Abstract
Background:
Intrathecal (IT) enzyme replacement therapy with recombinant human α-L-iduronidase (rhIDU) has been studied to treat glycosaminoglycan storage in the central nervous system of mucopolysaccharidosis (MPS) I dogs and is currently being studied in MPS I patients.
Methods:
We studied the immune response to IT rhIDU in MPS I subjects with spinal cord compression who had been previously treated with intravenous rhIDU. We measured the concentrations of specific antibodies and cytokines in serum and cerebrospinal fluid (CSF) collected before monthly IT rhIDU infusions and compared the serologic findings with clinical adverse event (AE) reports to establish temporal correlations with clinical symptoms.
Results:
Five MPS I subjects participating in IT rhIDU trials were studied. One subject with symptomatic spinal cord compression had evidence of an inflammatory response with CSF leukocytosis, elevated interleukin-5, and elevated immunoglobulin G. This subject also complained of lower back pain and buttock paresthesias temporally correlated with serologic abnormalities. Clinical symptoms were managed with oral medication, and serologic abnormalities were resolved, although this subject withdrew from the trial to have spinal decompressive surgery.
Conclusion:
IT rhIDU was generally well tolerated in the subjects studied, although one subject had moderate to severe clinical symptoms and serologic abnormalities consistent with an immune response.
Similar content being viewed by others
Main
Mucopolysaccharidosis I (MPS I) is a lysosomal storage disease caused by deficiency of the enzyme α-L-iduronidase (EC 3.2.1.76), leading to accumulation of glycosaminoglycans (GAG) throughout the body and resulting in multisystem dysfunction (1,2). Intravenous (i.v.) enzyme replacement therapy with recombinant human α-L-iduronidase (rhIDU) has been available for the treatment of MPS I patients since 2003 (3). When administered as a weekly infusion, i.v. rhIDU has been shown to reduce lysosomal GAG storage and improve many, though not all, of the clinical symptoms (3,4). An important shortcoming of i.v. rhIDU is the inability to effectively treat neurologic manifestations of central nervous system (CNS) GAG storage in MPS I patients (5). These include intellectual disability in the severe (Hurler) form of the disease, spinal cord compression owing to GAG storage in the cervical meninges of patients with attenuated disease (Hurler-Scheie and Scheie), and communicating hydrocephalus owing to obstructed cerebrospinal fluid (CSF) reabsorption in all forms of MPS I (6,7). Treatment of the latter often requires cervical laminectomy with removal of thickened meninges to decompress the spinal cord and ventriculoperitoneal shunt implantation to relieve CSF pressure (6,7,8,9).
Intrathecal (IT) enzyme replacement therapy has been successfully used for the treatment of lysosomal storage diseases in several animal models (10,11,12,13,14,15). When IT rhIDU is administered to MPS I dogs, the enzyme diffuses into the brain, spinal cord, and meninges and reduces GAG storage in these structures (15,16). Some of these dogs developed a CNS inflammatory response to IT rhIDU with mild to moderate aseptic meningitis (15,16). An immune response has also been observed in other animals when enzyme is administered directly into the CSF (12,13,17), and the CSF anti-rhIDU immunoglobulin (Ig) G titer in MPS I dogs correlates with diminished enzyme penetration into the brain and diminished efficacy in reducing GAG storage (17). The development of serum IgG antibodies against the recombinant protein is a common complication of i.v. enzyme replacement therapy, and MPS I patients receiving i.v. rhIDU often develop serum anti-rhIDU IgG antibodies (18). These patients generally do not suffer from clinically significant immunologic AEs (18), although the immune response to i.v. rhIDU has been shown to reduce therapeutic efficacy in MPS I dogs (19). Currently, IT rhIDU is being studied in clinical trials as a potential treatment for CNS disease in MPS I patients. The immune response to this therapy in humans has not been studied thus far.
In this study, we characterized the rhIDU-specific immune response in CSF and serum collected from MPS I subjects who had previously been treated with i.v. rhIDU and who were enrolled in clinical trials of IT rhIDU. We measured absolute concentrations of anti-rhIDU antibodies and TH1 and TH2 cytokines (20). We also reviewed case report forms for evidence of clinical AEs that were thought to be at least possibly related to IT rhIDU treatments and correlated these with laboratory findings. We found no serologic or clinical evidence of an anaphylactoid reaction in any subject. Most subjects had only mild to moderate clinical symptoms during the course of IT infusions and were able to complete the treatments. One subject with ongoing symptomatic spinal cord compression complained of intermittent lower back pain, buttock pain, and paresthesias following IT rhIDU infusions and developed a transiently elevated CSF white blood cell (WBC) count and anti-rhIDU IgG titer. The symptoms were managed with oral medications, and the CSF abnormalities were resolved within 3–4 mo though the subject ultimately withdrew from the trial for spinal decompressive surgery.
Results
We analyzed samples from a total of five subjects who gave signed, written informed consent and enrolled in the clinical trials described ( Table 1 ). One additional subject who enrolled in the pilot study died before any samples could be collected and so was not included in this analysis. A full discussion of the outcomes of the clinical trials is beyond the scope of this manuscript. Data from the completed pilot and extension studies will be detailed in a forthcoming report (P. Dickson et al., personal communication), although the cognition study is in progress.
