Abstract
Background:
Adults with the apolipoprotein E (APOE) gene alleles e4 and e2 are at high risk of poor neurological outcome after brain injury. The e4 allele has been associated with cerebral palsy (CP), and the e2 allele has been associated with worse neurological outcome with congenital heart disease. This study was done to test the hypothesis that the APOE genotype is associated with outcome among neonates who survive after hypoxic–ischemic encephalopathy (HIE).
Methods:
We conducted a cohort study of infants who survived HIE and had 18–22 mo standardized neurodevelopmental evaluations to assess associations between disability and the APOE genotypes e3/e3, e4/–, and e2/–.
Results:
A total of 139 survivors were genotyped. Of these, 86 (62%) were of the e3/e3, 41 (29%) were of the e4/–, and 14 (10%) were of the e2/– genotypes. One hundred and twenty-nine infants had genotype and follow-up data; 26% had moderate or severe disabilities. Disability prevalence was 30 and 19% among those with and without the e3/e3 genotype, 25 and 26% among those with and without the e2 allele, and 18 and 29% among those with and without the e4 allele, respectively. None of the differences were statistically significant. CP prevalence was also similar among genotype groups.
Conclusion:
Disability was not associated with the APOE genotype in this cohort of HIE survivors.
Similar content being viewed by others
Main
Neonatal hypoxic–ischemic encephalopathy (HIE) involves complex processes of energy depletion, inflammation, necrosis, apoptosis, and altered development of connectivity after injury (1,2,3,4). Clinical trials of therapeutic hypothermia have consistently demonstrated reductions in risk of death or impairment; however, the incidence of impairment among surviving cooled infants in clinical trials has consistently been between 40 and 50% (5). Uncovering associations between genetic variants and risk of adverse outcome after hypoxic–ischemic injury could lead to identification of mechanisms that could be targeted to further improve outcomes.
Apolipoprotein E (APOE) is the primary apolipoprotein produced in the brain (6). Three allelic variants of the APOE gene, e2, e3, and e4, deriving from two single-nucleotide polymorphisms—rs429358 (thymine, T; or cytosine, C), and rs7412(C or T)—result in single amino acid changes in the APOE protein (7,8,9). Presence of the APOE e4 allele has been strongly associated with increased risk for Alzheimer’s disease and poor neurological outcome after traumatic brain injury and brain hemorrhage among adults (9,10,11). The e4 allele has also been associated with persistence of the cognitive decline seen in adult patients following cardiac bypass surgery (12).
Previous case–control studies in children with cerebral palsy (CP), a morbidity that occasionally follows HIE, have demonstrated associations between the APOE e4 allele and increased severity of CP, microcephaly, and seizures (13,14). These studies included both term and preterm infants with various forms of CP. In studies assessing APOE genotype and outcome among children with trauma and heart surgery, the e4 allele has been associated with CP and worse neurodevelopmental outcome (15). The e2 allele has been associated with an increased risk for CP, worse neurodevelopmental outcome, and behavior problems among infants with congenital heart disease (16,17). APOE e3 is the most common allele, and e3/e3 homozygous adults are more likely to survive and have better functional outcome following cardiopulmonary resuscitation compared with adults with the less common minor alleles e4 and e2 (18,19).
No study has reported whether neurological outcome, including CP, among infants with moderate to severe neonatal HIE who survive to discharge is associated with the common variants in the APOE gene associated with neuropathology in adults and CP in younger patients. Because of the strong association between APOE alleles and neurological outcome after injury in older populations, and the suggestive associations between CP and e2 and e4 alleles in pediatric patients following an array of previous conditions, we conducted a cohort study to assess association between APOE genotypes and neurological and neurodevelopmental status at 18–22 mo among neonatal HIE survivors. We hypothesized that among 18- to 22-mo survivors of HIE, prevalence of disability would be lowest among those with the e3/e3 genotype and higher among infants carrying the APOE e2 or APOE e4 allele. We also included a secondary association analysis of prevalence of CP for APOE e3/e3 homozygotes and carriers of the e2 and e4 alleles. Because cooling has an impact on outcome after HIE, we also conducted an exploratory analysis to assess whether or not cooling influenced associations between APOE genotype and outcome.
