Abstract
Cerebral development may be impaired in fetuses with congenital cardiovascular malformations, particularly hypoplastic left heart syndrome (HLHS) and aortopulmonary transposition (APT). The decreased cerebral arterial pusatility index observed in some of these fetuses led to the belief that cerebral vascular resistance was reduced as a result of arterial hypoxemia and cerebral hypoxia is thought to be responsible for impaired cerebral growth. However, other hemodynamic factors could affect pulsatility index. I propose that cerebral blood flow is reduced in fetuses with HLHS and that reduced glucose, rather than oxygen, delivery interferes with cerebral development. This is based on the fact that most of these fetuses do not have lactate accumulation in the brain.
In fetuses with APT, umbilical venous blood, containing oxygen and glucose derived across the placenta, is distributed to the lungs and lower body; venous blood, with low oxygen and glucose content, is delivered to the ascending aorta and brain. Oxygen and glucose delivery may further be reduced by decreased cerebral blood flow resulting from run-off of aortic blood through the ductus arteriosus to the pulmonary circulation during diastole. In APT fetuses, lack of lactate in the brain also supports my proposal that glucose deficiency interferes with cerebral development.
Similar content being viewed by others
Main
Increased frequency of neurodevelopmental disabilities has been noted in children born with congenital cardiovascular malformations. It had been attributed to cerebral damage resulting from cardiac failure or hypoxemia during the neonatal period, or following complicated surgical procedures (1,2,3). Recently, it has been recognized that abnormalities in cerebral development may occur before birth in association with congenital cardiovascular malformations.
Unfortunately, most studies have grouped a variety of malformations and compared the observations with those in normal fetuses (4,5,6). However, it did appear that the most significant abnormalities were noted in fetuses with aortopulmonary transposition (APT) and hypoplastic left heart syndrome (HLHS). Head size at birth was noted to be reduced in infants with APT and particularly in those with HLHS (7). Hinton et al. (8) noted a significant reduction of head growth in fetuses with HLHS during the latter half of gestation; also, in 11 fetuses aborted electively, histopathology revealed diffuse cerebral white matter injury. Quantitative magnetic resonance imaging at 25–37 wk gestation showed a decrease in brain volume in fetuses with various congenital cardiovascular malformations compared with normal fetuses. These differences were most prominent in those with HLHS (5)
This evidence of prenatal disturbance in cerebral development has raised questions regarding possible mechanisms. Genetic disturbances with which the cardiovascular malformations are associated could be responsible; this requires further study. Recently, there has been considerable interest in the possibility that altered circulatory dynamics could result in cerebral injury. It has been proposed that cerebral hypoxia, associated with a decrease in the oxygen content of cerebral arterial blood, is primarily responsible for the disturbance in brain development. This has led to the suggestion that oxygen administration to the mother for prolonged periods should be considered, in an attempt to increase fetal blood oxygen content and thus improve oxygen delivery to the brain (6). Some centers in the United States and Europe have already instituted this approach. I suggest that this practice is premature and that the cerebral disturbance is the result of decrease glucose, rather than oxygen, supply to the brain.
The altered circulation in congenital cardiovascular malformations possibly affects cerebral development by decreasing oxygen saturation of cerebral arterial blood (hypoxemia) (4,6); decreasing cerebral energy substrate (glucose) supply; or decreasing cerebral blood flow with reduced oxygen and substrate supply (9,10).
Because cerebral development has been affected mainly in fetuses with HLHS and APT, these are the malformations I will discuss
Fetal Cerebral Development and Blood Flow
Brain weight increases proportionally with body weight in the latter half of gestation both in the lamb and human fetus. However, in the lamb, brain weight is two percent or less of body weight, whereas in the human, fetal brain weight is 13–14 percent of body weight ( Figure 1 ). Despite the fact that brain weight relative to body weight does not change, there is a dramatic increase in blood flow relative to brain weight, particularly in the latter third of gestation. This is probably due to the rapid acceleration of synapse development and cerebral myelination, which would increase the demand for oxygen and energy substrates for metabolism. It is associated with a marked increase in cerebral vascularity (11). In the fetal lamb, blood flow per 100 g of brain weight is about 30 ml/min at 60 d gestation; it increases to about 130 ml/min near term (~150 d) ( Figure 2 ). During late gestation, the brain receives about 3.5 percent of the combined ventricular output of about 450 ml//min/kg fetal weight.
