that we studied a large, heterogeneous population of (critically ill) children, which is quite unique. Indeed, most often clinical studies in ICU exclude children, as they represent only a small population spread over different developmental stages, and results obtained from adult studies are too often extrapolated to children. Nevertheless, a limitation of our study is that we only showed associations, with no evidence of causality. Secondly, the measurements we performed are primarily of hetero-oligomers between CL-L1 and CL-K1 polypeptide chains, two collectins that have most likely evolved from the same ancestral gene by gene duplication (21,26,29). We have observed that there is a tight correlation between the amount of CL-L1 and CL-K1 in plasma but no one has studied in detail whether both molecules can be present separately at different sites in the body and whether such proteins appear in plasma at extreme conditions (24,26,29,30).
In conclusion, corrected for baseline characteristics, risk factors, and several lectin pathway proteins, a high serum CL-L1 concentration upon PICU admission is associated with an increased risk of infection and prolonged need of intensive care, and counteracts the protective effect on these outcomes of having a high MASP-3 concentration. More pathophysiological research will, however, be needed to further elucidate the role of CL-L1 during critical illness and during infection in particular. Nevertheless, the present findings yield valuable and unique information, which can incite further exploration in this relatively new, though expanding field of research.
Methods
Subjects
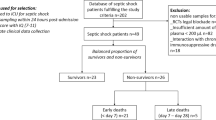
This study is a preplanned analysis of all patients (n = 700) included in a randomized controlled study on tight glycemic control in the PICU (1). The majority of the children were admitted to the PICU after cardiac surgery for congenital heart defects (75%), whereas the others were admitted after complicated surgery or trauma, after solid organ transplant surgery, or after neurological, infectious, or other medical disorders. Critically ill children were allocated upon PICU admission to either conventional insulin therapy (n = 351, insulin was started only when the blood glucose concentration exceeded 215 mg/dl and was tapered down or stopped when glycemia fell below 180 mg/dl), or intensive insulin therapy (IIT, n = 349, insulin was infused to achieve age-adjusted normal fasting glucose levels). Both randomization groups were comparable for baseline characteristics (1). The characteristics of the total patient cohort are shown in Table 4 . In addition, we included 81 healthy children ( Table 4 ), who were scheduled for minor ambulatory surgery. Blood was withdrawn preoperatively after catheterization that was required for induction and/or maintenance of anesthesia. These children were propensity score-matched with critically ill children (vide infra) to study the impact of critical illness. The study was approved by the KU Leuven Institutional Review Board (ML2586) and was registered with ClinicalTrials.gov (NCT00214916). The study was performed in accordance with the 1964 Declaration of Helsinki and its amendments. Written informed consent was obtained from the parents or legal guardians of patients and controls.
Blood Sampling and Biochemical Analyses
Upon PICU admission, serum was collected and stored at −80 °C until analysis. For 29 patients, no baseline serum sample was available. For 40 patients, 20 per randomization group (with comparable baseline characteristics, data not shown), additional serum samples collected on day 2, day 4, day 8 (if the patient was still in ICU on those days), and last day, in PICU, were used to study the time profile of CL-L1 during critical illness.
CRP was determined by routine clinical chemistry. Whole arterial blood glucose was measured at 1–4 h intervals during ICU stay using the ABL700 blood gas analyzer (Radiometer Medical A/S, Copenhagen, Denmark). CL-L1 concentrations were measured in duplicate using an in-house time-resolved immune-fluorometric assay (TRIFMA) with a setup similar to conventional sandwich immune assays (22). However, we used a new and better characterized preparation of recombinant CL-L1, resulting in healthy control levels approximately three times lower than given in our original report (22). In brief, capture of the protein with anti-CL-L1 and detection of bound CL-L1 with biotinylated anti-CL-L1, was followed by incubation with Eu3+-labeled streptavidin. After washing, the europium bound in the wells was quantified after addition of enhancement solution to the wells, and the fluorescence was read using time-resolved fluorometry. Data were analyzed using the WorkOut 2 software (PerkinElmer Life Sciences, Waltham, Massachusetts, USA). In addition to a standard curve, consisting of serial dilutions of plasma, three internal control plasma samples (representing a high, medium, and low concentration of the protein) and a buffer control were included on each microtiter plate. All samples were analyzed in duplicate and the analysis was repeated if the coefficient of variation was higher than 20%. The plate was repeated if the quality controls varied with a CV above 15% as compared with a collection of previously measured values. If the concentration of the samples exceeded the highest value of the standard curve, the assays were repeated at higher dilution.