Results
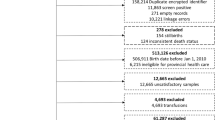
This candidate gene association study enrolled 147 subjects who were participating in the Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network’s (hereafter, “Network”) randomized trial of Hypothermia for neonatal HIE or the Network’s study of amplitude-integrated electroencephalography (aEEG) in infants with neonatal HIE (20,21). The numbers of infants who (i) were enrolled in the candidate gene study from the two main studies, (ii) were lost to follow-up, and (iii) died before ascertaining the 18- to 22-mo outcome are depicted in Figure 1 . Eight (5.4%) infants died before discharge—six within the first 4 postnatal days, one at 8 d, and one at 19 d—and were not included in the association analyses. One hundred and thirty-nine survivors had DNA samples obtained. Ten (7.2%) infants did not have complete information to define the primary outcome. One hundred and twenty-nine infants ultimately had successful DNA extraction, underwent APOE genotyping, and survived to have adequate information from follow-up evaluations at 18–22 mo to determine the primary outcome.
Number of infants enrolled in the apolipoprotein E (APOE) candidate gene study from each of the two primary Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network studies. Follow-up is defined as nonmissing primary outcome (moderate or severe disability) among survivors. One infant was lost but was assigned primary outcome through adjudication; data are missing for other follow-up outcomes. aAmong amplitude-integrated electroencephalography (aEEG) infants, 47 infants were followed, but we were only able to assign primary outcome to only 46 of them (one had the Bayley examination but was missing cerebral palsy and hearing data). bTen infants did not have adequate information to allow determination of the primary outcome. RCT, randomized controlled trial.
The APOE study cohort appeared to be representative of the infants enrolled in the Network’s Hypothermia and aEEG studies who survived to discharge and follow-up. Survivors in the APOE study who were successfully genotyped, including the 10 who did not have adequate information to define the primary outcome, did not differ in race/ethnicity or intrapartum complications relative to survivors from the aEEG and Hypothermia studies who were not enrolled in the APOE genotype study. There was good representation of infants who were classified as African American, Caucasian, and Hispanic in the APOE and the nongenotyped Hypothermia and aEEG study populations ( Table 1 ). Infants in the APOE study cohort had higher Apgar scores at 10 min and more of them were cooled compared with infants from the two Network studies who were not enrolled in the APOE study (designated as “other survivors” in Table 1 ); however, there was no difference in the percentage of infants with moderate (81 vs. 80%) or severe (19 vs. 20%) encephalopathy in the two groups ( Table 1 ).
Genotype Frequencies
Among the 139 infants who survived to discharge and had APOE genotypes determined, 10% carried an e2 and 29%, an e4 allele. Moreover, 62% had the APOE e3/e3 genotype. Surviving African American infants had a higher prevalence of an e4 allele and a lower prevalence of the e3/e3 genotype than either Caucasian or Hispanic infants ( Table 2 ).
Prevalence of Outcome for Each Genotype
Twenty-six percent of the infants in the APOE study who survived to discharge had the primary outcome, namely, moderate or severe disability. Only two infants had moderate disability, and the remaining infants were severely disabled. The prevalence of moderate or severe disability among infants with the APOE e3/e3 genotype did not differ significantly from those without this hypothesized protective genotype, nor did the prevalence of the primary outcome differ among those with and without the hypothesized risk alleles e4 or e2 ( Figure 2 ). In addition, no differences were found when separate analyses were carried out for infants of different races, with moderate or severe initial encephalopathy, or for infants cooled or not cooled.