Fetal brain weight. Changes in brain weight are shown relative to body weight during gestational development in the lamb (a) and human (b) fetus. Brain weight is about two percent of body weight in the lamb (x----x----x), but 13–14 percent in the human (.__.__.); the percentage does not change significantly with advancing gestation (a constructed from data in ref. (25) and b from data in ref. (26)).
Changes in brain blood flow relative to brain weight during gestational development of the lamb fetus. Note the progressive increase in flow per 100 g of brain in the latter third of gestation (constructed from data in ref. (27)).
In the human fetus, combined ventricular output is 450–500 ml/kg/min. No reliable data are available for cerebral blood flow in late gestation, but if it is assumed that blood flow/i00 g of brain is the same as in the lamb, total cerebral flow would be about 350 ml/min/kg of fetal weight, representing more than 50 percent of combined ventricular output. Cerebral blood flow is probably lower, because hemoglobin concentration is much higher in late gestation. In the lamb, hemoglobin concentration is 7–8 g/dl at 90 d and 8–10 g/dl at term. However, in the human fetus, it is 9.0 ± 2.8 g/dl at 10 wk and 16.5 ± 4.0 at 39 wk (12). Thus cerebral oxygen supply could be provided at lower blood flow because higher hemoglobin concentration would provide a greater oxygen delivery at the same oxygen saturation of cerebral arterial blood. However, this will not facilitate an increase in metabolic substrate supply.
In the adult, cerebral autoregulation provides for a constant blood flow per 100 g brain weight over a wide range of mean arterial perfusion pressure, from about 60–160 mm Hg; below 60 mm Hg, perfusion falls linearly with pressure. In the fetal lamb, autoregulation of cerebral vasculature provides constant flow at mean pressures of 40–80 mm Hg ( Figure 3 ). Cerebral flow progressively falls at pressures below 40 mm Hg (13). Pulsation is also important in facilitating cerebral blood flow and decreased pulsatility could reduce flow at similar mean pressures (14)
Diagram comparing cerebral autoregulation in adult and fetus. In the adult, cerebral perfusion is constant when mean perfusion pressure is 60–160 mm Hg. In the fetus, cerebral flow is constant at mean pressures of 40–80 mm Hg. Below 40 mm Hg, flow falls precipitously with decreasing pressure.
Cerebral Arterial Pulsatility Index
Application of the Doppler ultrasound technique allows definition of the velocity profile of flow through vessels. An index, defined as the pulsatility index (PI), has been derived from the velocity profile over the cardiac cycle; it is estimated from the equation—peak velocity minus minimal velocity divided by the mean velocity. From Doppler flow studies in anterior or middle cerebral arteries, the PI is currently being used to define cerebral vascular resistance, with a decrease in the index denoting a fall in cerebral vascular resistance. It has been applied to study of cerebral vasculature in fetuses with congenital cardiovascular malformations (4). However, factors other than changes in vascular resistance may affect PI; it may be altered by changes in arterial compliance, ventricular ejection and stroke volume and by vascular obstruction.
Cerebral Oxygen and Substrate Metabolism in the Fetus
In the late gestation fetal lamb, about 12 ml/min/100 g of oxygen is delivered to the brain and oxygen consumption (QO2) is about 4 ml/min/100 g (15). This represents about 10 percent of total oxygen consumption by the fetus. Cerebral glucose consumption is about 5.3 mg/min/100g and it is estimated this accounts for about 15 percent of total glucose metabolism in the fetal lamb (16). Since the mean glucose-oxygen quotient is 1.10, glucose metabolism accounts for all oxygen utilization (12). No reliable data are available for the human fetus; it has been proposed that, during late gestation, the brain utilizes about 50 percent of total QO2, and also 50 percent of glucose metabolized (17). Glucose is normally the only energy substrate for the brain; it is metabolized to pyruvate, which, with adequate oxygen availability, is then processed through the tricarboxylic acid cycle. If oxygen supply is inadequate, pyruvate is metabolized to lactate. Thus energy supply may be decreased by either low glucose or low oxygen availability. If oxygen supply is reduced, anaerobic metabolism results in lactate production. However with inadequate glucose supply, lactate production is not increased (18).
