Abstract
Background
This study aimed at comparing cardiorespiratory stability during total liquid ventilation (TLV)—prior to lung aeration—with conventional mechanical ventilation (CMV) in extremely preterm lambs during the first 6 h of life.
Methods
23 lambs (11 females) were born by c-section at 118–120 days of gestational age (term = 147 days) to receive 6 h of TLV or CMV from birth. Lung samples were collected for RNA and histology analyses.
Results
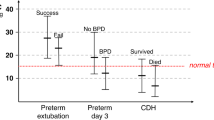
The lambs under TLV had higher and more stable arterial oxygen saturation (p = 0.001) and cerebral tissue oxygenation (p = 0.02) than the lambs in the CMV group in the first 10 min of transition to extrauterine life. Although histological assessment of the lungs was similar between the groups, a significant upregulation of IL-1a, IL-6 and IL-8 RNA in the lungs was observed after TLV.
Conclusions
Total liquid ventilation allowed for remarkably stable transition to extrauterine life in an extremely preterm lamb model. Refinement of our TLV prototype and ventilation algorithms is underway to address specific challenges in this population, such as minimizing tracheal deformation during the active expiration.
Impact
-
Total liquid ventilation allows for remarkably stable transition to extrauterine life in an extremely preterm lamb model.
-
Total liquid ventilation is systematically achievable over the first 6 h of life in the extremely premature lamb model.
-
This study provides additional incentive to pursue further investigation of total liquid ventilation as a transition tool for the most extreme preterm neonates.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Lee, C. D., Nelin, L. & Foglia, E. E. Neonatal resuscitation in 22-week pregnancies. N. Engl. J. Med. 386, 391–393 (2022).
Kumar, N., Akangire, G., Sullivan, B., Fairchild, K. & Sampath, V. Continuous vital sign analysis for predicting and preventing neonatal diseases in the twenty-first century: big data to the forefront. Pediatr. Res. 87, 210–220 (2020).
Lara-Cantón, I. et al. Oxygen supplementation during preterm stabilization and the relevance of the first 5 min after birth. Front. Pediatr. 8, 12 (2020).
Ballabh, P. Intraventricular hemorrhage in premature infants: mechanism of disease. Pediatr. Res. 67, 1–8 (2010).
Younge, N. et al. Survival and neurodevelopmental outcomes among periviable infants. N. Engl. J. Med 376, 617–628 (2017).
Stritzke, A. et al. Use and timing of surfactant administration: impact on neonatal outcomes in extremely low gestational age infants born in Canadian Neonatal Intensive Care Units. J. Matern Fetal Neonatal Med. 31, 2862–2869 (2018).
Sindelar, R., Nakanishi, H., Stanford, A. H., Colaizy, T. T. & Klein, J. M. Respiratory management for extremely premature infants born at 22 to 23 weeks of gestation in proactive centers in Sweden, Japan, and USA. Semin. Perinatol. 46, 151540 (2022).
Weisz, D. E. et al. Duration of and trends in respiratory support among extremely preterm infants. Arch. Dis. Child Fetal Neonatal Ed. 106, 286–291 (2021).
Hirata, K. et al. Longitudinal impairment of lung function in school-age children with extremely low birth weights. Pediatr. Pulmonol. 52, 779–786 (2017).
Mushtaq, A. Progress needed in bronchopulmonary dysplasia. Lancet Respir. Med. 7, 300–301 (2019).
Shukla, V. V. et al. Hospital and neurodevelopmental outcomes in nano-preterm infants receiving invasive vs noninvasive ventilation at birth. JAMA Netw. Open 5, e2229105 (2022).
Foust, R. 3rd et al. Liquid assisted ventilation: an alternative ventilatory strategy for acute meconium aspiration injury. Pediatr. Pulmonol. 21, 316–322 (1996).
Sarkar, S., Paswan, A. & Prakas, S. Liquid ventilation. Anesth. Essays Res. 8, 277–282 (2014).
Klingstedt, C. et al. The influence of body position and differential ventilation on lung dimensions and atelectasis formation in anaesthetized man. Acta Anaesthesiol. Scand. 34, 315–322 (1990).