Prevalence of moderate/severe disability in infants of different genotypes. For each genotype, white bars denote the percentage of those with the genotype surviving with moderate to severe disability and black bars denote the percentage without the genotype surviving with moderate to severe disability. Among 81 infants with the apolipoprotein E (APOE) e3/e3 genotype and follow-up, prevalence of the primary outcome was 30%, and among the 48 infants not homozygous for e3/e3, prevalence was 19% (P = 0.21). Among 12 infants with the APOE e2 allele, the prevalence of primary outcome was 25%, compared with 26% among the 117 infants without the e2 allele (P = 1.00). Among those with the APOE e4 allele (n = 38), the prevalence of the primary outcome was 18%, compared with 29% among the 91 without the e4 allele (P = 0.27).
Similar to what was noted with the primary outcome, the prevalence of Bayley II Mental Developmental Index (MDI) <70 did not differ in the groups (i) with and without the APOE e3/e3 genotype or (ii) with and without an e4 or e2 allele ( Figure 3 ). The prevalence of moderate or severe CP was not significantly different between infants with and those without the e3/e3 genotype or between those with and those without an e4 or e2 allele ( Figure 4 ).
Prevalence of Mental Developmental Index (MDI) <70 among infants of different genotypes. For each genotype, white bars denote the percentage of those with the genotype surviving with MDI <70, and black bars denote the percentage without the genotype surviving with MDI <70. Among 79 infants with the apolipoprotein E (APOE) e3/e3 genotype and follow-up, prevalence of MDI <70 was 28%, and among the 49 infants not homozygous for e3, prevalence was 16% (P = 0.20). Among 13 infants with the APOE e2 allele, the prevalence of primary outcome was 15%, compared with 24% among the 115 infants without the e2 allele (P = 0.73). Among those with the APOE e4 allele (n = 38), the prevalence of the primary outcome was 16%, compared with 27% among the 90 without the e4 allele (P = 0.25).
Prevalence of moderate to severe cerebral palsy (CP) among infants of different genotypes. For each genotype, white bars denote the percentage of those with the genotype surviving with moderate to severe CP, and black bars denote the percentage without the genotype surviving with moderate to severe CP. Among 80 infants with the apolipoprotein E (APOE) e3/e3 genotype and follow-up, prevalence of moderate to severe CP was 14%, and among the 48 infants not homozygous for APOE e3, prevalence was 13% (P = 1.00). Among 12 infants with the APOE e2 allele, the prevalence of moderate to severe CP was 17%, compared with 13% among the 116 infants without the e2 allele (P = 0.66). Among those with the APOE e4 allele (n = 38), the prevalence of moderate to severe CP was 11%, compared with 14% among the 90 without the e4 allele (P = 0.78).
Discussion
This report is the first to test associations between APOE genotypes and neurological outcome in a cohort limited to term infants who survived to discharge after neonatal HIE. Previous case–control studies of pediatric populations reporting association between APOE genotypes and CP, a common outcome after HIE, did not target assessment of only infants with neonatal hypoxic–ischemic injury (13,14). Our results demonstrate no association between APOE genotype and moderate or severe disability, or specifically associations with CP, in this more restrictive injury phenotype, as well as demonstrating no modification from use of hypothermia.
Genetic epidemiology strongly supports associations between the e4 allele and both Alzheimer’s disease and poor prognosis after neurological injury. The association between the e4 allele and Alzheimer’s disease was uncovered using traditional linkage analysis and family studies (10). The association is seen even when unbiased approaches tested the e4 allele among millions of single-nucleotide polymorphisms throughout the genome for association with Alzheimer’s disease (P = 2.52 × 10–53) (22).