At baseline, before the initiation of IT rhIDU infusions, all subjects had measurable serum levels of anti-rhIDU IgM and IgG ( Figure 1 ), an expected immune response with previous exposure to i.v. rhIDU therapy. Most subjects had higher levels of serum anti-rhIDU IgM than IgG. There was no detectable level of anti-rhIDU IgE in the serum of any subject studied. Serum anti-rhIDU IgD was also checked for consistency to rule out primary immunodeficiency (data not shown). None of the subjects had detectable levels of any anti-rhIDU antibody in the CSF at baseline (data not shown).
Baseline anti-rhIDU IgM, IgG, and IgE antibody concentrations in MPS I subject sera before starting IT rhIDU treatments. Right axis shows measured OD units per microliter; left axis shows converted antibody concentration in nanograms per milliliter. Subjects 001-01-03 (filled circles), 001-01-01 (open diamonds), 001-01-04 (open triangles), 001-02-01 (open circles), and 002-01-01 (open squares) are included in the study ( Table 1 ). There were no detectable levels of any anti-rhIDU antibody isotype in the CSF of any subject at baseline (data not shown). CSF, cerebrospinal fluid; Ig, immunoglobulin; IT rhIDU, intrathecal rhIDU enzyme replacement therapy; MPS I, mucopolysaccharidosis I; OD, optical density; rhIDU, recombinant human α-L-iduronidase.
After the initiation of monthly IT rhIDU infusions, none of the subjects developed a measurable anti-rhIDU IgM level in the CSF ( Figure 2b ), whereas all subjects had relatively low and constant anti-rhIDU IgM levels in the serum ( Figure 2a ). One subject, 001-01-04, had an elevated and fluctuating level of anti-rhIDU IgG in the serum, while all others had much lower relatively constant levels over time ( Figure 2c ). Only one subject, 001-01-03, developed a CSF anti-rhIDU IgG level ( Figure 2d ), peaking on day 90, before the fourth IT rhIDU infusion, and resolving during the following 2 mo. The serum and CSF anti-rhIDU IgG antibodies in this subject did not inhibit rhIDU uptake in vitro (data not shown). No subject had appreciable levels of anti-rhIDU IgE in the serum or the CSF ( Figure 2e , f ).
Anti-rhIDU antibody levels in MPS I subjects during the course of IT rhIDU treatments. (a) Serum anti-rhIDU IgM, (c) IgG, and (e) IgE; (b) CSF anti-rhIDU IgM, (d) IgG, and (f) IgE. Samples were drawn immediately before each monthly IT rhIDU infusion. Right axis shows measured OD units per microliter; left axis shows converted antibody concentration in nanograms per milliliter. Subjects 001-01-03 (filled circles), 001-01-01 (open diamonds), 001-01-04 (open triangles), 001-02-01 (open circles), and 002-01-01 (open squares) are included in the study ( Table 1 ). For subjects who received extended treatment courses—001-01-03 and 001-02-01—only data from the initial treatment period are shown for comparison. CSF, cerebrospinal fluid; Ig, immunoglobulin; IT rhIDU, intrathecal rhIDU enzyme replacement therapy; MPS I, mucopolysaccharidosis I; OD, optical density; rhIDU, recombinant human α-L-iduronidase.
At baseline, before the initiation of IT rhIDU infusions, there was no consistent pattern of abnormality across TH1 (cellular immune response) or TH2 (humoral immune response) cytokines in the serum or CSF ( Figure 3 ). All subjects had elevated (interleukin) IL-8 levels compared with the other cytokines studied, and this elevation was greater in the CSF than that in the serum in most subjects ( Figure 3a , b ). Individual subjects also displayed much lower but still detectable levels of tumor necrosis factor α, interferon γ, and IL-6 in the serum ( Figure 3a ), in addition to detectable levels of IL-6 in the CSF ( Figure 3b ).
Baseline absolute cytokine concentrations in the (a) serum and (b) CSF of MPS I subjects before starting IT rhIDU treatments. TH1 (cellular immune response) cytokines: IL-1β, IL-2, IL-8, TNF-α, and IFN-γ; TH2 (humoral immune response) cytokines: IL-4, IL-5, IL-6, IL-10, and GM-CSF (20). Subjects 001-01-03 (filled circles), 001-01-01 (open diamonds), 001-01-04 (open triangles), 001-02-01 (open circles), and 002-01-01 (open squares) are in the study ( Table 1 ). CSF, cerebrospinal fluid; GM-CSF, granulocyte macrophage colony-stimulating factor; IFN-γ; interferon γ; Ig, immunoglobulin; IL, interleukin; IT rhIDU, intrathecal rhIDU enzyme replacement therapy; MPS I, mucopolysaccharidosis I; rhIDU, recombinant human α-L-iduronidase; TNF-α, tumor necrosis factor α.
After the initiation of monthly IT rhIDU infusions, all subjects were found to have a persistently elevated IL-8 level in the CSF, which was relatively constant over a 4- to 5-mo period ( Figure 4b , d , f , h , j ). By contrast, most subjects had fluctuating IL-8 levels in the serum ( Figure 4a , c , e , g , i ). No subject had a pattern of cytokine elevations consistent with a TH1 or TH2 immune response in the serum or CSF. Subject 001-01-03 had a transiently elevated tumor necrosis factor α level in the serum ( Figure 4a ) and an elevated IL-5 level in the CSF, which peaked on day 90 just before the fourth IT rhIDU infusion ( Figure 4b ).