Studies of the effects of hypoxemia of cerebral arterial blood on cerebral blood flow have shown a remarkable ability of the brain to tolerate significant reduction of arterial oxygen content. This is accomplished by a reduction of cerebral vascular resistance with an increase in blood flow; reduction of carotid arterial oxygen tension from 21 to 12 mm Hg (oxygen saturations about 65 and 35 percent) almost doubled cerebral blood flow in fetal lambs (19). As a result of the enhanced flow, QO2 per 100 g of brain tissue was maintained when arterial oxygen tension fell from 36 to 14 mm Hg (15).
Fetuses with Congenital Cardiovascular Malformations
Fetal cerebral development, blood flow, and metabolism in fetuses with congenital cardiovascular malformations have been reviewed in several studies (4,5,6). Unfortunately, fetuses with malformations with vastly different hemodynamic disturbances have been grouped to compare with normal fetuses. However, observation of the data indicates that cerebral insult occurs predominantly with HLHS and APT.
HLHS
In this malformation, left ventricular output is reduced and in the extreme of aortic atresia, no blood is ejected into the ascending aorta. There is complete admixture of well-oxygenated umbilical venous blood and poorly oxygenated systemic venous blood in the right atrium, thus blood with the same oxygen content is distributed to the lungs and through the ductus arteriosus to the whole fetal body.
Because of this admixture, oxygen saturation (SaO2) of blood distributed to the brain is lower than normal; in the fetal lamb carotid arterial SaO2 is 60–65 percent. Assuming that in the human fetus umbilical venous SaO2 is about 80 percent and systemic venous SaO2 about 40 percent, based on measurements of umbilical and systemic venous flows, the mixed SaO2 would be 50–55 percent.
The concept is now widely held that reduced oxygen supply to the brain interferes with its development. The observation that the cerebral arterial PI was decreased in fetuses with congenital heart disease, but particularly with HLHS, suggested that cerebral vascular resistance was reduced. It was proposed that this could be the result of the reduced SaO2 of cerebral arterial blood (4). Cerebral QO2 has been reported to be reduced in a group of fetuses with various congenital cardiovascular malformations (6); however, the cerebral QO2 was expressed in relation to fetal body weight, not to brain weight. Because brain size was reduced in some fetuses, it might be expected that cerebral QO2 related to body weight would be reduced and that the lower QO2 could be the result, rather than the cause of the small brain size. The decrease of SaO2 of cerebral arterial blood to 50–55 percent in the complete admixture lesion is most unlikely to affect cerebral oxygenation, because, as mentioned above, cerebral QO2 is not reduced with decreases in arterial SaO2 to as low as about 35 percent (15).
Comparison between HLHS and another complete admixture malformation, pulmonary atresia, also raises questions regarding the possible role of the reduced arterial SaO2. In fetuses with pulmonary atresia, complete admixture of umbilical and systemic venous blood occurs in the left atrium. This mixed blood is distributed via the aorta to the whole body and its SaO2 would be the same as that in HLHS—50–55 percent. Whereas the cerebral arterial PI is reduced in HLHS, it is normal or increased in fetuses with pulmonary atresia (19). Furthermore, interference with cerebral development has not been noted in fetuses and infants with pulmonary atresia. This raises questions regarding the concept that the reduced PI in HLHS is reflecting a decreased cerebral vascular resistance resulting from arterial hypoxemia and suggests that other factors could be involved in the changes in PI.