Although the genetic epidemiology supporting links between APOE genotype and Alzheimer’s disease is strong, tests of association between APOE e4 allele and CP among children have not been as consistent. Two recent reports (23,24) of subjects with CP have not found the strengths of association found in the two earlier reports of association between CP and APOE genotype (13,14). Wu et al. (23) reported results of association studies between candidate gene single-nucleotide polymorphisms and CP from a diverse, general population of 334,333 newborn infants from the Kaiser Permanente Health System, inclusive of healthy and sick infants. From this cohort, 138 cases of various types of CP and 165 controls were compared. APOE e4/e3 heterozygotes were associated with CP compared with e3/e3 homozygotes (odds ratio: 1.7 (95% confidence interval: 1.01–2.9)). In the second, more recent Australian case–control study of children >5 y of age with CP, among 55 children with diplegia compared with 281 controls, the odds ratio for CP was 1.87 (95% confidence interval: 1.03–3.40) for the e4/e3 compared with the e3/e3 genotypes; however, among children with quadriplegia (n = 40) compared with controls (n = 249), odds ratio for CP for e2/e3 heterozygotes compared with e3/e3 homozygotes was 0.23 (95% confidence interval: 0.05–1.00) (24). The authors of both studies concluded that due to the multiple comparisons with dozens of candidate single-nucleotide polymorphisms, neither could claim that the associations with APOE genotype were significant; however, both were cautious in eliminating the possibility of genetic links with risk of CP, citing the importance of the potential impact of variation in injury type or risk phenotype as well as variation in the CP phenotype outcomes on their analyses (23,24). A third study, also among a cohort of children with multiple CP phenotypes with a variety of potential etiologies, has found no associations between APOE genotypes and severity of CP, although prevalence of active epilepsy was higher among children with the e4 allele (25).
Mechanisms for the associations between APOE genotypes and Alzheimer’s disease and poor outcomes after trauma and stroke in older populations are not definitively known. For Alzheimer’s disease, the leading hypothesis is that protein variations caused by the different genotypes lead to differential effects of APOE on amyloid-β accumulation in the brain and its vasculature (9). For the associations with poor outcome after stroke or trauma, there is less certainty (26). Postulated mechanisms associated with the e4 allele in animal studies of various ischemic and traumatic brain injuries include less-efficient transport of lipids important for repair and subsequent synaptogenesis (27), worse protection against oxidative injury (28), and greater degree of brain inflammation (29,30). Because oxidative injury, derangements in subsequent connectivity, and inflammatory injury are all potential contributors to poor outcomes post hypoxic–ischemic injury (4), the e4 allele’s association with these mechanisms raises suspicions that it would be similarly implicated in worse outcomes after HIE. Our results in a small cohort of infants surviving to discharge after neonatal HIE with well-defined outcome phenotypes do not support this hypothesis.
Prevalence of moderate to severe disability in our small study cohort was 18% for those with the e4 allele and 29% for those without the e4 allele. This difference was not significant. There is some speculation, however, that the e4 allele may be associated with benefits in younger populations. In a study assessing association between the presence of the e4 allele and the severity of CP in a population of children with CP (61% preterm), there was a trend suggesting that infants with one e4 allele were more likely to be in the low-severity group (31). Among children born and raised in poor areas of Mexico and Brazil, the e4 allele has been associated with better 2 y and later outcomes (6,32). If the APOE variants are truly protective earlier but contribute to risk of Alzheimer’s later in life, the gene may obey the principle of antagonistic pleiotropy, such that despite potentially detrimental effects later in life, certain polymorphisms may be beneficial during critical periods of development when faced with environmental stress (6,26). Of note, population prevalence of the e4 allele in our racially mixed study population (29%) is higher than that reported from adult cohorts from multiple regions and ethnicities (2–40%) (33,34). Evidence points to APOE as a critical glial factor in synaptogenesis, which may also subsequently affect long-term synaptic plasticity (35). Wright et al. (6) postulate that if e4 promotes myelination, synaptogenesis, or other fatty acid/cholesterol-mediated processes associated with neurodevelopment, then the higher Bayley scores noted among the children in his study cohort may be due to protection against the adverse effects of neurotoxins on these processes by a mechanism related to as-yet-unknown differences in function in the peptide produced from the APOE gene with the e4 allele. An intestinal health–related hypothesis has also emerged from a study of Brazilian indigent children with below-median height-for-age z-scores supplemented with retinol and zinc or both, plus glutamine supplementation. In the measures of intestinal barrier function and cognitive outcome, children lacking the e4 allele exhibited negative Pearson correlations between the change in lactulose-to-mannitol ratio over 4 mo and verbal learning and nonverbal intelligence, regardless of receiving any of the three interventions. The authors speculate that there is an interaction between APOE genotype and gut trophic factors, which translates into better nutritional, and ultimately, neurocognitive, outcomes (36). Accumulation of larger cohorts of infants with HIE and available genetic samples and accurate neurological and neurodevelopmental outcome phenotypes are needed to test this finding.
