Abstract
We aimed to identify the effect of suction pressure and catheter size on change in lung volume during open and closed endotracheal suction. Anesthetized piglets (n = 12) were intubated with a 4.0-mm endotracheal tube. Lung injury was induced with saline lavage. Three suction methods (open, closed in-line, and closed with a side-port adaptor) were performed in random order using 6, 7, and 8 French gauge (FG) catheters, at vacuum pressures of 80, 140, and 200 mm Hg. Lung volume change was measured with respiratory inductive plethysmography. Overall, open suction resulted in greater lung volume loss during and at 60-s postsuction than either closed method (p < 0.001). When open and closed methods were analyzed separately, volume change was independent of catheter size and suction pressure with open suction. With closed suction, volume loss increased with larger catheter sizes and higher suction pressures (p < 0.001). With an 8-FG catheter and suction pressure of 140 or 200 mm Hg, volume loss was equivalent with open and closed suction. Lung volume changes are influenced by catheter size and suction pressure, as well as suction method. With commonly used suction pressures and catheter sizes, closed suction has no advantage in preventing loss of volume in this animal model.
Similar content being viewed by others

Main
Endotracheal tube (ETT) suction is performed periodically in patients receiving mechanical ventilation, to maintain a patent airway and facilitate ventilation. Although necessary, it is associated with adverse sequelae including atelectasis, hypoxia, and cardiovascular instability (1–4), attributed in part to loss of lung volume. Volume loss can arise from breaking the ventilator circuit for “open” suction and aspiration of gas after application of negative pressure. Closed suction techniques, performed without disconnecting the ventilator circuit, have been widely adopted to reduce the adverse effects of suction (5).
Two closed suction techniques are available: in-line systems, in which a suction catheter, enclosed in a plastic sheath, is incorporated into the ventilator circuit; and side-port adaptors, Y-shaped connectors placed between the ETT and the ventilator circuit, through which a suction catheter is passed. Few studies have compared the two methods, and there is little evidence to support the use of one over the other (6–8). Both techniques have been shown to result in greater physiologic stability in neonates (9,10), and less loss of lung volume in adults (7,11) and children (12) than open suction, although large volume losses have been recorded with both closed and open methods (7,12,13). In the only neonatal study to date comparing lung volume changes, there was no difference in volume loss between open and closed suction during either conventional or high-frequency oscillatory ventilation (HFOV), and wide variation in losses with both methods (14).
The contribution to volume loss of factors other than suction method remains to be elucidated. At least in vitro, suction catheter size and suction pressure have been implicated in determining tracheal pressure during suction (15–17), the presumed precursor to volume loss. Whether tracheal pressure changes result in clinically observable effects is unclear (4,18–20) and there is no consensus on appropriate catheter sizes or suction pressures for clinical use in children or neonates (21–27). No studies have investigated the impact of these factors on lung volume changes.
The aim of this study was to investigate the effect of suction method (open, closed in-line, and closed with a side-port adaptor), catheter size, and suction pressure on lung volume changes during endotracheal suction. Comparisons were made during both conventional, time-cycled pressure-limited ventilation (TCPLV) and HFOV.
MATERIALS AND METHODS
The study procedures were approved by the Murdoch Childrens Research Institute Animal Ethics Committee. It was not feasible to conduct the study in human infants, as the protocol required multiple episodes of suction in a short timeframe, together with repeated alveolar derecruitment and rerecruitment, and thus an animal model was used. Two-wk-old piglets (n = 12) were anesthetized with isoflurane and intubated with a 4.0-mm cuffed ETT; the cuff was then inflated until no leak was detected. Anesthesia was maintained with propofol 10 mg/kg/h and morphine 0.6 mg/kg/h, and muscle relaxation achieved with pancuronium 0.15 mg/kg/h. TCPLV (Bear Cub; Viasys Healthcare, Yorba Linda, CA) was established with initial settings rate 30, inspiratory time 0.5 s, positive end-expiratory pressure (PEEP) 5 cm H2O, and peak inspiratory pressure (PIP) to maintain tidal volume at 10 mL/kg. Inspired oxygen fraction was maintained at 1.0 throughout the experiment, in accordance with recommendations for endotracheal suction in infants and children (22). A pneumotachograph (Florian respiratory monitor, Acutronic Medical Systems, Zug, Switzerland) was placed proximal to the ETT. Lung injury was induced with repeat saline lavage until the alveolar-arterial oxygen difference was ≥400 mm Hg for 30 min.
Measurements.