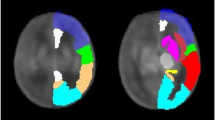
I propose that the alterations in blood flow patterns in fetuses with HLHS and pulmonary atresia are contributing to the changes in PI. In the fetus with HLHS, the right ventricle ejects into the pulmonary trunk and blood flow to the whole fetal body, apart from the lungs, passes through the ductus arteriosus. To reach the upper body, blood flows retrograde through the aortic arch; there is thus a very circuitous pathway for blood to reach the cerebral arteries ( Figure 4 ). This could interfere with the transmission of the pulse wave from the ventricle and account for the reduced PI. In addition, coarctation of the aorta has been found to present in about 70 percent of patients with HLHS; in half of them, the coarctation was preductal (between the ductus and the aortic isthmus) and in most of the others, it was juxtaductal (20). Thus, in addition to the circuitous blood flow, obstruction to flow from the ductus to the cerebral arteries could contribute to decreasing the PI. The combination of the circuitous pathway and frequent obstruction could result in a decrease of cerebral arterial pressure. Because cerebral autoregulation is not effective at lower perfusion pressures, cerebral blood flow could be significantly reduced. As mentioned above, reduced pulsatility could further compromise cerebral blood flow.
Blood flow patterns. Course of blood flows in fetuses with aortic atresia (a) and pulmonary atresia (b). In aortic atresia blood flow to the brain is derived from the right ventricle. It passes circuitously through the pulmonary artery, ductus arteriosus, and aortic arch. In addition, coarctation of the aorta frequently imposes some obstruction to flow into the aortic arch. In pulmonary atresia, the left ventricle ejects a large stroke volume directly into the ascending aorta. Asc Ao, ascending aorta; DA, ductus arteriosus; PA, pulmonary arteries; RV, LV, right, left ventricle; UV/DV, umbilical vein, ductus venosus.
The increase in PI in fetuses with pulmonary atresia is also probably related to hemodynamic factors. In this malformation, the total cardiac output is ejected by the left ventricle, thus almost doubling the normal output ( Figure 4 ). The high stroke volume and greater velocity of ascending aortic flow is transmitted to the cerebral arteries, resulting in the increased PI. Any change in PI due to a decrease in cerebral vascular resistance resulting form arterial hypoxemia is surmounted by the hemodynamic changes in flow in the aorta.
Disturbances in cerebral development in HLHS most likely result from inadequate cerebral perfusion. The adverse effects are most likely to occur in the latter half of gestation, because normally, blood flow per 100 g of brain tissue progressively increases during this time (see above). The inadequate perfusion compromises not only oxygen supply, but also delivery of metabolic substrates, predominantly glucose. It is more likely that the reduction in glucose supply is the crucial factor in affecting cerebral development. This concept is supported by the magnetic resonance spectroscopy studies of fetuses with HLHS by Limperopoulos et al. (5). They observed that cerebral lactate levels were elevated in only 5 of 19 of these fetuses. As discussed above, inadequate oxygen supply results in lactate accumulation, whereas inadequate glucose supply is not associated with increased lactate production. Possibly, if oxygen deprivation is greater than deficient glucose supply, lactate may be present.
APT
In the normal fetus, well-oxygenated umbilical venous blood is distributed to the liver and through the ductus venosus. Left hepatic venous blood, which has a relatively high SaO2, together with ductus venosus blood, is directed preferentially through the foramen ovale to the left atrium and ventricle and ejected into the ascending aorta. This provides blood with a relatively high SaO2 to the cerebral circulation. Poorly oxygenated venous blood from the superior and inferior vena cava passes preferentially through the tricuspid valve to the right ventricle and is ejected into the pulmonary trunk to be distributed to the lung and through the ductus arteriosus to the descending aorta. In the fetal lamb, the SaO2 is 60–65 percent in carotid arterial and 50–55 percent in descending aortic, blood (21).
In the fetus with APT, venous drainage patterns appear to be normal. However, well-oxygenated blood ejected by the lift ventricle passes to the pulmonary circulation and through the ductus arteriosus to the descending aorta. Poorly oxygenated blood from the right ventricle is ejected into the ascending aorta and the cerebral circulation ( Figure 5 ). The SaO2 in various vessels are not known, but can be estimated to be about 40–45 percent in the ascending aorta and about 60 percent in the descending aorta.