We have used our study population to get the most precise estimate possible of associations between APOE genotypes and alleles and outcomes for term infants with HIE. Although our study is unique in that it included only infants with HIE, the small study population allowed only a limited number of exploratory tests of association and has limited statistical power to detect significant effects (37,38). Although the estimate may be precise, our findings should be interpreted with caution. A two-to-three-times-larger study population with similar proportions of allele frequencies and outcome prevalence among cases and controls would be needed to demonstrate significance with 90% power (39). In addition, the importance of accuracy of injury as well as outcome phenotype to studies of genetic association cannot be underestimated. Even though we believe that the eligibility criteria based on neonatal encephalopathy is a strength of our study, some infants in the study cohort had acute, sentinel events consistent with sudden acute hypoxic–ischemic injury such as umbilical cord prolapse or uterine rupture, whereas others had encephalopathy at birth without perinatal sentinel events or with multiple intrapartum complications (20). Our study also includes only surviving infants. Our rationale for this is in part a practical one, because we did not ask consent for collecting samples for research DNA analysis in the acute first days and weeks of hospitalization and because of our focus on APOE genetic variance playing a role in recovery from moderate to severe injury. Significant differences may have been found in a larger cohort of patients and if samples were collected at birth so that all infants who died, many of whom had severe encephalopathy, could have been included in the analyses. APOE may have more to do with susceptibility to initial injury rather than recovery from that initial injury and initial recovery.
Although our exploratory study did not reveal significant associations between APOE genotypes and outcomes after HIE, the lower prevalence of CP and MDI <70 among infants with the e4 allele is of interest, which requires testing in much larger cohorts with both accurate initial neonatal HIE and follow-up neurologic and neurodevelopmental phenotypes.
Conclusion
In this small cohort of surviving infants with neonatal HIE, there was no evidence for an association of the APOE e3/e3 genotype with improved neurodevelopmental outcome at 18–22 mo or for an association between presence of either the APOE e2 or e4 allele and increased risk for neurodevelopmental disability. Additional studies are required to confirm these results and explore other potential genetic factors that may influence outcome after neonatal HIE.