Cytokine levels in MPS I subjects during the course of IT rhIDU treatments. Absolute concentrations of TH1 (filled symbols: circles IL-1β; squares IL-2; diamonds IL-8; triangles TNF-α; inverted triangles IFN-γ) and TH2 cytokines (open symbols: circles IL-4; squares IL-5; diamonds IL-6; triangles IL-10; inverted triangles GM-CSF) measured in samples drawn immediately before each monthly IT rhIDU infusion. Horizontal rows correspond to individual subjects: 001-01-03 (a) serum and (b) CSF; 001-01-01 (c) serum and (d) CSF; 001-01-04 (e) serum and (f) CSF; 001-02-01 (g) serum and (h) CSF; 002-01-01 (i) serum and (j) CSF. For subjects who received extended treatment courses—(a,b) 001-01-03 and (g,h) 001-02-01—only data from the initial treatment period are shown for comparison. CSF, cerebrospinal fluid; GM-CSF, granulocyte macrophage colony-stimulating factor; IFN-γ; interferon γ; IL, interleukin; IT rhIDU, intrathecal rhIDU enzyme replacement therapy; MPS I, mucopolysaccharidosis I; OD, optical density; rhIDU, recombinant human α-L-iduronidase; TNF-α, tumor necrosis factor α.
At the time of enrollment, Subject 001-01-03 was 13 y old, with a history of hydrocephalus, for which a ventriculoperitoneal shunt was placed at the age of 6 y, and spinal cord compression, which was diagnosed on magnetic resonance imaging at 11 y. She received six off-label off-study IT rhIDU treatments every 1–2 mo before being approved for enrollment in the extension study, during which she received five IT rhIDU treatments at 90-d intervals ( Table 1 ). During the initial course of treatments, she developed an elevated CSF WBC count that peaked on day 90 before the fourth infusion and mirrored the elevations in CSF anti-rhIDU IgG ( Figure 5a ) and IL-5 ( Figure 5c ). The differential cell count in the CSF was predominantly lymphocytic (data not shown). B- and T-cell subsets of this lymphocyte count were not measured. This subject also had a markedly elevated CSF protein level at baseline ( Figure 5c ), attributed to spinal cord compression. She was treated with a 7-d course of oral prednisone after the fourth IT rhIDU infusion on day 90 ( Figure 5a , arrow) on the basis of her complaints of back and buttock pain and history of spinal cord compression. Subsequently, the CSF WBC count, anti-rhIDU IgG, IL-5, and protein levels decreased ( Figure 5a , c ), though the CSF protein level increased again after 1 mo ( Figure 5c ).
CSF findings in Subject 001-01-03. CSF WBC count (short dashed line: a,b), protein (long dashed line: c,d), and glucose (dotted line: c,d) were measured along with anti-rhIDU IgG antibody (filled circles with solid line: a,b), IL-8 (filled diamonds with solid line: c,d), and IL-5 (open squares with solid line: c,d) levels before each monthly IT rhIDU infusion. (a,c): Initial off-study treatment period; (b,d): extension study. Subject complained of mild buttock pain (arrowheads, a) and moderate to severe headache with facial flushing (arrowheads, b) was thought to be related to IT rhIDU. A 7-d course of oral prednisone was started following the fourth IT rhIDU infusion on day 90 (vertical arrow, a). Normal values for CSF indexes: WBC 0–7/µl; total protein 5–40 mg/dl; and glucose 40–80 mg/dl (38). CSF, cerebrospinal fluid; IgG, immunoglobulin G; IL, interleukin; IT rhIDU, intrathecal rhIDU enzyme replacement therapy; MPS I, mucopolysaccharidosis I; rhIDU, recombinant human α-L-iduronidase; WBC, white blood cell.
This subject was pretreated with oral prednisone before subsequent IT rhIDU infusions for pain and CSF pleocytosis. During the extension study, her CSF WBC count normalized and the CSF anti-rhIDU IgG level became undetectable ( Figure 5b ). By contrast, while the IL-5 level became undetectable in the CSF, the total protein and IL-8 levels increased further, as compared with the baseline, during the extension study ( Figure 5d ). The CSF glucose level remained within the normal range during the entire evaluation period ( Figure 5c , d ).
Subject 001-02-01, a 27-y-old female who completed the pilot study, also received eight additional IT rhIDU treatments during the extension study ( Table 1 ). Throughout the course of her participation, the CSF WBC count, protein, and glucose remained within normal limits, and all CSF anti-rhIDU antibody levels remained undetectable (data not shown). This subject had an elevated CSF IL-8 level during the pilot study ( Figure 4h ) that persisted without marked variation during the extension study (data not shown).