Stavis, R. L., Wolfson, M. R., Cox, C., Kechner, N. & Shaffer, T. H. Physiologic, biochemical, and histologic correlates associated with tidal liquid ventilation. Pediatr. Res. 43, 132–138 (1998).
Cox, C., Stavis, R. L., Wolfson, M. R. & Shaffer, T. H. Long-term tidal liquid ventilation in premature lambs: physiologic, biochemical and histological correlates. Biol. Neonate 84, 232–242 (2003).
Degraeuwe, P. L. et al. Conventional gas ventilation, liquid-assisted high-frequency oscillatory ventilation, and tidal liquid ventilation in surfactant-treated preterm lambs. Int. J. Artif. Organs 23, 754–764 (2000).
Jackson, J. C., Standaert, T. A., Truog, W. E. & Hodson, W. A. Full-tidal liquid ventilation with perfluorocarbon for prevention of lung injury in newborn non-human primates. Artif. Cells Blood Substit. Immob. Biotechnol. 22, 1121–1132 (1994).
Wolfson, M. R., Greenspan, J. S., Deoras, K. S., Rubenstein, S. D. & Shaffer, T. H. Comparison of gas and liquid ventilation: clinical, physiological, and histological correlates. J. Appl. Physiol. (1985) 72, 1024–1031 (1992).
Curtis, S. E., Fuhrman, B. P., Howland, D. F., DeFrancisis, M. & Motoyama, E. K. Cardiac output during liquid (perfluorocarbon) breathing in newborn piglets. Crit. Care Med. 19, 225–230 (1991).
Bagnoli, P., Acocella, F., Di Giancamillo, M., Fumero, R. & Costantino, M. L. Finite element analysis of the mechanical behavior of preterm lamb tracheal bifurcation during total liquid ventilation. J. Biomech. 46, 462–469 (2013).
Robert, R., Micheau, P. & Walti, H. A supervisor for volume-controlled tidal liquid ventilator using independent piston pumps. Biomed. Signal Process. Control 2, 267–274 (2007).
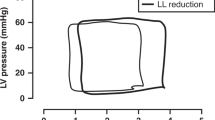
Sage, M. et al. Assessing the impacts of total liquid ventilation on left ventricular diastolic function in a model of neonatal respiratory distress syndrome. PloS One 13, e0191885 (2018).
Sage, M. et al. Effect of low versus high tidal-volume total liquid ventilation on pulmonary inflammation. Front. Physiol. 11, 603 (2020).
See, W. et al. Air distribution within the lungs after total liquid ventilation in a neonatal ovine model. Respir. Physiol. Neurobiol. 290, 103666 (2021).
Morin, C. et al. Conventional vs high-frequency ventilation for weaning from total liquid ventilation in lambs. Respir. Physiol. Neurobiol. 299, 103867 (2022).
Percie du Sert, N. et al. The ARRIVE guidelines 2.0: updated guidelines for reporting animal research. J. Physiol. 598, 3793–3801 (2020).
Skoll, A. et al. No. 364-antenatal corticosteroid therapy for improving neonatal outcomes. J. Obstet. Gynaecol. Can. 40, 1219–1239 (2018).
Mychaliska, G. B. et al. Operating on placental support: the ex utero intrapartum treatment procedure. J. Pediatr. Surg. 32, 227–230 (1997). discussion 230-221.
El-Sabbagh, A. M. et al. Cerebral oxygenation of premature lambs supported by an artificial placenta. ASAIO J. 64, 552–556 (2018).
Robert, R., Micheau, P. & Walti, H. Optimal expiratory volume profile in tidal liquid ventilation under steady state conditions, based on a symmetrical lung model. ASAIO J. 55, 63–72 (2009).
Sage, M. et al. Perflubron distribution during transition from gas to total liquid ventilation. Front. Physiol. 9, 1723 (2018).
Hillman, N. H. et al. Airway injury from initiating ventilation in preterm sheep. Pediatr. Res. 67, 60–65 (2010).
Harijith, A. K. & Bhandari, V. in Bronchopulmonary Dysplasia (ed V. Bhandari) p. 3–26 (Springer International Publishing, 2016).
Schmittgen, T. D. & Livak, K. J. Analyzing real-time PCR data by the comparative C(T) method. Nat. Protoc. 3, 1101–1108 (2008).