Methods
Surviving infants with moderate or severe HIE enrolled in the Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network’s therapeutic Hypothermia study (20) and in the Network study of utility of aEEG for prediction of outcome among infants with HIE were eligible (21). Eligibility criteria for these studies included gestational age of at least 36 wk and birth weight greater than 1,800 g. Neonatal HIE was defined as described in the Hypothermia and aEEG studies. Eligibility criteria included a pH of 7.0 or less or a base deficit of 16 mmol/l or more in cord blood or blood gas during the first hour after birth. If, during this interval, the pH was between 7.01 and 7.15, base deficit was between 10 and 15.9 mmol/l, or blood gas reading was not available, additional criteria were required. These included history of an acute perinatal event (e.g., late or variable decelerations, cord prolapse, cord rupture, uterine rupture, maternal trauma, hemorrhage, or cardiorespiratory arrest) and either a 10-min Apgar score of 5 or less or the use of assisted ventilation initiated at birth and continued for at least 10 min. Once these criteria were met, all infants underwent a standardized neurological examination performed by a certified examiner. Infants were candidates for the study when moderate or severe encephalopathy or seizures were present (20,21). Outcome at 18–22 mo was assessed by a standard neurological examination and the Bayley Scales of Infant Development II were applied by certified examiners (20,21). Severe disability, in the Hypothermia study and in this study, was defined as any one of the following: MDI < 70, Gross Motor Function Classification System 3–5 (equivalent to moderate/severe CP), hearing impairment requiring aids, or bilateral blindness. Moderate disability was defined as Bayley II MDI 70–84 plus any one of the following: Gross Motor Function Classification System 2, hearing impairment with no aids, or seizure disorder requiring anticonvulsants. The primary outcome for the association analyses was presence of either moderate or severe disability (20,21).
For DNA collection and analysis, a buccal swab was used to collect DNA before hospital discharge or at follow-up. APOE genotypes were determined using restriction fragment-length polymorphism measurements. DNA extraction and APOE genotyping were conducted at Duke University (Durham, NC) . DNA was extracted from the buccal swabs and first amplified using oligonucleotide primers F4 (5′-ACAGAATTCGCCCCGGCCTGGTACAC-3′) and F6 (5′-TAAGCTTGGCACGGCTGTCCAAGGA-3′). Amplification products of APOE were then subjected to restriction enzyme HhaI digestion, as described by Hixson and Vernier (40).
Because not every family whose infant was enrolled in the Network’s Hypothermia or aEEG studies was approached for consent for the APOE genotyping study from the time of initiation of the Hypothermia or aEEG study, we compared demographics and perinatal characteristics and events between those enrolled in the genotyping study and those who were not. We used χ2 for categorical variables and t-tests to compare the two groups.
For the primary analyses, we compared prevalence of the primary outcome—moderate or severe disability—among infants with and without the APOE e3/e3 genotype and with or without any e2 or e4 allele by Fisher’s exact test. We also compared prevalence of the components of the primary outcomes—MDI < 70 and moderate/severe CP (Gross Motor Function Classification System 3–5)—among infants (i) with and without the APOE e3/e3 genotype and (ii) with and without the e2 or e4 allele. In separate exploratory analyses, we compared prevalence of outcomes for infants with and without the e3/e3 genotype or alleles (i) among infants of different races, to account for potential allele frequency differences among races, (ii) among infants with different levels of encephalopathy at enrollment, and (iii) among infants cooled and those not cooled.
Informed consent was obtained, and the study was approved by all sites’ Institutional Review Boards (the list of sites is included in the Supplementary Appendix online), including the data-coordinating center, RTI International (Research Triangle Park, NC). Because genetic information was generated, a Certificate of Confidentiality was obtained for this study by the data-coordinating center.
Statement of Financial Support
The National Institute of Child Health and Human Development (NICHD) Neonatal Research Network (NRN) funded this trial. Principal Investigators and Research Coordinators received salary support as part of the Network grants at each site, and grant numbers are individually listed in the Supplemental Appendix online. No authors have financial ties to products used in the study or potential/perceived conflicts of interest to disclose.
References
McQuillen PS, Ferriero DM . Selective vulnerability in the developing central nervous system. Pediatr Neurol 2004;30:227–35.
Stone BS, Zhang J, Mack DW, Mori S, Martin LJ, Northington FJ . Delayed neural network degeneration after neonatal hypoxia-ischemia. Ann Neurol 2008;64:535–46.
Miller SP, Ferriero DM . From selective vulnerability to connectivity: insights from newborn brain imaging. Trends Neurosci 2009;32:496–505.
Northington FJ, Chavez-Valdez R, Martin LJ . Neuronal cell death in neonatal hypoxia-ischemia. Ann Neurol 2011;69:743–58.
