Abstract
Background:
To describe the interrelationship between antenatal steroids, exogenous surfactant, and two approaches to lung recruitment at birth on oxygenation and respiratory system compliance (Cdyn) in preterm lambs.
Methods:
Lambs (n = 63; gestational age 127 ± 1 d) received either surfactant at 10-min life (Surfactant), antenatal corticosteroids (Steroid), or neither (Control). Within each epoch lambs were randomly assigned to a 30-s 40 cmH2O sustained inflation (SI) or an initial stepwise positive end-expiratory pressure (PEEP) open lung ventilation (OLV) maneuver at birth. All lambs then received the same management for 60-min with alveolar–arterial oxygen difference (AaDO2) and Cdyn measured at regular time points.
Results:
Overall, the OLV strategy improved Cdyn and AaDO2 (all epochs except Surfactant) compared to SI (all P < 0.05; two-way ANOVA). Irrespective of strategy, Cdyn was better in the Steroid group in the first 10 min (all P < 0.05). Thereafter, Cdyn was similar to Steroid epoch in the OLV + Surfactant, but not SI + Surfactant group. OLV influenced the effect of steroid and surfactant (P = 0.005) on AaDO2 more than SI (P = 0.235).
Conclusions:
The antenatal state of the lung influences the type and impact of a recruitment maneuver at birth. The effectiveness of surfactant maybe enhanced using PEEP-based time-dependent recruitment strategies rather than approaches solely aimed at initial lung liquid clearance.
Similar content being viewed by others
Main
It is widely agreed that the optimal support of the preterm lung involves the combination of antenatal corticosteroid exposure, exogenous surfactant therapy, and early application of lung protective respiratory support strategies (1). Together, these therapies reduce the potential of assisted ventilation to injure the developmentally immature, surfactant-deficient preterm lung. The roles of early exogenous surfactant therapy (2) and antenatal corticosteroids (3) in improving lung mechanics, functional residual capacity, and reducing respiratory support are well established. The optimal respiratory support strategies are still debated (4,5,6,7).
Ideally, lung protective respiratory support should commence during transition to ex utero life (1,8). During this period, the infant must rapidly clear lung liquid, aerate the lung, establish a functional residual capacity, and commence tidal ventilation, processes influenced by the intrinsic mechanical properties of the lung as well as the applied respiratory strategy (5,6,9,10,11,12,13). The optimal approach in preterm infants remains unclear but broadly requires an inflating pressure to drive fetal lung fluid into the alveoli and allow lung aeration, and positive end-expiratory pressure (PEEP) to maintain aeration and prevent fluid efflux back into the airways (14,15,16,17). In preterm animals, using an initial stepwise PEEP or open lung ventilation (OLV) approach during tidal ventilation from birth improves aeration and short-term respiratory outcomes in preterm animals via utilizing hysteresis and time dependency (6,11). However, clinical trials at birth are lacking. The most widely examined intentional recruitment maneuver at birth is the use of an initial sustained inflation (SI) to clear fetal lung liquid from the airways (18,19). Preclinical experimental studies of SI have been mixed (5,6,9,10,11,20), with an increase in lung injury reported in some studies (21,22,23). Improved short-term respiratory outcomes have been reported in some clinical trials (24,25), although without long-term benefits, and an increased risk of patent ductus arteriosus (19).
The interrelationship between antenatal corticosteroids, surfactant replacement, and intentional recruitment maneuvers is not fully understood. The intentional exploitation of the mechanical properties of the lung inherent in all recruitment strategies suggests that antenatal steroids and surfactant therapy may influence their effectiveness. The role of recruitment maneuvers on subsequent respiratory therapies may also be important. Clinical studies of SI have suggested a reduced need for surfactant replacement following a SI (24,25,26). However, in preterm lambs, pretreatment with surfactant improves the lung injury patterns and response to a SI compared with post-SI surfactant (12), suggesting a recruitment maneuver may also influence subsequent respiratory therapies (8). The interplay of antenatal steroids with intentional recruitment maneuvers is even less well understood. As the question of the clinical use of recruitment maneuvers at birth becomes more topical, the application of future algorithms will need to consider the interdependency between established respiratory therapies and the applied recruitment strategy.