Statistical Analyses
Data were analyzed with JMP Pro 11.2.0 (SAS Institute, Cary, NC). Two-sided P values below 0.05 were considered significant. Data are presented as mean (95% CI), median (IQR), or proportion (percentage), as appropriate. Continuous variables were analyzed with the Wilcoxon test, and proportions with the chi-square test. Associations between variables were calculated with Spearman’s correlation coefficient. To evaluate the association of CL-L1 serum concentrations upon PICU admission with risk of infection, independent of known risk factors, multivariable logistic regression analysis was performed. The classical baseline characteristics and risk factors (age, gender, BMI, randomization, CRP, history of malignancy, cardiac surgery, modified pediatric risk of mortality (PRISM) score) were considered, and in view of the potential context-specificity of disturbances in this system, (27,28), also, the upon-admission concentrations of the other lectin pathway proteins (measured in ref. (17)) were added. In a second step, the interaction between CL-L1 and MASP-3 concentrations was tested, in which the addition of the CL-L1 * MASP-3 interaction variable to the model assesses whether the effect of CL-L1 on risk of infection is different at different values of MASP-3. To evaluate the predictive power for likelihood to early alive discharge from PICU, Cox proportional hazard analysis was performed entering the same risk factors, with nonsurvivors censored beyond the longest staying survivor, ensuring the most stringent analysis avoiding competing risk between death and earlier discharge (31). We excluded multicollinearity of the variables entered in the models via the collinearity diagnostics tool in SPSS version 22.0 (32).
We used propensity-score matching of the SPSS R-menu (Version R2.10.1, R Foundation for Statistical Computing) in IBM SPSS Statistics 19 (SPSS, Chicago, IL) to select demographically comparable cohorts of healthy and critically ill children (33,34). Propensity-scores were estimated via logistic regression with age, gender, and BMI as continuous covariates. One-to-one nearest neighbor matching was performed with the use of a caliper of 0.004.
Statement of Financial Support
This work was supported by the TBM program (Toegepast Biomedisch onderzoek met een primair Maatschappelijke finaliteit) of the Institute for Science and Technology, Flanders, Belgium (IWT 070695). C.I. received a Clinical PhD Fellowship of the Research Foundation – Flanders (FWO). S.T. was supported by The Danish Council for Independent Research, Medical Sciences and the Novo Nordisk Foundation. G.Vd.B. was supported by the University of Leuven, receives long-term structural research financing via the Methusalem program, funded by the Flemish Government, and holds an “ERC Advanced Grant” from the Ideas Program of the European Union FP7.
Disclosure
The authors declare that they do not have any financial relationships relevant to this article, nor any conflict of interest, to disclose.
References
Vlasselaers D, Milants I, Desmet L, et al. Intensive insulin therapy for patients in paediatric intensive care: a prospective, randomised controlled study. Lancet 2009;373:547–56.
Janeway CA Jr, Medzhitov R. Innate immune recognition. Annu Rev Immunol 2002;20:197–216.
Holers VM. Complement and its receptors: new insights into human disease. Annu Rev Immunol 2014;32:433–59.
Ricklin D, Lambris JD. Complement in immune and inflammatory disorders: pathophysiological mechanisms. J Immunol 2013;190:3831–8.
Ip WK, Takahashi K, Ezekowitz RA, Stuart LM. Mannose-binding lectin and innate immunity. Immunol Rev 2009;230:9–21.
Neth O, Hann I, Turner MW, Klein NJ. Deficiency of mannose-binding lectin and burden of infection in children with malignancy: a prospective study. Lancet 2001;358:614–8.
Yuan Y, Yan D, Han G, Gu G, Ren J. Complement C3 depletion links to the expansion of regulatory T cells and compromises T-cell immunity in human abdominal sepsis: a prospective pilot study. J Crit Care 2013;28:1032–8.
Ren J, Zhao Y, Yuan Y, et al. Complement depletion deteriorates clinical outcomes of severe abdominal sepsis: a conspirator of infection and coagulopathy in crime? PLoS One 2012;7:e47095.
Rittirsch D, Redl H, Huber-Lang M. Role of complement in multiorgan failure. Clin Dev Immunol 2012;2012:962927.
Charchaflieh J, Wei J, Labaze G, et al. The role of complement system in septic shock. Clin Dev Immunol 2012;2012:407324.
Degn SE, Thiel S. Humoral pattern recognition and the complement system. Scand J Immunol 2013;78:181–93.
Ohtani K, Suzuki Y, Wakamiya N. Biological functions of the novel collectins CL-L1, CL-K1, and CL-P1. J Biomed Biotechnol 2012;2012:493945.
Schlapbach LJ, Aebi C, Hansen AG, Hirt A, Jensenius JC, Ammann RA. H-ficolin serum concentration and susceptibility to fever and neutropenia in paediatric cancer patients. Clin Exp Immunol 2009;157:83–9.