Higgins RD, Raju T, Edwards AD, et al.; Eunice Kennedy Shriver National Institute of Child Health and Human Development Hypothermia Workshop Speakers and Moderators. Hypothermia and other treatment options for neonatal encephalopathy: an executive summary of the Eunice Kennedy Shriver NICHD workshop. J Pediatr 2011;159:851–858.e1.
Wright RO, Hu H, Silverman EK, et al. Apolipoprotein E genotype predicts 24-month bayley scales infant development score. Pediatr Res 2003;54:819–25.
Mahley RW, Rall SC Jr . Apolipoprotein E: far more than a lipid transport protein. Annu Rev Genomics Hum Genet 2000;1:507–37.
Kim J, Basak JM, Holtzman DM . The role of apolipoprotein E in Alzheimer’s disease. Neuron 2009;63:287–303.
Verghese PB, Castellano JM, Holtzman DM . Apolipoprotein E in Alzheimer’s disease and other neurological disorders. Lancet Neurol 2011;10:241–52.
Corder EH, Saunders AM, Strittmatter WJ, et al. Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer’s disease in late onset families. Science 1993;261:921–3.
Zhou W, Xu D, Peng X, Zhang Q, Jia J, Crutcher KA . Meta-analysis of APOE4 allele and outcome after traumatic brain injury. J Neurotrauma 2008;25:279–90.
Tardiff BE, Newman MF, Saunders AM, et al. Preliminary report of a genetic basis for cognitive decline following cardiac operations. Ann of Thorac Surg 1997;64:715–720.
Meirelles Kalil Pessoa de Barr E, Rodrigues CJ, de Barros TE, Bevilacqua RG . Presence of apolipoprotein E 4 allele in cerebral palsy. J Pediatr Orthop 2000;20:786–796.
Kuroda MM, Weck ME, Sarwark JF, Hamidullah A, Wainwright MS . Association of apolipoprotein E genotype and cerebral palsy in children. Pediatrics 2007;119:306–13.
Lo TY, Jones PA, Chambers IR, et al. Modulating effect of apolipoprotein E polymorphisms on secondary brain insult and outcome after childhood brain trauma. Childs Nerv Syst 2009;25:47–54.
Gaynor JW, Gerdes M, Zackai EH, et al. Apolipoprotein E genotype and neurodevelopmental sequelae of infant cardiac surgery. J Thorac Cardiovasc Surg 2003;126:1736–45.
Gaynor JW, Nord AS, Wernovsky G, et al. Apolipoprotein E genotype modifies the risk of behavior problems after infant cardiac surgery. Pediatrics 2009;124:241–50.
Schiefermeier M, Kollegger H, Madl C, et al. Apolipoprotein E polymorphism: survival and neurological outcome after cardiopulmonary resuscitation. Stroke 2000;31:2068–73.
Eisenberg DT, Kuzawa CW, Hayes MG . Worldwide allele frequencies of the human apolipoprotein E gene: climate, local adaptations, and evolutionary history. Am J Phys Anthropol 2010;143:100–11.
Shankaran S, Laptook AR, Ehrenkranz RA, et al.; National Institute of Child Health and Human Development Neonatal Research Network. Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N Engl J Med 2005;353:1574–84.
Shankaran S, Pappas A, McDonald SA, et al.; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Predictive value of an early amplitude integrated electroencephalogram and neurologic examination. Pediatrics 2011;128:e112–20.
Kamboh MI, Demirci FY, Wang X, et al.; Alzheimer’s Disease Neuroimaging Initiative. Genome-wide association study of Alzheimer’s disease. Transl Psychiatry 2012;2:e117.
Wu YW, Croen LA, Vanderwerf A, Gelfand AA, Torres AR . Candidate genes and risk for CP: a population-based study. Pediatr Res 2011;70:642–6.