Subject 001-01-03 also experienced neurologic AEs that coincided with the CSF findings and were thought to be related to IT rhIDU infusions ( Table 2 ). She complained of buttock pain immediately following, or within 1-2 days of, IT rhIDU infusions on several occasions ( Figure 5a , arrowheads), including the fourth injection on day 90. The pain was bilateral, lasted 2–4 d, and was relieved by oral hydrocodone. She also had a history of frequent migraine headaches before enrollment and experienced one episode of severe headache and facial flushing following infusion number 7, for which she was hospitalized and observed according to study protocol ( Figure 5b , arrowhead). Finally, during the extension study, Subject 001-01-03 developed symptoms consistent with worsening spinal cord compression. She complained of leg pain, foot paresthesias, and hand weakness and then developed urinary urgency and incontinence. She was evaluated by her neurosurgeon, underwent spine imaging, and withdrew from the trial for spinal decompressive surgery that was performed 2 mo following the last IT rhIDU infusion shown in Figure 5b and 5d . No serologic or AE data were collected after withdrawal from the trial; therefore, we cannot evaluate the effect of decompressive surgery on the CSF abnormalities. The subject’s symptoms were not attributed to IT rhIDU, and the compression symptoms were resolved following surgery.
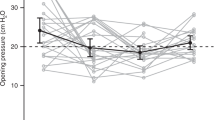
Among the remaining subjects, there were a total of six serious AEs reported: pneumonia (001-01-01, 001-02-01); hypoxia with respiratory distress (001-02-01) and corneal transplantation (001-02-01); and buttock cramping, spinal cord compression, and prostate cancer (002-01-01). One instance of pneumonia was thought to be possibly related to IT rhIDU infusion (001-01-01) although none of the other serious AEs described in any subject were thought to be related to the infusions. Most subjects complained of mild intermittent or isolated headaches following the first one or two IT rhIDU infusions; these were generally not recurrent and not temporally associated with any CSF or serum abnormality. Subject 001-01-04, a 24-y-old female with cervical spinal stenosis, hydrocephalus, and lumboperitoneal shunt—who had a history of chronic headaches, neck pain, and upper back pain—complained of slightly worsened pain symptoms following the first three IT rhIDU infusions. She was also found to have a transiently elevated CSF opening pressure of 26 cm H2O before the third injection. Her chronic pain symptoms were managed with oral steroids and analgesics during the trial.
Discussion
We studied subjects enrolled in clinical trials to assess safety of IT rhIDU and functional improvement in MPS I patients with spinal cord compression or cognitive impairment. All subjects had previous exposure to i.v. rhIDU for at least 6 mo, and in most cases, for several years, before study entry. All subjects experienced some form of neurological complaint or symptom, most commonly mild intermittent or isolated headaches.
Neurologic adverse reactions have been previously reported in patients receiving IT injections of therapeutic proteins. Two patients treated with IT rituximab for CNS B-cell lymphoma complained of painful paresthesias involving the buttocks, legs, and feet immediately following lumbar puncture and injection (21). These symptoms were also reported in a patient who was treated after decreasing the protein concentration of the IT injection, although after adding IT dexamethasone to the protocol, no additional patients complained of the same pain (21).
Similar neurologic symptoms can also be attributed to drug-induced aseptic meningitis, an uncommon though well-known CNS inflammatory process characterized by CSF pleocytosis with lymphocytosis, normal to low glucose levels, and elevated protein levels in the absence of infection (22,23). Possible mechanisms include a hypersensitivity reaction limited to the meninges, deposition of circulating immune complexes within the meninges, or direct chemical irritation of the meninges caused by IT drug delivery (23).
In our study, Subject 001-01-03 had laboratory evidence of aseptic meningitis that developed during the course of IT rhIDU infusions. However, the concurrent development of an elevated anti-rhIDU IgG antibody level in the CSF suggests a specific immune response. Dogs receiving IT rhIDU developed a CSF pleocytosis and anti-rhIDU IgG antibodies (15), and histological evaluation of the meninges showed a plasma cell infiltrate in these dogs. While it is possible that aseptic meningitis could cause increased permeability of the blood–brain barrier, allowing leakage of lymphocytes into the CSF, the absence of correspondence between serum and CSF IL-5 and IL-8 levels in Subject 001-01-03 ( Figure 4a , 4b ) makes this mechanism unlikely as the sole explanation for the CSF anti-rhIDU IgG findings.
Patients with all forms of MPS I have unmeasurable endogenous α-L-iduronidase activity though those with attenuated disease may synthesize trace amounts of endogenous enzyme depending on the underlying genetic mutation (1,24). This cross-reactive immunologic material is recognized as self-protein by the host immune system, and its presence is thought to mitigate the development of serum antibodies to i.v. recombinant human enzyme in cross-reactive immunologic material–positive subjects as compared with cross-reactive immunologic material–negative subjects (18). It is not clear how this concept extends to explain the development of anti-rhIDU IgG antibodies in the relatively immune-privileged CNS. All the subjects studied had an attenuated MPS I phenotype consistent with probable cross-reactive immunologic material–positive status and had varying concentrations of anti-rhIDU IgG in their sera, although only one had an elevated level in the CSF. The subject with CSF anti-rhIDU IgG antibodies was found to have antibodies that did not inhibit rhIDU uptake or activity in vitro.
Froin’s syndrome—elevated protein, xanthochromia, and hypercoagulability of the CSF—is a well-described phenomenon reported in patients with spinal canal obstruction caused by tumors, epidural abscess, or spinal meningitis (25,26) and accounts for some of the CSF findings in Subject 001-01-03. However, this does not explain the observation that this subject’s clinical symptoms and CSF protein level progressed even while all laboratory evidence of a specific CSF immune response and all serious AEs related to IT rhIDU infusions resolved ( Figure 5b , 5d ).