The aim of this study was to describe the interrelationship between antenatal steroid exposure, exogenous surfactant therapy, and a SI or an OLV approach at birth on oxygenation and respiratory system compliance in preterm lambs. This study was a priori designed as part of a 3-y program of nested studies examining the role of inflating pressure (SI) and stepwise PEEP approaches (OLV) on regional aeration, lung mechanics, and lung injury. Some of the detailed individual injury and physiological data have been reported separately (6,11).
Results
Fetal Characteristics
Sixty-three lambs were studied. Their characteristics are described in Table 1 . Overall, the groups were well matched by epoch and ventilation strategy. Birth weight was lower in the Steroid epoch compared with Control epoch (P = 0.009; one-way ANOVA), and specifically due to the Steroid + SI group compared to Control + SI and SI + Surfactant groups (P = 0.001; one-way ANOVA). The OLV + Surfactant group was also a mean (95% confidence interval) of 0.72 (0.33, 1.11) kg lighter than the SI + Surfactant group (t-test). Overall, there was no difference in the SI and OLV birth weights across all epochs (P = 0.057, t-test). Breeding resulted in more singletons than expected in the Control and Surfactant epochs, reaching significance in the Control-SI group (P = 0.0001, chi-squared test). All lambs completed the study without complications, including pneumothoraces. There were no differences in heart rate, blood pressure, or temperature (data not presented).
Respiratory System Compliance
Pooling all epochs, Cdyn improved with time during the study in both the SI and OLV groups (P = 0.0002; Figure 1a ). Overall, the OLV strategy resulted in better Cdyn than the SI (P < 0.0001).
Pooled compliance and oxygenation. (a) Cdyn and (b) AaDO2 over time for the SI (closed circles; n = 31) and OLV (open diamonds; n = 32) groups, combining data from all adjunctive therapy allocations. Time of surfactant therapy (10 min) indicated with dashed line. Cdyn improved by a mean (95% CI) of 0.08 (0.04, 0.12) ml/kg/cmH2O and 0.06 (0.04, 0.08) ml/kg/cmH2O between 5 and 60 min in the OLV and SI groups, respectively. AaDO2 increased by a mean (95% CI) of 87.1 (44.7, 129.6) mm Hg and 183.3 (130.7, 236.0) mm Hg between 5 and 60 min in the OLV and SI groups, respectively. *P < 0.05, **P < 0.01 (two-way ANOVA with Sidak posttests). All data mean (SD). CI, confidence interval; OLV, open lung ventilation; SI, sustained inflation.
Within the SI groups, Cdyn was not different between the Control + SI and SI + Surfactant groups ( Figure 2b ), and Cdyn was lower in both compared to Steroid + SI (all P < 0.01). In contrast, only in the first 10 min of life was Cdyn better in the Steroid + OLV group compared to both Control + OLV (P = 0.009) and OLV + Surfactant (P = 0.038) groups ( Figure 2b ). After surfactant was administered, the OLV + Surfactant group demonstrated similar Cdyn values as Steroid + OLV. The Control + OLV had a significantly lower Cdyn than Steroid + OLV for the entire study, and against OLV + Surfactant at 60 min (all P < 0.05).
Influence of adjunctive therapy on compliance and oxygenation. Cdyn and AaDO2 for the SI (a and c, circles) and OLV (b and d, diamonds) groups. Open symbols represent the Control epoch, grey symbols Surfactant, and black symbols Steroid. Time of surfactant therapy (10 min) indicated with dashed line. At 60 min both the Steroid and Surfactant epochs had better Cdyn than the Control group in the OLV cohort. All data mean (SD). *P < 0.05 and **P < 0.01 vs. Steroid and †P < 0.01 Surfactant and Control vs. Steroid (two-way ANOVA with Sidak posttests). OLV, open lung ventilation; SI, sustained inflation.
Within each treatment epoch, the use of the OLV strategy significantly improved Cdyn compared to a SI: Control (P < 0.0001), Surfactant (P < 0.0001), and Steroid (P = 0.008) epochs. Time was also a significant factor in the Surfactant (P = 0.0041) and Steroid (P = 0.0153) epochs.