O’Callaghan ME, Maclennan AH, Gibson CS, et al.; Australian Collaborative Cerebral Palsy Research Group. Fetal and maternal candidate single nucleotide polymorphism associations with cerebral palsy: a case-control study. Pediatrics 2012;129:e414–23.
Blackman JA, Worley G, Strittmatter WJ . Apolipoprotein E and brain injury: implications for children. Dev Med Child Neurol 2005;47:64–70.
Lien E, Andersen GL, Bao Y, et al. Apolipoprotein E polymorphisms and severity of cerebral palsy: a cross-sectional study in 255 children in Norway. Dev Med Child Neurol 2013;55:372–7.
Poirier J, Baccichet A, Dea D, Gauthier S . Cholesterol synthesis and lipoprotein reuptake during synaptic remodelling in hippocampus in adult rats. Neuroscience 1993;55:81–90.
Lee Y, Aono M, Laskowitz D, Warner DS, Pearlstein RD . Apolipoprotein E protects against oxidative stress in mixed neuronal-glial cell cultures by reducing glutamate toxicity. Neurochem Int 2004;44:107–18.
Laskowitz DT, Goel S, Bennett ER, Matthew WD . Apolipoprotein E suppresses glial cell secretion of TNF alpha. J Neuroimmunol 1997;76:70–4.
Laskowitz DT, Fillit H, Yeung N, Toku K, Vitek MP . Apolipoprotein E-derived peptides reduce CNS inflammation: implications for therapy of neurological disease. Acta Neurol Scand, Supplc 2006;185:15–20.
Blackman JA, Gurka MJ, Bao Y, Dragulev BP, Chen WM, Romness MJ . Apolipoprotein E and functional motor severity in cerebral palsy. J Pediatr Rehabil Med 2009;2:67–74.
Oriá RB, Patrick PD, Zhang H, et al. APOE4 protects the cognitive development in children with heavy diarrhea burdens in Northeast Brazil. Pediatr Res 2005;57:310–6.
Corbo RM, Scacchi R . Apolipoprotein E (APOE) allele distribution in the world. Is APOE*4 a ‘thrifty’ allele? Ann Hum Genet 1999;63(Pt 4):301–10.
Lewis SJ, Brunner EJ . Methodological problems in genetic association studies of longevity–the apolipoprotein E gene as an example. Int J Epidemiol 2004;33:962–70.
Mauch DH, Nägler K, Schumacher S, et al. CNS synaptogenesis promoted by glia-derived cholesterol. Science 2001;294:1354–7.
Mitter SS, Oriá RB, Kvalsund MP, et al. Apolipoprotein E4 influences growth and cognitive responses to micronutrient supplementation in shantytown children from northeast Brazil. Clinics (Sao Paulo) 2012;67:11–8.
Ioannidis JP, Ntzani EE, Trikalinos TA, Contopoulos-Ioannidis DG . Replication validity of genetic association studies. Nat Genet 2001;29:306–9.
Lohmueller KE, Pearce CL, Pike M, Lander ES, Hirschhorn JN . Meta-analysis of genetic association studies supports a contribution of common variants to susceptibility to common disease. Nat Genet 2003;33:177–82.
Hattersley AT, McCarthy MI . What makes a good genetic association study? Lancet 2005;366:1315–23.
Hixson JE, Vernier DT . Restriction isotyping of human apolipoprotein E by gene amplification and cleavage with HhaI. J Lipid Res 1990;31:545–8.
Author information
Authors and Affiliations
Consortia
Corresponding author
Supplementary information
Supplementary Appendix
(DOC 29 kb)
Rights and permissions
About this article
Cite this article
Cotten, C., Goldstein, R., McDonald, S. et al. Apolipoprotein E genotype and outcome in infants with hypoxic–ischemic encephalopathy. Pediatr Res 75, 424–430 (2014). https://doi.org/10.1038/pr.2013.235
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2013.235