IL-8, a chemokine also known as CXCL8, is produced by a variety of cells, including monocytes, macrophages, fibroblasts, and endothelial cells, and functions as a chemoattractant for neutrophils and naive T cells, stimulating neutrophil activation and degranulation (20). IL-5 is produced by TH2 CD4 T cells and stimulates bone marrow production of eosinophils (20). The significance of the comparative CSF elevations of IL-8 and IL-5 in Subject 001-01-03 is unclear owing to a lack of correspondence in CSF cell count findings and the lack of published normative data for comparison. Previously published studies of cytokine levels in the CSF focus on patients with infectious (26,27,28,29,30), autoimmune (31,32), or other neurologic disease (33,34,35). The variety of acute or chronic conditions studied and the inconsistency of methods used to quantify cytokine levels make comparison with the results from our patients difficult. Immune tolerance to rhIDU, owing to the combination of immunosuppression by monthly steroid prophylaxis and antigen exposure, could theoretically explain the decrease in specific CSF IgG and WBC count in Subject 001-01-03, similar to the regimen shown to produce serum immune tolerance in MPS I dogs treated with i.v. rhIDU (36).
The small number of subjects we studied may bias our interpretation by limiting the variety of neurologic AEs we were able to observe. The absence of a control group for comparison, which is inherent while enrolling a sufficient number of subjects with rare diseases in clinical trials, is also a limitation of our study. However, the potential benefits of this novel therapy for MPS I patients are significant—treating CNS disease including intellectual disability, spinal cord compression symptoms, and hydrocephalus—while the AEs that we attribute to the immune response to IT rhIDU were tolerable and managed fairly readily with steroids and pain medication.
In summary, we studied laboratory and clinical data for five MPS I subjects with spinal cord compression and a history of previous i.v. rhIDU treatment enrolled in trials of IT rhIDU to assess for evidence of an immune response to the therapy. To our knowledge, this study represents the first systematic characterization of the immune response to IT rhIDU in MPS I patients and the first measurement of absolute antibody and cytokine concentrations in the sera and CSFs of MPS I patients. Four subjects had intermittent mild neurologic complaints, including headache, back pain, and neck pain, which were managed with oral analgesics or steroids in one case. They had no laboratory evidence of an immune or inflammatory response to the therapy. One subject with symptomatic progressive spinal cord compression complained of back and buttock pain and paresthesias following IT rhIDU infusions and developed a transiently elevated CSF anti-rhIDU IgG level. She ultimately withdrew from the trial for spinal decompressive surgery. The remaining subjects completed their respective treatment courses without clinical or laboratory evidence of an enzyme-specific immune response to IT rhIDU therapy.
Methods
This study involved deidentified patient samples and case report forms. The study was reviewed and approved by the John Wolf Human Subjects Committee of the Los Angeles Biomedical Research Institute at Harbor-University of California Los Angeles Medical Center, and a waiver of informed consent was granted.
rhIDU (Aldurazyme, BioMarin Pharmaceutical, Novato, CA) was approved for i.v. use in humans by the US Food and Drug Administration and was administered via the IT route under an Investigational New Drug authorization from the Food and Drug Administration and the European Union Drug Regulating Authorities. Patient samples and case report forms from three multicenter, multinational safety studies were included.
In a pilot study (NCT 00215527), MPS I subjects with spinal cord compression who were at least 8 y old and who had received i.v. rhIDU treatments for at least 6 mo were treated monthly with 1.74 mg IT rhIDU for a total of four doses (“pilot study”). This dose was chosen for human trials based on the lowest IT dose required to achieve increased enzyme levels in the brain and meninges and reduction of brain GAG in MPS I dogs (15). In an extension study (NCT 00786968), MPS I subjects who completed the pilot study with good response to IT rhIDU, defined by improvement in any outcome measure and no safety concerns, received up to 12 mo of additional therapy at 30- to 90-d intervals (“extension study”). In a “cognition study” (NCT 00852358), MPS I subjects with cognitive impairment or decline who were at least 6 y old and who had received i.v. rhIDU treatments for at least 6 mo were enrolled in a 1-y randomized controlled trial followed by 1-y open-label phase of 1.74 mg IT rhIDU given at 30- to 90-d intervals (“cognition study”).
One subject (001-01-03, Table 1 ) received off-study, off-label IT rhIDU treatments before enrollment in the extension study. Samples and clinical information from the off-study period were included.
In each study, rhIDU (0.58 mg/ml) was diluted with 6−8 ml of Elliotts B solution (Ben Venue Laboratories, Bedford, OH), a buffered IT injection diluent with pH, electrolytes, glucose, and osmolarity almost similar to human CSF. The diluted enzyme was administered via lumbar puncture and infused slowly over 2−3 min. Subjects were individually pretreated with acetaminophen and an antihistamine before infusions. Each subject was closely monitored during infusions for any adverse clinical reactions.
Safety was assessed throughout each subject’s study participation with periodic clinical and laboratory evaluations. A history and physical examination was performed at each visit during the studies, and any clinically significant worsening from baseline medical status was documented as an AE. Laboratory assessments included CSF opening pressure, CSF and serum chemistry and cell counts, GAG quantitation, cytokine quantitation, and enzyme-linked immunosorbent assay for α-L-iduronidase-specific antibodies.