Oxygenation
Figure 1b shows AaDO2 data for the pooled SI and OLV groups. Both strategies exhibited worsening AaDO2 over the 60 min period (P < 0.0001; two-way ANOVA), but AaDO2 was significantly lower in OLV recipients from 30 min of life compared to SI (P < 0.0001).
In the SI recipients, AaDO2 behaved similarly during the entire study period, with no difference between epochs (P = 0.235; Figure 2c ). In contrast, epoch allocation (P = 0.005) was a significant factor in OLV recipients ( Figure 2d ), with the Steroid + OLV group having lower AaDO2 values at 5 and 30 min compared to Surfactant + OLV (P = 0.033) and Control + OLV (P = 0.021) groups, respectively. After surfactant administration, there was no difference in the Surfactant + OLV compared to Steroid + OLV.
OLV resulted in lower AaDO2 compared to SI in the Steroid and Control epochs, with time and strategy being significant factors (all P < 0.0001). Posttest analysis identified better oxygenation in the OLV recipients from 30 min of life in the Control epoch and 45 min in the Steroid epoch. There was no difference in AaDO2 between the Surfactant + SI and Surfactant + OLV groups with regards to time (P = 0.058) and strategy (P = 0.716).
Discussion
There is growing interest in the role of respiratory strategies in the Delivery Room. In our study using intubated preterm lambs, we systematically describe the interrelationship between the use of antenatal corticosteroids, exogenous surfactant therapy, and two distinct recruitment strategies applied at birth. A strategy that maintained tidal recruitment over time via an open lung approach to PEEP resulted in better Cdyn and oxygenation compared to an initial SI, irrespective of the use or not of adjunctive therapies. Importantly, the lung recruitment approach preceding exogenous surfactant administration modulated the short-term surfactant response. Our findings may have relevance to the development of clinical respiratory strategies to support the preterm lung at birth.
Unlike previous animal studies of respiratory care at birth (6,10,11,12,15,16,20,21,22,27,28,29,30), our study involved a large sample size. Pooling all epochs, the use of an OLV stepwise PEEP approach significantly improved Cdyn and oxygenation compared to a 30-s 40 cmH2O SI. Respiratory birth transition needs to be considered as a continuum, from clearance of fetal lung liquid, to alveolar aeration and prevention of fluid efflux during expiratory elastic recoil, through to effective tidal ventilation (4). Fundamental to this process is the establishment and maintenance of a sufficient volume state (6). A SI focuses on the initial fluid clearance and aeration but its value depends on subsequent respiratory management maintaining aeration. PEEP is essential in the preterm lung (5,14). In our study, we used a PEEP (8 cmH2O) previously shown to be appropriate in preterm lambs (6,11,16,17), and higher than that used in similar animal studies (5,9,10,14,15,20,29), suggesting our results are due to differences in recruitment strategy and not subsequent ventilator management.
An OLV strategy provides increasing PEEP support with an approach designed to exploit hysteresis (31,32). This approach is known to place ventilation on the deflation limb of the quasi-static pressure–volume relationship (31,33) and targets the region of optimal compliance (31,32,33,34). Thus, it is not surprising that the OLV approach improved Cdyn and oxygenation. Initial aeration was achieved using only 0.4-s tidal inspiratory times, suggesting that the benefits were related to both the prevention of fluid efflux during early respiratory transition and optimization of volume history during subsequent tidal ventilation. The OLV PEEP strategy was applied over a longer period than just the single 30-s SI, illustrating the importance of recruitment as a function of pressure and time dependence (35). This supports the argument that PEEP, and how it is used, maybe more important than the first inflation at birth. To date, a number of trials of SI but not PEEP recruitment at birth have been performed in humans (4,18,19).
Surfactant is known to improve lung mechanics and oxygenation, and its benefits in preterm infants are well established (2). The lack of improvement in Cdyn and AaDO2 following surfactant administration in the SI groups was surprising. While many previous preclinical studies of lung recruitment administered surfactant before the first inflation (21,36), our current strategy is more clinically applicable. We have recently shown that there is considerable variability in the spatiotemporal behavior of lung mechanics at birth, even in controlled preclinical experiments (6,12,23). Although our choice of SI parameters is based on previous work (9,10,12,20,27,29), it is likely that some of our lambs required a longer SI duration. Our results may reflect insufficient regional aeration, a situation clinicians currently have no bedside tools to rapidly detect during a SI. Irrespective of the specific strategy, our study highlights that an inadequate recruitment maneuver at birth might have a negative influence on subsequent respiratory therapies.