Diagram of circulation in fetus with aortopulmonary transposition.Well-oxygenated umbilical venous blood passes through the foramen ovale to the left atrium and ventricle. It is ejected into the pulmonary artery; during systole some passes through the ductus arteriosus to the descending aorta. Poorly oxygenated venous blood passes to the right atrium and ventricle. It is ejected into the ascending aorta and to the cerebral circulation. During diastole, the low pulmonary vascular resistance favors run-off of blood from the ascending aorta and arch through the ductus arteriosus to the lungs. Asc AO, ascending aorta; DA, ductus arteriosus; PA, pulmonary artery; RV, LV, right, left ventricle; RA, LA, right, left atrium; SVC, IVC, superior, inferior vena cava; UV/DV, umbilical vein, ductus venosus.
The decreased cerebral arterial SaO2 possibly could affect cerebral oxygenation, but in fetal lamb studies, QO2 was maintained by vasodilatation, with an increase of flow (15). A reduction in cerebral vascular resistance should be reflected in a decrease in PI. Studies of cerebral arterial PI in fetuses with transposition show inconsistent results. Jouannic found the index was decreased (22) but Berg found normal indices (23). It is possible that, as with HLHS, hemodynamic factors other than cerebral vascular resistance may affect the PI.
In the fetus with APT, the well-oxygenated blood ejected by the left ventricle will enter the pulmonary circulation and thus pulmonary vascular resistance would be reduced; this could have significant effects on the dynamics of flow in the ductus arteriosus and aortic arch. Normally, blood flows only from the pulmonary artery to the descending aorta during both systole and diastole. In the latter part of gestation, the fetus with transposition may show bidirectional flow; during systole blood flows from the pulmonary trunk to the descending aorta, but in diastole, flow is from the aortic arch to the pulmonary arteries ( Figure 5 ). The kinetics associated with ventricular contraction favors flow from the pulmonary trunk to the descending aorta during systole; this is enhanced by the short distance from the pulmonary valve to the ductus arteriosus in APT. During diastole, blood flows from the aorta to the pulmonary circulation, because pulmonary vascular resistance is reduced. This run-off of blood from the ascending aorta during diastole could significantly reduce diastolic pressure and cerebral perfusion. These hemodynamic factors could also influence the PI in the cerebral arteries.
Although most attention has been directed to the possible role of inadequate oxygen supply as a cause of the reduced brain volume in fetuses with transposition, it is important to recognize that cerebral glucose supply may be deficient. Glucose is delivered to the fetus from the placenta through the umbilical vein; thus in the normal fetus, blood with a high glucose concentration would be preferentially directed to the left atrium and ventricle, then into the ascending aorta, thus favoring glucose supply to the cerebral circulation. In the fetus with APT, the brain would receive mainly venous blood from the right atrium and ventricle, ejected into the ascending aorta, and not derive the benefit of glucose from the umbilical vein. Although glucose concentration in pulmonary venous blood would be relatively high, little would cross the foramen ovale to the right atrium to be directed to the brain. Because pulmonary vascular resistance is decreased, pulmonary blood flow is high and would be recirculated in the left side of the heart with little passage to the right side. Descending aortic concentration of glucose would be higher than normal. I propose that the interference in cerebral development in the fetus with APT is primarily related to decreased energy substrate supply rather than inadequate oxygenation. This is supported by the observation that in magnetic resonance spectroscopy studies of brains of 13 fetuses with transposition, only two showed presence of lactate (5).
Conclusion
Impairment of brain development in fetuses with congenital cardiovascular malformations is now widely recognized. However, this has not been associated with all congenital heart defects, but only with some, particularly with HLHS and APT. It is therefore inappropriate to compare groups comprising a variety of lesions with different hemodynamic disturbances, with normal fetuses, as had been done in many reports (4,5,6). Rather, each malformation should be considered separately.