CSF and Serum Collection
Samples were collected at baseline and immediately before each i.v. enzyme infusion. Approximately 6−10 ml of CSF was withdrawn at each lumbar puncture and 2.5−5 ml of whole blood was collected in a serum separator tube. Samples were aliquoted and stored at −80 °C and later thawed for subsequent antibody and cytokine assays.
CSF and Serum Enzyme-Linked Immunosorbent Assay for α-L-Iduronidase-Specific Antibodies
Anti-rhIDU antibodies were measured by an enzyme-linked immunosorbent assay method. In brief, CSF and serum samples collected from each subject at each time point were first diluted in a ratio of 1:100; then subsequent 1:3 serial dilutions were incubated on 96-well assay plates (Immulon 1B U-bottom microtiter plates, Dynex Technologies, Chantilly, VA) containing wells with adsorbed rhIDU (BioMarin Pharmaceutical). Specific binding of CSF and serum anti-rhIDU antibodies to the coated wells was detected using alkaline phosphate–conjugated goat anti-human IgG (Southern Biotechnology Associates, Birmingham, AL), IgM, or IgE (Bethyl Laboratories, Montgomery, TX) secondary antibodies. Absorbance at 405 nm was measured as optical density values using a BioTek Synergy 2 Microplate Reader (BioTek Instruments, Winooski, VT), converted to optical density units per microliter based on the dilution and then subsequently converted to protein concentration in nanograms per milliliter by comparison with a human IgG standard curve, using linear regression to calculate the conversion factor.
Enzyme Uptake Inhibition Assay
We measured the in vitro inhibition of exogenous rhIDU uptake by anti-rhIDU antibodies in the serum and CSF of study subjects using a previously described method (19). In brief, rhIDU (BioMarin Pharmaceutical) was diluted to a concentration of 18 U/ml in minimal essential medium, without fetal bovine serum, plus 1% L-glutamine (Hyclone Classical Liquid Media MEM EBSS, Thermo Fisher Scientific, Waltham, MA) and then incubated for 1 h at room temperature in the absence or presence of either serum or CSF of the subject added at 1:50 dilution. Skin fibroblasts from an MPS I Hurler individual (GM 1391; National Institute of General Medical Sciences, Human Genetic Cell Repository, Coriell Institute for Medical Research, Camden, NJ) were passed to a confluence of 85–95% in six-well cell culture cluster plates, and the diluted serum or CSF plus rhIDU mixture or rhIDU alone was added in 2-ml aliquots to triplicate wells containing these confluent cells. Cells were incubated at 37 °C and 5% CO2 for 1 h, rinsed, harvested by trypsinization, and pelleted by centrifugation. The pellet was washed and resuspended, disrupted by sonication, and centrifuged. Enzyme activity in the supernatant was measured in triplicate assays by detecting cleavage of 4-methylumbelliferyl derivatives (19,37) from 4-methylumbelliferyl α-L-iduronide (Calbiochem, San Diego, CA) by rhIDU using a spectrofluorophotometer at 365-nm excitation and 440-nm emission (Shimadzu RF-1501, Shimadzu, Tokyo, Japan). One unit of activity was equivalent to 1 nmol converted substrate per hour.
CSF and Serum Cytokine Assay
Cytokine levels in CSF and serum samples collected from each subject at each time point were quantified using a multiplex bead-based immunoassay (Invitrogen Human Cytokine 10-Plex Panel, Life Technologies, Grand Island, NY). Briefly, the wells of a 96-well filter plate (1.2-μ Durapore membrane 96-well plate, EMD Millipore, Billerica, MA) were prewet with working wash solution provided by the manufacturer (Wash Solution Concentrate, Life Technologies), and polystyrene beads individually coated with antibodies specific to human cytokines IL-1β, IL-2, IL-4, IL-5, IL-6, IL-8, IL-10, tumor necrosis factor α, interferon γ, or granulocyte macrophage colony-stimulating factor, were added (Human Cytokine 10-Plex Antibody Bead Concentrate, Life Technologies). Incubation buffer and assay diluent provided by the manufacturer (Life Technologies) along with 50 µl of either CSF or serum samples were added, and the plate was incubated on a shaker for 2 h at room temperature. Serial dilutions of a standard solution of the above 10 cytokines provided by the manufacturer were also plated in duplicate (Human 16-Plex Standard, Life Technologies). After the incubation, 100 µl of biotinylated antibodies specific to each assayed cytokine (Human Cytokine 10-Plex Biotinylated Antibody Concentrate, Life Technologies) was added to each well, and the plate was incubated on a shaker for 1 h at room temperature. Streptavidin conjugated with R-phycoerythrin (Streptavidin–RPE Concentrate, Life Technologies) was added to each well, followed by a 30-min incubation on a shaker at room temperature. After aspiration and washing, the beads were resuspended in working wash solution, and the fluorescent intensity of streptavidin–RPE-tagged cytokine-specific beads was read with a Luminex-200 dual laser detection system (Luminex, Austin, TX). Standard curves were generated by the Luminex xMAP analysis software package (Luminex) for each cytokine and were used to convert measured fluorescent intensity to absolute concentration in picograms per milliliter. All samples were assayed in duplicate.