Antenatal steroids improve lung function in preterm lambs (37,38). It is not surprising that we demonstrated the response to any chosen recruitment maneuver at birth is likely to be different in the steroid-exposed and nonexposed fetal lung. The oxygenation benefit of steroid therapy was less convincing, with no difference in SI recipients and marginal benefit in OLV recipients. Unlike Cdyn, AaDO2 and SpO2 are influenced by ventilation–perfusion matching and hemodynamic transition (39). Clinicians need to be aware of the limitations of oxygenation as a marker of respiratory transition, at birth. Better clinically applicable measures of lung mechanics in early life are urgently needed.
Ultimately, the goal of any preterm respiratory intervention is to improve neurologically intact survival while reducing, or at least not increasing, lung injury. We have intentionally not reported lung injury in this study. Early lung injury is complicated and influenced by many factors beyond respiratory management (1). Although we controlled the breeding population and conditions as best as possible, maternal and environmental factors cannot be entirely standardized, limiting the accuracy of molecular comparison across epochs. This is evident by the difference in birth weight in the OLV + Surfactant group and the higher singleton rate in the Control + SI group. The former was likely due to the environmental factors, as these ewes were mated at the end of a long drought. The protective benefit of surfactant and steroids is established (2,3) and the important question is whether a specific recruitment strategy altered injury within a particular epoch. We have previously reported this (6,11) and have not shown a difference in early biomarkers of lung injury. The magnitude of influence from the recruitment maneuver on injury is likely to be less than maternal well-being, steroids, and surfactant, and the focus should be on ensuring that injury is not worsened using one approach.
The pressure and time criteria for the SI and OLV strategies used in our study are not consistent with human studies (18,19). To achieve lung aeration at birth, and then maintain recruitment and tidal ventilation, a recruitment strategy needs to overcome specific the mechanical and time constant constraints of the respiratory system (1,6,23). Practically, this requires an adequate inflating pressure and/or PEEP to be applied for a sufficient duration to achieve volume change (5,9,23). The preterm lamb is known to require a longer and higher inflating pressure to achieve lung aeration (10,13,20,23) than has been advocated in human trials (19,25). Although we would not advocate the use of these absolute SI and OLV parameters in humans, we contend that the choice of physiologically appropriate settings for the model allows for more meaningful translation.
To limit confounding factors, such as variable volume delivery, the lambs were anaesthetized and ventilated with a cuffed endotracheal tube, not a common clinical scenario. In unintubated preterm infants, the glottis is often closed at birth, which may limit the ability to deliver a sufficient volume to the lung (40). Pressure and VT delivery during facemask support is further complicated by operated-related variable delivery (18). Although both the OLV and SI strategy could be practically applied using a facemask and a variable pressure system (such as the Neopuff), we elected to use an intubated model to ensure standardization of the strategy effect. Common to other preterm lamb studies, lung fluid was passively drained before birth to better replicate the human scenario (6,13,17,23,29), but the residual volume in the lung needing to be overcome during aeration cannot be known. This further emphasizes the need for sufficiently powered animal studies.
It is feasible that the higher maximum possible inflating pressure during the OLV strategy, compared to the initial SI pressure of 40 cmH2O, influenced aeration (15,16). Recently, we reported the detailed analysis of the Control epoch compared to a group receiving positive pressure ventilation (PPV) at 8 cmH2O PEEP. There were better physiological outcomes in the OLV group and no difference between the SI and PPV only groups (6). Finally, although pneumothoraces were not found in our study population, reports in similar preterm lamb studies (6,17), and some human studies of SI (18,19), illustrate that the interaction between applied pressure and air leak in the preterm lung is not well understood. Interesting, in the already-aerated lung, air leak has not been a feature of OLV strategies in human (31,33) and animal studies (32,34,35).