Based on the observation that cerebral arterial PI was reduced in fetuses with congenital heart disease, it was suggested that this reflected a decreased cerebral vascular resistance and that this was caused by a fall in cerebral arterial SaO2 (hypoxemia), resulting from abnormal flow patterns (4). Cerebral hypoxia is now widely considered to be the cause of the abnormal cerebral development. However, as discussed above, cerebral arterial PI could be affected by hemodynamic disturbances other than vascular resistance. Also, in fetal lambs, even quite severe reduction of cerebral arterial SaO2 does not induce a fall in cerebral oxygen consumption, due to the compensatory increase in blood flow.
I propose that, rather than a decrease in oxygen supply, interference with glucose supply is the more important factor responsible for impaired cerebral development. In HLHS, this is the result of decreased cerebral perfusion. A low cerebral flow could also interfere with oxygen delivery, but the infrequent detection of lactate in the brain by magnetic resonance spectroscopy suggests that deficient glucose supply is the primary concern. In fetuses with APT, umbilical venous blood containing glucose from the placenta is largely distributed through the foramen ovale to the lungs and descending aorta. The brain is perfused mainly with systemic venous blood and thus glucose delivery could be impaired. Cerebral perfusion could also possibly be affected by the run-off of aortic blood through the ductus arteriosus to the pulmonary circulation during diastole. The delivery of blood with a low SaO2 could contribute to the impaired brain growth, but the fact that lactate was observed infrequently in brains of fetuses with APT (5), supports the importance of inadequacy of glucose supply.
Based on the concept that impaired brain development is the result of cerebral arterial hypoxemia, it has been suggested that oxygen be administered to mothers of fetuses with “congenital heart disease” (6). This should not be recommended until more information is available regarding glucose and oxygen supply in fetuses with specific congenital cardiovascular malformations. Recently, glucose has been infused over an extended period in a fetus with intrauterine growth retardation to improve growth (24). Glucose infusion into fetuses with specific cardiac malformations to promote brain growth could possibly be recommended. However, it is inadvisable to consider this approach without more specific information about possible adverse effects of glucose infusion into the fetus.
Statement of Financial Support
No financial assistance was received to support this article.
Disclosure
None.
References
Aisenberg RB, Rosenthal A, Nadas AS, Wolff PH. Developmental delay in infants with congenital heart disease. Correlation with hypoxemia and congestive heart failure. Pediatr Cardiol 1982;3:133–7.
Limeropoulos C, Rosenblatt B, Rohliceck CV. Neurodevelopmental status of newborns and infants with congenital heart defects before and after surgery. J Pediatr. 2000; 137: 638–45
Marino BS, Lipkin PH, Newburger JW, et al.; American Heart Association Congenital Heart Defects Committee, Council on Cardiovascular Disease in the Young, Council on Cardiovascular Nursing, and Stroke Council. Neurodevelopmental outcomes in children with congenital heart disease: evaluation and management: a scientific statement from the American Heart Association. Circulation 2012;126:1143–72.
Donofrio MT, Bremer YA, Schieken RM, et al. Autoregulation of cerebral blood flow in fetuses with congenital heart disease: the brain sparing effect. Pediatr Cardiol 2003;24:436–43.
Limperopoulos C, Tworetzky W, McElhinney DB, et al. Brain volume and metabolism in fetuses with congenital heart disease: evaluation with quantitative magnetic resonance imaging and spectroscopy. Circulation 2010;121:26–33.
Sun L, Macgowan CK, Sled JG, et al. Reduced fetal cerebral oxygen consumption is associated with smaller brain size in fetuses with congenital heart disease. Circulation 2015;131:1313–23.
Manzar S, Nair AK, Pai MG, Al-Khusaiby SM. Head size at birth in neonates with transposition of great arteries and hypoplastic left heart syndrome. Saudi Med J 2005;26:453–6.
Hinton RB, Andelfinger G, Sekar P, et al. Prenatal head growth and white matter injury in hypoplastic left heart syndrome. Pediatr Res 2008;64:364–9.
Rudolph AM.Congenital Diseases of the Heart. 3rd edn. Chichester, UK: Wiley-Blackwell, 2009; 285.