AE Review
Case report forms labeled with subject number and initials were used to determine total AEs based on history, physical examination, and neurologic examination. An AE was defined as any undesirable physical, psychological, or behavioral effect experienced by a subject during his or her participation in the study including subjective or objective symptoms reported by the subject and/or observed by the medical staff; clinically significant laboratory anomalies; and exacerbation of preexisting disease-related symptoms or laboratory abnormalities. These were characterized by type, severity, onset, and duration and rated by the study investigator as definitely, probably, or possibly related to the IT rhIDU infusion. The subset of neurologic AE was identified for each subject, and the recorded dates were compared with the dates of sample collections and IT rhIDU infusions.
Statement of Financial Support
This study was supported by grants from the US Food and Drug Administration (FD003450); the Lysosomal Disease Network (NS065768); the University of California, Los Angeles, Clinical and Translational Science Institute (National Center for Advancing Translational Sciences, grant UL1TR000124); National Institutes of Health’s National Center for Research Resources (Clinical and Translational Science Award, UL1RR024131, to Paul Harmatz); the Ryan Foundation for MPS Children; BioMarin Pharmaceutical (Novato, CA); and Genzyme (Cambridge, MA). This publication was also made possible in part by the National Institute of General Medical Sciences (NIGMS), National Institutes of Health (NIH; grant 5T32GM008243-27, to Moin Vera). The Lysosomal Disease Network is a part of the NIH Rare Diseases Clinical Research Network (RDCRN), supported through collaboration between the NIH Office of Rare Diseases Research (ORDR) at the National Center for Advancing Translational Science (NCATS), the National Institute of Neurological Disorders and Stroke (NINDS), and National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or NIGMS.
Disclosures
The Los Angeles Biomedical Research Institute at Harbor-UCLA and the Department of Pediatrics at Harbor-UCLA have a financial interest in rhIDU (formulated as laronidase). Paul Harmatz has provided consulting services to BioMarin Pharmaceutical and has received research grants, participated in advisory boards, and received speakers honoraria and travel support from BioMarin.
References
Neufeld EF, Meunzer J . The Mucopolysaccharidoses. In: Scriver CR, Beaudet AL, Sly WS, Valle D, eds. The Metabolic and Molecular Bases of Inherited Disease. New York: McGraw-Hill, 2001:3421–52.
Wraith JE . Mucopolysaccharidoses and oligosaccharidoses. In: Saudubray J-M, van den Berghe G, Walter JH, eds. Inborn Metabolic Diseases: Diagnosis and Treatment, 5th ed. Berlin: Springer-Verlag, 2012:579–90.
Kakkis ED, Muenzer J, Tiller GE, et al. Enzyme-replacement therapy in mucopolysaccharidosis I. N Engl J Med 2001;344:182–8.
Wraith JE, Clarke LA, Beck M, et al. Enzyme replacement therapy for mucopolysaccharidosis I: a randomized, double-blinded, placebo-controlled, multinational study of recombinant human alpha-L-iduronidase (laronidase). J Pediatr 2004;144:581–8.
Enns GM, Huhn SL . Central nervous system therapy for lysosomal storage disorders. Neurosurg Focus 2008;24:E12.
Kachur E, Del Maestro R . Mucopolysaccharidoses and spinal cord compression: case report and review of the literature with implications of bone marrow transplantation. Neurosurgery 2000;47:223–8; discussion 228–9.
Dickson PI, Chen AH . Intrathecal enzyme replacement therapy for mucopolysaccharidosis I: translating success in animal models to patients. Curr Pharm Biotechnol 2011;12:946–55.
Kennedy P, Swash M, Dean MF . Cervical cord compression in mucopolysaccharidosis. Dev Med Child Neurol 1973;15:194–9.
Kaufman HH, Rosenberg HS, Scott CI, Lee YY, Pruessner JL, Butler IJ . Cervical myelopathy due to dural compression in mucopolysaccharidosis. Surg Neurol 1982;17:404–10.
Lee WC, Tsoi YK, Troendle FJ, et al. Single-dose intracerebroventricular administration of galactocerebrosidase improves survival in a mouse model of globoid cell leukodystrophy. FASEB J 2007;21:2520–7.
Dodge JC, Clarke J, Treleaven CM, et al. Intracerebroventricular infusion of acid sphingomyelinase corrects CNS manifestations in a mouse model of Niemann-Pick A disease. Exp Neurol 2009;215:349–57.
Chang M, Cooper JD, Sleat DE, et al. Intraventricular enzyme replacement improves disease phenotypes in a mouse model of late infantile neuronal ceroid lipofuscinosis. Mol Ther 2008;16:649–56.
Hemsley KM, King B, Hopwood JJ . Injection of recombinant human sulfamidase into the CSF via the cerebellomedullary cistern in MPS IIIA mice. Mol Genet Metab 2007;90:313–28.
Auclair D, Finnie J, Walkley SU, et al. Intrathecal recombinant human 4-sulfatase reduces accumulation of glycosaminoglycans in dura of mucopolysaccharidosis VI cats. Pediatr Res 2012;71:39–45.
Kakkis E, McEntee M, Vogler C, et al. Intrathecal enzyme replacement therapy reduces lysosomal storage in the brain and meninges of the canine model of MPS I. Mol Genet Metab 2004;83:163–74.
Dickson P, McEntee M, Vogler C, et al. Intrathecal enzyme replacement therapy: successful treatment of brain disease via the cerebrospinal fluid. Mol Genet Metab 2007;91:61–8.