In conclusion, our preterm lamb study demonstrates the interrelationship between the antenatal state of the lung, type and effectiveness of a recruitment maneuver at birth, and adjunctive lung protective therapies. In particular, independent of antenatal steroid and postrecruitment maneuver surfactant therapy, the use of a dynamic PEEP step recruitment strategy resulted in better oxygenation and dynamic compliance than a single SI at birth. Surfactant therapy after a dynamic PEEP step strategy, but not a SI, allowed further improvements in compliance, highlighting the potential role a recruitment maneuver at birth may have on optimizing other respiratory therapies. Our findings suggest a single unifying resuscitation algorithm is unlikely to account for these differences.
Methods
The study was performed at the animal research facility of the Murdoch Childrens Research Institute, Melbourne, Victoria, Australia. The Murdoch Childrens Research Institute ethics committee approved the study in accordance with the National Health and Medical Research Committee (Australia) guidelines.
Study Population
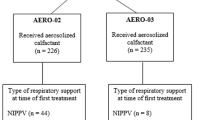
Border-Leicester/Suffolk lambs, gestational age 127 ± 1 d (term ~147 d), born via date-mating from a single Border-Leicester ewe flock and sired by two Suffolk rams. To standardize the environment exposure at conception and delivery, the study was performed within the austral winter and spring of 3 consecutive years, and all ewes came from the same breeding pedigree and location. The study was divided into three epochs detailed in Figure 3 :
Summary of study design. The study was performed over 3 y with each epoch representing the following permutations of adjunctive therapies and recruitment maneuvers. Year 1: Surfactant epoch in which all lambs received exogenous surfactant (100 mg/kg; Curosurf, Chiesi Farmaceutici SpA, Parma, Italy) and no antenatal steroid exposure. Year 2: Control epoch in which neither exogenous surfactant nor antenatal steroids were administered. Year 3: Steroid epoch in which lambs were born to ewes treated with 11.4 mg Betamethasone i.m. 24 and 48 h prior to delivery. No surfactant therapy was administered. In each epoch, lambs were randomized to either a SI or and OLV positive end-expiratory pressure strategy at birth. OLV, open lung ventilation; SI, sustained inflation.
Surfactant epoch. Exogenous surfactant (100 mg/kg; Curosurf, Chiesi Farmaceutici SpA, Parma, Italy) administered via the endotracheal tube using an in-line system at 10 min of life.
Control epoch. No exogenous surfactant or antenatal steroids.
Steroid epoch. Mothers treated with Betamethasone i.m. 24 and 48 h prior to delivery.
Experimental Instrumentation
Lambs were delivered via caesarean section under general anesthesia following instrumentation, intubation with a cuffed endotracheal tube, and, to replicate the human fetal fluid state, passive drainage of 10–15 ml/kg lung fluid on placental support using our previously described protocol (6,11,12,34). After delivery, animals were weighed and placed supine and monitoring and vascular lines were connected prior to commencing mechanical ventilation. Continuous infusions of ketamine and midazolam were used to maintain anesthesia/analgesia and suppress spontaneous respiratory effort.
Measurements
To monitor physiological stability, preductal peripheral oxygen saturation (SpO2), heart rate, arterial blood pressure, and rectal temperature (HP48S monitor, Hewlett Packard, Andover, MA) were recorded continuously from birth. A Florian Respiratory monitor (Acutronic Medical Systems AG, Hirzel, Switzerland) was used to continuously measure pressure (PAO), gas flow, and tidal volume (VT) at the airway opening (6,11,12). Arterial blood gases were performed at 5 min of age and every 15 min from birth. An additional gas analysis was performed at 10 min, or immediately prior to surfactant administration, for the Surfactant and Control epochs. As part of a different study (12,23), electrical impedance tomography imaging of tidal ventilation was available during the entire study, allowing continuous monitoring for pneumothoraces.
Ventilation Strategies at Birth
Within each epoch, lambs were randomly assigned before the delivery to one of the following ventilation strategies:
-
1
1. An initial 30-s SI, via the endotracheal tube at 40 cmH2O using a Neopuff Infant T-piece Infant Resuscitator (Fisher and Paykel Healthcare, Auckland, New Zealand), followed by 5 s at 8 cmH2O PEEP. PPV in a volume-targeted mode (SLE5000, SLE, South Croydon, UK) was then commenced at 8 cmH2O PEEP, inflation time 0.4 s, rate 60 inflations/min, and VT was set at 7 ml/kg (maximum inflating pressure 50 cmH2O) (6).