McQuillen PS, Goff DA, Licht DJ. Effects of congenital heart disease on brain development. Prog Pediatr Cardiol 2010;29:79–85.
du Plessis AJ. Cerebral blood flow and metabolism in the developing fetus. Clin Perinatol 2009;36:531–48.
Brown MS. Fetal and neonatal erythropoiesis. In Developmental and Neonatal Hematology. Stockman JA III, Pochedly C (eds.). New York: Raven Press, 1988.
Papile LA, Rudolph AM, Heymann MA. Autoregulation of cerebral blood flow in the preterm fetal lamb. Pediatr Res 1985;19:159–61.
Undar A, Masai T, Beyer EA, Goddard-Finegold J, McGarry MC, Fraser CD Jr . Pediatric physiologic pulsatile pump enhances cerebral and renal blood flow during and after cardiopulmonary bypass. Artif Organs 2002;26:919–23.
Jones M Jr, Sheldon RE, Peeters LL, Meschia G, Battaglia FC, Makowski EL. Fetal cerebral oxygen consumption at different levels of oxygenation. J Appl Physiol Respir Environ Exerc Physiol 1977;43:1080–4.
Duggan C, Watkins JB, Walker WA. Nutrition in Pediatrics: Basic Science, Clinical Applications. Hamilton: BC Decker; 2008
Makowski EL, Schneider JM, Tsoulos NG, Colwill JR, Battaglia FC, Meschia G. Cerebral blood flow, oxygen consumption, and glucose utilization of fetal lambs in utero. Am J Obstet Gynecol 1972;114:292–303.
Ghosh A, Smith M. Brain tissue biochemistry. Core Topics in Neuroanesthesia and Neurointensive Care. Matta BF, Menon DK, Smith M (eds.). New York NY: Cambridge Univ Press, 2011;90.
Szwast A, Tian Z, McCann M, Soffer D, Rychik J. Comparative analysis of cerebrovascular resistance in fetuses with single-ventricle congenital heart disease. Ultrasound Obstet Gynecol 2012;40:62–7.
Mahowald JM, Lucas RV Jr, Edwards JE. Aortic valvular atresia. Associated cardiovascular anomalies. Pediatr Cardiol 1982;2:99–105.
Rudolph AM. Aortopulmonary transposition in the fetus: speculation on pathophysiology and therapy. Pediatr Res 2007;61:375–80.
Jouannic JM, Benachi A, Bonnet D, et al. Middle cerebral artery Doppler in fetuses with transposition of the great arteries. Ultrasound Obstet Gynecol 2002;20:122–4.
Berg C, Gembruch O, Gembruch U, Geipel A. Doppler indices of the middle cerebral artery in fetuses with cardiac defects theoretically associated with impaired cerebral oxygen delivery in utero: is there a brain-sparing effect? Ultrasound Obstet Gynecol 2009;34:666–72.
Tchirikov M, Kharkevich O, Steetskamp J, Beluga M, Strohner M. Treatment of growth-restricted human fetuses with amino acids and glucose supplementation through a chronic fetal intravascular perinatal port system. Eur Surg Res 2010;45:45–9.
Barcroft J. Researches on Pre-natal Life. Charles C Thomas, Springfield IL 1947.
Guihard-Costa AM, Ménez F, Delezoide AL. Organ weights in human fetuses after formalin fixation: standards by gestational age and body weight. Pediatr Dev Pathol 2002;5:559–78.
Rudolph AM, Heymann MA. Circulatory changes during growth in the fetal lamb. Circ Res 1970;26:289–99.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rudolph, A. Impaired cerebral development in fetuses with congenital cardiovascular malformations: Is it the result of inadequate glucose supply?. Pediatr Res 80, 172–177 (2016). https://doi.org/10.1038/pr.2016.65
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2016.65
This article is cited by
-
Antenatal and Perioperative Mechanisms of Global Neurological Injury in Congenital Heart Disease
Pediatric Cardiology (2021)
-
Maternal hyperoxygenation for the human fetus: should studies be curtailed?
Pediatric Research (2020)
-
Investigating altered brain development in infants with congenital heart disease using tensor-based morphometry
Scientific Reports (2020)