Wickham, H. ggplot2: Elegant Graphics for Data Analysis. (Springer, 2016).
Nagin, D. S. Analyzing developmental trajectories: a semiparametric, group-based approach. Psychol. Methods 4, 139–157 (1999).
Shaffer, T. H., Tran, N., Bhutani, V. K. & Sivieri, E. M. Cardiopulmonary function in very preterm lambs during liquid ventilation. Pediatr. Res. 17, 680–684 (1983).
Samson, N., Fortin-Pellerin, E. & Praud, J. P. The contribution of ovine models to perinatal respiratory physiology. Front Biosci. (Landmark Ed.) 23, 1195–1219 (2018).
Albertine, K. H. Utility of large-animal models of BPD: chronically ventilated preterm lambs. Am. J. Physiol. Lung Cell Mol. Physiol. 308, L983–L1001 (2015).
Oei, J. L. et al. Outcomes of oxygen saturation targeting during delivery room stabilisation of preterm infants. Arch. Dis. Child. Fetal Neonatal Ed. 103, F446–F454 (2018).
Bagnoli, P. et al. Effect of repeated induced airway collapse during total liquid ventilation. ASAIO J. 53, 549–555 (2007).
Ancora, G. et al. Evidence-based clinical guidelines on analgesia and sedation in newborn infants undergoing assisted ventilation and endotracheal intubation. Acta Paediatr. 108, 208–217 (2019).
McPherson, C., Ortinau, C. M. & Vesoulis, Z. Practical approaches to sedation and analgesia in the newborn. J. Perinatol. 41, 383–395 (2021).
McDonagh, P. et al. Perflubron emulsion reduces inflammation during extracorporeal circulation. J. Surg. Res. 99, 7–16 (2001).
Kaisers, U., Kelly, K. P. & Busch, T. Liquid ventilation. Br. J. Anaesth. 91, 143–151 (2003).
Jiang, L., Feng, H., Chen, X., Liang, K. & Ni, C. Low tidal volume reduces lung inflammation induced by liquid ventilation in piglets with severe lung injury. Artif. Organs 41, 440–445 (2017).
Kohlhauer, M. et al. A new paradigm for lung-conservative total liquid ventilation. EBioMedicine 52, 102365 (2020).
Eichenwald, C., Dysart, K., Zhang, H. & Fox, W. Neonatal partial liquid ventilation for the treatment and prevention of bronchopulmonary dysplasia. NeoReviews 21, e238–e248 (2020).
Micheau, P. et al. Liquid ventilator and method to induce tidal liquid ventilation and/or hyperthermia, filed April 12, 2019 in Canada, (Patent application PCT/CA2019/050450).
Acknowledgements
The authors would like to thank Samuel Lemaire-Paquette from the biostatistics department of the Université de Sherbrooke Hospital Research Center for help with the statistical analysis and review of the manuscript.
Funding
This research was funded by the Center de recherche du CHUS, Foundation of Stars, Quebec Respiratory Health Research Network, Fonds de Recherche en Santé du Québec, the Natural Sciences and Engineering Research Council of Canada, and the Canadian Institutes of Health Research.
Author information
Authors and Affiliations
Contributions
Substantial contributions to the conception and design, acquisition of data, or analysis and interpretation of data: C.M., É.S., J.P.P., B.C., P.L., W.S., M.S., R.I., C.N., N.S., S.M., S.T., P.M., and E.F.P. Drafting the article or revising it critically for important intellectual content: C.M., E.F.P., J.P.P., and P.M. Final approval of the version to be published: all authors.
Corresponding author
Ethics declarations
Competing interests
P.M. declares to be a co-inventor of patents on liquid ventilation (US patents #7,726,311 B2; US patent 2016/0,271,348 A1; US patent 2021/0,077,759 A1; European patent 21305533.8). P.M. is a shareholder of a start-up company dedicated to the commercialization of a liquid ventilator for ultra-fast hypothermia induction after cardiac arrest (Orixha). The remaining authors declare no conflicts of interest of any sort.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Morin, C., Simard, É., See, W. et al. Total liquid ventilation in an ovine model of extreme prematurity: a randomized study. Pediatr Res 95, 974–980 (2024). https://doi.org/10.1038/s41390-023-02841-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02841-6