-
2
2. Stepwise PEEP strategy (OLV), using PPV + volume-targeted mode as above except for commenced at 6 cmH2O PEEP at birth, and then increased by 2 cmH2O every 10 inflations until 20 cmH2O PEEP (maximum on ventilator). PEEP was then decreased every 10 inflations to 6 cmH2O PEEP. The lung was then transiently re-recruited with 10 inflations at PEEP 20 cmH2O (~170 s total duration) (6,11), prior to PPV at 8 cmH2O PEEP as per SI group for the remainder of the study.
PPV was initially applied with a fraction of inspired oxygen of 0.21 in all groups and then titrated to maintain SpO2 of 88–94%. Volume-targeted mode was adjusted to maintain a PaCO2 between 45 and 60 mm Hg after each arterial blood gas analysis using a standardized protocol (6,11,12). Hydration was maintained with continuous i.v. infusions and bolus fluid administered for persistent hypotension or metabolic acidosis. At 60 min of life, the animals were humanely euthanized with pentobarbitone.
Data Processing and Analysis
All continuous physiological measurements were recorded at 1,000 Hz, processed, and analyzed using Labchart 7 (AD Instruments, Sydney, New South Wales, Australia). Inflation pressure and PEEP during PPV were determined from the PAO waveform. VT was determined from integration of the flow wave using the known points of zero flow (PEEP and end-inflation). Dynamic compliance (Cdyn) was then calculated from the corresponding pressure change and VT values over the last stable 30 continuous inflations immediately preceding each arterial blood gas. The alveolar–arterial oxygen gradient (AaDO2) at each arterial gas was used to indicate arterial oxygenation.
Statistical Analysis
A sample size of eight was required to determine a difference in AaDO2 of 100 mm Hg and Cdyn of 0.1 ml/kg/cmH2O (power 0.8, alpha error 0.05). To account for potential errors in antenatal assessment of ewe parity, and the potential for smaller differences within the steroid group, at breeding 10 lambs were allocated to each ventilation strategy in the Control and Surfactant groups, and 13 in the steroid group. All data passed normality testing and, unless indicated, were analyzed with two-way measures ANOVA (using time and strategy as factors) and Sidak posttests. Statistical analysis was performed with GraphPad PRISM 6 (GraphPad Software, San Diego, CA) and a P <0.05 considered significant.
Statement of Financial Support
This study is supported by a National Health and Medical Research Council Project Grant, Canberra, Australia (Grant ID 1009287) and the Victorian Government Operational Infrastructure Support Program (Melbourne, Victoria, Australia). D.G.T. is supported by a National Health and Medical Research Council Clinical Career Development Fellowship (Grant ID 1053889). P.G.D. is supported by a National Health and Medical Research Council Program Grant (Grant ID 606789) and Practitioner Fellowship (Grant ID 556600).
Disclosure
The authors have no conflicts of interests to declare.
References
Jobe AH, Hillman N, Polglase G, Kramer BW, Kallapur S, Pillow J. Injury and inflammation from resuscitation of the preterm infant. Neonatology 2008;94:190–6.
Rojas-Reyes MX, Morley CJ, Soll R. Prophylactic versus selective use of surfactant in preventing morbidity and mortality in preterm infants. Cochrane Database Syst Rev 2012;3:CD000510.
Roberts D, Dalziel S. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev 2006:CD004454.
Lista G, Castoldi F, Cavigioli F, Bianchi S, Fontana P. Alveolar recruitment in the delivery room. J Matern Fetal Neonatal Med 2012;25:S(1):39–40.
te Pas AB, Siew M, Wallace MJ, et al. Establishing functional residual capacity at birth: the effect of sustained inflation and positive end-expiratory pressure in a preterm rabbit model. Pediatr Res 2009;65:537–41.