Dickson PI, Ellinwood NM, Brown JR, et al. Specific antibody titer alters the effectiveness of intrathecal enzyme replacement therapy in canine mucopolysaccharidosis I. Mol Genet Metab 2012;106:68–72.
Wang J, Lozier J, Johnson G, et al. Neutralizing antibodies to therapeutic enzymes: considerations for testing, prevention and treatment. Nat Biotechnol 2008;26:901–8.
Dickson P, Peinovich M, McEntee M, et al. Immune tolerance improves the efficacy of enzyme replacement therapy in canine mucopolysaccharidosis I. J Clin Invest 2008;118:2868–76.
Janeway CA, Travers P, Walport M, Shlomchik MJ, eds. Immunobiology: The Immune System in Health and Disease, 6th ed. New York: Garland, 2005:347–51.
Bromberg JE, Doorduijn JK, Baars JW, van Imhoff GW, Enting R, van den Bent MJ . Acute painful lumbosacral paresthesia after intrathecal rituximab. J Neurol 2012;259:559–61.
Moris G, Garcia-Monco JC . The challenge of drug-induced aseptic meningitis. Arch Intern Med 1999;159:1185–94.
Kepa L, Oczko-Grzesik B, Stolarz W, Sobala-Szczygiel B . Drug-induced aseptic meningitis in suspected central nervous system infections. J Clin Neurosci 2005;12:562–4.
Schuchman EH, Desnick RJ . Mucopolysaccharidosis type I subtypes. Presence of immunologically cross-reactive material and in vitro enhancement of the residual alpha-L-iduronidase activities. J Clin Invest 1988;81:98–105.
Greenfield JG . Original Papers: on Froin’s syndrome, and its relation to allied conditions in the cerebrospinal fluid. J Neurol Psychopathol 1921;2:105–41.
Mirza S, Adams WM, Corkhill RA . Froin’s syndrome revisited, 100 years on. Pseudo-Froin’s syndrome on MRI. Clin Radiol 2008;63:600–4.
Asano T, Ichiki K, Koizumi S, et al. Enhanced expression of cytokines/chemokines in cerebrospinal fluids in mumps meningitis in children. Pediatr Int 2011;53:143–6.
John CC, Panoskaltsis-Mortari A, Opoka RO, et al. Cerebrospinal fluid cytokine levels and cognitive impairment in cerebral malaria. Am J Trop Med Hyg 2008;78:198–205.
Ichiyama T, Ito Y, Kubota M, Yamazaki T, Nakamura K, Furukawa S . Serum and cerebrospinal fluid levels of cytokines in acute encephalopathy associated with human herpesvirus-6 infection. Brain Dev 2009;31:731–8.
Pinto Junior VL, Rebelo MC, Gomes RN, Assis EF, Castro-Faria-Neto HC, Bóia MN . IL-6 and IL-8 in cerebrospinal fluid from patients with aseptic meningitis and bacterial meningitis: their potential role as a marker for differential diagnosis. Braz J Infect Dis 2011;15:156–8.
Maimone D, Gregory S, Arnason BG, Reder AT . Cytokine levels in the cerebrospinal fluid and serum of patients with multiple sclerosis. J Neuroimmunol 1991;32:67–74.
Trysberg E, Carlsten H, Tarkowski A . Intrathecal cytokines in systemic lupus erythematosus with central nervous system involvement. Lupus 2000;9:498–503.
Mogi M, Harada M, Narabayashi H, Inagaki H, Minami M, Nagatsu T . Interleukin (IL)-1 beta, IL-2, IL-4, IL-6 and transforming growth factor-alpha levels are elevated in ventricular cerebrospinal fluid in juvenile parkinsonism and Parkinson’s disease. Neurosci Lett 1996;211:13–6.
Mittleman BB, Castellanos FX, Jacobsen LK, Rapoport JL, Swedo SE, Shearer GM . Cerebrospinal fluid cytokines in pediatric neuropsychiatric disease. J Immunol 1997;159:2994–9.
Ludwig J, Binder A, Steinmann J, Wasner G, Baron R . Cytokine expression in serum and cerebrospinal fluid in non-inflammatory polyneuropathies. J Neurol Neurosurg Psychiatr 2008;79:1268–73.
Kakkis E, Lester T, Yang R, et al. Successful induction of immune tolerance to enzyme replacement therapy in canine mucopolysaccharidosis I. Proc Natl Acad Sci USA 2004;101:829–34.
Kakkis ED, McEntee MF, Schmidtchen A, et al. Long-term and high-dose trials of enzyme replacement therapy in the canine model of mucopolysaccharidosis I. Biochem Mol Med 1996;58:156–67.
Tschudy MM, Arcara KM, eds. Johns Hopkins: The Harriet Lane Handbook, 19th ed. Philadelphia: Mosby, 2012.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vera, M., Le, S., Kan, Sh. et al. Immune response to intrathecal enzyme replacement therapy in mucopolysaccharidosis I patients. Pediatr Res 74, 712–720 (2013). https://doi.org/10.1038/pr.2013.158
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2013.158
This article is cited by
-
New treatments for the mucopolysaccharidoses: from pathophysiology to therapy
Italian Journal of Pediatrics (2018)
-
Clinical Improvement of Alpha-mannosidosis Cat Following a Single Cisterna Magna Infusion of AAV1
Molecular Therapy (2016)