Schlapbach LJ, Kessler U, Thiel S, et al. M-ficolin in the neonatal period: Associations with need for mechanical ventilation and mortality in premature infants with necrotising enterocolitis. Mol Immunol 2009;46:2597–603.
Vollmer-Conna U, Piraino BF, Cameron B, et al.; Dubbo Infection Outcomes Study Group. Cytokine polymorphisms have a synergistic effect on severity of the acute sickness response to infection. Clin Infect Dis 2008;47:1418–25.
Gao L, Barnes KC. Recent advances in genetic predisposition to clinical acute lung injury. Am J Physiol Lung Cell Mol Physiol 2009;296:L713–25.
Ingels C, Vanhorebeek I, Steffensen R, et al. Lectin pathway of complement activation and relation with clinical complications in critically ill children. Pediatr Res 2014;75:99–108.
Ohtani K, Suzuki Y, Eda S, et al. Molecular cloning of a novel human collectin from liver (CL-L1). J Biol Chem 1999;274:13681–9.
Keshi H, Sakamoto T, Kawai T, et al. Identification and characterization of a novel human collectin CL-K1. Microbiol Immunol 2006;50:1001–13.
Ohtani K, Suzuki Y, Eda S, et al. The membrane-type collectin CL-P1 is a scavenger receptor on vascular endothelial cells. J Biol Chem 2001;276:44222–8.
Selman L, Hansen S. Structure and function of collectin liver 1 (CL-L1) and collectin 11 (CL-11, CL-K1). Immunobiology 2012;217:851–63.
Axelgaard E, Jensen L, Dyrlund TF, et al. Investigations on collectin liver 1. J Biol Chem 2013;288:23407–20.
Laursen TL, Sandahl TD, Støy S, et al.; US Acute Liver Failure Study Group. Circulating mannan-binding lectin, M-, L-, H-ficolin and collectin-liver-1 levels in patients with acute liver failure. Liver Int 2015;35:756–63.
Storm L, Christensen IJ, Jensenius JC, Nielsen HJ, Thiel S ; Danish Study Group on Early Detection of Colorectal Cancer. Evaluation of complement proteins as screening markers for colorectal cancer. Cancer Immunol Immunother 2015;64:41–50.
Troegeler A, Lugo-Villarino G, Hansen S, et al. Collectin CL-LK Is a Novel Soluble Pattern Recognition Receptor for Mycobacterium tuberculosis. PLoS One 2015;10:e0132692.
Henriksen ML, Brandt J, Andrieu JP, et al. Heteromeric complexes of native collectin kidney 1 and collectin liver 1 are found in the circulation with MASPs and activate the complement system. J Immunol 2013;191:6117–27.
Keizer MP, Wouters D, Schlapbach LJ, Kuijpers TW. Restoration of MBL-deficiency: redefining the safety, efficacy and viability of MBL-substitution therapy. Mol Immunol 2014;61:174–84.
Gardai SJ, Xiao YQ, Dickinson M, et al. By binding SIRPalpha or calreticulin/CD91, lung collectins act as dual function surveillance molecules to suppress or enhance inflammation. Cell 2003;115:13–23.
Bayarri-Olmos R, Hansen S, Henriksen ML, et al. Genetic variation of COLEC10 and COLEC11 and association with serum levels of collectin liver 1 (CL-L1) and collectin kidney 1 (CL-K1). PLoS One 2015;10:e0114883.
Troldborg A, Thiel S, Jensen L, et al. CL-L1 and CL-K1 and other complement associated pattern recognition molecules in systemic lupus erythematosus. Clin Exp Immunol 2015;182:132–8.
Casaer MP, Mesotten D, Hermans G, et al. Early versus late parenteral nutrition in critically ill adults. N Engl J Med 2011;365:506–17.
Midi H, Sarkar S K, Rana S. Collinearity diagnostics of binary logistic regression model. Journal of Interdisciplinary Mathematics 2010;13:3, 253–267.
Heinze G, Jüni P. An overview of the objectives of and the approaches to propensity score analyses. Eur Heart J 2011;32:1704–8.
Thoemmes F. Propensity score matching in SPSS. ArXiv: 1201.6385 [online], 2012. (https://arxiv.org/ftp/arxiv/papers/1201/1201.6385.pdf).
Acknowledgements
We thank the pediatric ICU clinical and nursing staff for excellent patient care, protocol compliance, and sample handling.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ingels, C., Vanhorebeek, I., Derese, I. et al. The pattern recognition molecule collectin-L1 in critically ill children. Pediatr Res 80, 237–243 (2016). https://doi.org/10.1038/pr.2016.76
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2016.76