Tingay DG, Rajapaksa A, Zonneveld CE, et al. Spatiotemporal aeration and lung injury patterns are influenced by the first inflation strategy at birth. Am J Respir Cell Mol Biol 2016;54:263–72.
Dargaville PA, Tingay DG. Lung protective ventilation in extremely preterm infants. J Paediatr Child Health 2012;48:740–6.
Björklund LJ, Ingimarsson J, Curstedt T, et al. Manual ventilation with a few large breaths at birth compromises the therapeutic effect of subsequent surfactant replacement in immature lambs. Pediatr Res 1997;42:348–55.
te Pas AB, Siew M, Wallace MJ, et al. Effect of sustained inflation length on establishing functional residual capacity at birth in ventilated premature rabbits. Pediatr Res 2009;66:295–300.
Polglase GR, Tingay DG, Bhatia R, et al. Pressure- versus volume-limited sustained inflations at resuscitation of premature newborn lambs. BMC Pediatr 2014;14:43.
Tingay DG, Bhatia R, Schmölzer GM, Wallace MJ, Zahra VA, Davis PG. Effect of sustained inflation vs. stepwise PEEP strategy at birth on gas exchange and lung mechanics in preterm lambs. Pediatr Res 2014;75:288–94.
Tingay DG, Wallace MJ, Bhatia R, et al. Surfactant before the first inflation at birth improves spatial distribution of ventilation and reduces lung injury in preterm lambs. J Appl Physiol (1985) 2014;116:251–8.
Tingay DG, Polglase GR, Bhatia R, et al. Pressure-limited sustained inflation vs. gradual tidal inflations for resuscitation in preterm lambs. J Appl Physiol (1985) 2015;118:890–7.
Siew ML, Te Pas AB, Wallace MJ, et al. Positive end-expiratory pressure enhances development of a functional residual capacity in preterm rabbits ventilated from birth. J Appl Physiol (1985) 2009;106:1487–93.
Siew ML, Wallace MJ, Kitchen MJ, et al. Inspiration regulates the rate and temporal pattern of lung liquid clearance and lung aeration at birth. J Appl Physiol (1985) 2009;106:1888–95.
Wheeler K, Wallace M, Kitchen M, et al. Establishing lung gas volumes at birth: interaction between positive end-expiratory pressures and tidal volumes in preterm rabbits. Pediatr Res 2013;73:734–41.
Probyn ME, Hooper SB, Dargaville PA, McCallion N, Harding R, Morley CJ. Effects of tidal volume and positive end-expiratory pressure during resuscitation of very premature lambs. Acta Paediatr 2005;94:1764–70.
McCall KE, Davis PG, Owen LS, Tingay DG. Sustained lung inflation at birth: what do we know, and what do we need to know. Arch Dis Child Fetal Neonatal Ed 2016;101:F175–80
Schmölzer GM, Kumar M, Aziz K, et al. Sustained inflation versus positive pressure ventilation at birth: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed 2015;100:F361–8.
Tingay DG, Polglase GR, Bhatia R, et al. Pressure-limited sustained inflation vs. gradual tidal inflations for resuscitation in preterm lambs. J Appl Physiol (1985) 2015;118:890–7.
Hillman NH, Kemp MW, Miura Y, Kallapur SG, Jobe AH. Sustained inflation at birth did not alter lung injury from mechanical ventilation in surfactant-treated fetal lambs. PLoS One 2014;9:e113473.
Hillman NH, Kemp MW, Noble PB, Kallapur SG, Jobe AH. Sustained inflation at birth did not protect preterm fetal sheep from lung injury. Am J Physiol Lung Cell Mol Physiol 2013;305:L446–53.
Tingay DG, Lavizzari A, Zonneveld CE, et al. An individualized approach to sustained inflation duration at birth improves outcomes in newborn preterm lambs. Am J Physiol Lung Cell Mol Physiol 2015;309:L1138–49.
te Pas AB, Walther FJ. A randomized, controlled trial of delivery-room respiratory management in very preterm infants. Pediatrics 2007;120:322–9.
Lista G, Boni L, Scopesi F, et al.; SLI Trial Investigators. Sustained lung inflation at birth for preterm infants: a randomized clinical trial. Pediatrics 2015;135:e457–64.
Grasso C, Sciacca P, Giacchi V, et al. Effects of sustained lung inflation, a lung recruitment maneuver in primary acute respiratory distress syndrome, in respiratory and cerebral outcomes in preterm infants. Early Hum Dev 2015;91:71–5.
Klingenberg C, Sobotka KS, Ong T, et al. Effect of sustained inflation duration; resuscitation of near-term asphyxiated lambs. Arch Dis Child Fetal Neonatal Ed 2013;98:F222–7.
Polglase GR, Hooper SB, Gill AW, et al. Cardiovascular and pulmonary consequences of airway recruitment in preterm lambs. J Appl Physiol (1985) 2009;106:1347–55.
Sobotka KS, Hooper SB, Allison BJ, et al. An initial sustained inflation improves the respiratory and cardiovascular transition at birth in preterm lambs. Pediatr Res 2011;70:56–60.
Ikegami M, Jobe AH. Injury responses to different surfactants in ventilated premature lamb lungs. Pediatr Res 2002;51:689–95.
Tingay DG, Mills JF, Morley CJ, Pellicano A, Dargaville PA. The deflation limb of the pressure-volume relationship in infants during high-frequency ventilation. Am J Respir Crit Care Med 2006;173:414–20.
Dargaville PA, Rimensberger PC, Frerichs I. Regional tidal ventilation and compliance during a stepwise vital capacity manoeuvre. Intensive Care Med 2010;36:1953–61.
Tingay DG, Mills JF, Morley CJ, Pellicano A, Dargaville PA. Indicators of optimal lung volume during high-frequency oscillatory ventilation in infants. Crit Care Med 2013;41:237–44.
Zannin E, Ventura ML, Dellacà RL, et al. Optimal mean airway pressure during high-frequency oscillatory ventilation determined by measurement of respiratory system reactance. Pediatr Res 2014;75:493–9.
Pellicano A, Tingay DG, Mills JF, Fasulakis S, Morley CJ, Dargaville PA. Comparison of four methods of lung volume recruitment during high frequency oscillatory ventilation. Intensive Care Med 2009;35:1990–8.
Siew ML, Te Pas AB, Wallace MJ, et al. Surfactant increases the uniformity of lung aeration at birth in ventilated preterm rabbits. Pediatr Res 2011;70:50–5.
Ikegami M, Jobe AH, Newnham J, Polk DH, Willet KE, Sly P. Repetitive prenatal glucocorticoids improve lung function and decrease growth in preterm lambs. Am J Respir Crit Care Med 1997;156:178–84.
Polk DH, Ikegami M, Jobe AH, Sly P, Kohan R, Newnham J. Preterm lung function after retreatment with antenatal betamethasone in preterm lambs. Am J Obstet Gynecol 1997;176:308–15.
Smolich JJ, Kenna KR, Cheung MM. Onset of asphyxial state in nonrespiring interval between cord clamping and ventilation increases hemodynamic lability of birth transition in preterm lambs. J Appl Physiol (1985) 2015;118:675–83.
van Vonderen JJ, Hooper SB, Hummler HD, Lopriore E, te Pas AB. Effects of a sustained inflation in preterm infants at birth. J Pediatr 2014;165:903–8.e1.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tingay, D., Rajapaksa, A., McCall, K. et al. The interrelationship of recruitment maneuver at birth, antenatal steroids, and exogenous surfactant on compliance and oxygenation in preterm lambs. Pediatr Res 79, 916–921 (2016). https://doi.org/10.1038/pr.2016.25
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2016.25
This article is cited by
-
Oscillatory mechanics at birth for identifying infants requiring surfactant: a prospective, observational trial
Respiratory Research (2021)
-
Feasibility of combining two individualized lung recruitment maneuvers at birth for very low gestational age infants: a retrospective cohort study
BMC Pediatrics (2020)
-
Plasma proteomics reveals gestational age-specific responses to mechanical ventilation and identifies the mechanistic pathways that initiate preterm lung injury
Scientific Reports (2018)
-
Efficacy of a new technique – INtubate-RECruit-SURfactant-Extubate – “IN-REC-SUR-E” – in preterm neonates with respiratory distress syndrome: study protocol for a randomized controlled trial
Trials (2016)