End-expiratory lung volume change (ΔVL) was estimated with a low-pass filtered, DC-coupled respiratory inductive plethysmograph (RIP) (Respitrace 200; Noninvasive Monitoring Systems Inc., North Bay Village, FL), sampling at 200 Hz using the method we have described previously (28,29). Once thermally stable (30), the voltage signal was calibrated during 15 ventilator inflations on TCPLV to the tidal volume measured by the pneumotachograph, and a calibrated volume signal obtained from the sum of the abdominal and chest RIP voltages (31).
Experimental protocol.
Before commencing the experimental series, the pressure–volume (PV) relationship of the lung was mapped with RIP by increasing PIP and PEEP in increments of 5 cm H2O until the upper inflection point was passed and no further end-expiratory recruitment was achieved (total lung capacity), then decreasing at the same rate until the PEEP was 0 cm H2O, mapping the deflation limb and identifying the point of maximal curvature (closing pressure) (29,32). Each limb of the PV relationship was mapped over a 3-min period. Lung volume data were displayed and recorded continuously throughout the process using a custom-built data acquisition program designed with LabVIEW 6.0 (National Instruments, Austin, TX). The recording provided a template that was displayed on a computer screen for the duration of the experiment, with real-time PV recordings superimposed, thus, enabling guidance of ventilation changes. The lung was then rerecruited through total lung capacity and ventilation established on the deflation limb, with PEEP 2 cm H2O above the identified closing pressure, and PIP set to maintain the premapping PIP-PEEP difference (33,34).
Suction episodes were then performed using all permutations of three methods (open, in-line, and side-port adaptor) and three catheter sizes (6, 7, and 8 French gauge [FG]), in random order. Randomisation was performed using a dedicated randomisation program (Graphpad software, San Diego, CA). The full range of procedures could not be performed in all animals; thus, in six animals the above permutations were performed twice, at vacuum pressures of 80 and 200 mm Hg (11 and 27 kPa), applied in random order, and in the remaining six animals all episodes were performed at a vacuum pressure of 140 mm Hg (19 kPa). The in-line system was the Ballard Trachcare (Kimberly-Clark, Roswell, GA) and the side-port adaptor a Neo-LINK universal adaptor (Viasys MedSystems, Wheeling, IL), which contains a self-sealing valve that permits catheter entry without opening the circuit to atmosphere. The same disposable catheters (Mallinkrodt, Rowville, Victoria, Australia) were used for open and side-port adaptor suction. Both types of catheter are 30 cm in length and have one end and two side holes of identical size. The 6-, 7-, and 8-FG catheters have external diameters of 2, 2.3, and 2.7 mm, respectively, and thus occlude 25%, 34%, and 44% of the 4.0-mm ETT luminal cross-sectional area. As reported previously (15), gas flow through each of the catheters increases in a nonlinear fashion with increasing suction pressure, consistent with turbulent flow.
In all cases, the suction catheter was passed to the tip of the ETT without suction, and suction subsequently applied for 6 s, the typical duration of suction in our institutions, while withdrawing the catheter. Between episodes, lung rerecruitment was performed as required, as described earlier, to maintain lung volume at the same point on the PV relationship, as determined by the prerecorded template (33,34). Suction episodes were performed at ∼5-min intervals.
HFOV was then commenced (3100A high-frequency oscillator; Sensormedics, Yorba Linda, CA). The PV relationship was mapped as before, by adjusting the mean airway pressure (Paw) in steps of 3 cm H2O, and ventilation was subsequently established on the deflation limb, 2 cm H2O above closing pressure (33). Between suction episodes, Paw was adjusted as required to rerecruit through total lung capacity and maintain ventilation at the same point. Frequency was fixed at 10 Hz, and amplitude set to maintain Pco2 at 35–55 cm H2O. The suction episodes were repeated as described earlier. In total, six animals received 36 episodes of suction, and six received 18 episodes. The entire experiment lasted for ∼4 h in each animal.
Data collection and analysis.
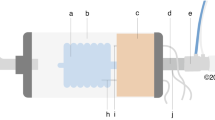
Lung volume data were recorded continuously from 15 s before each suction procedure until 90 s after its completion. Each RIP recording was examined and ΔVL determined at critical time points using a data processing program designed with LabVIEW 6.0 (Fig. 1). The main points of comparison were the minimum volume and the residual volume loss still evident at 60 s after completion of the procedure (ΔVL60). Univariate ANOVA was used to examine the overall effect of each of the three suction variables in turn. Combined effects, including interactions, were then examined using multiway ANOVA. Logistic regression was used to predict recovery of lung volume to ≥ 90% of baseline. All statistical analyses were performed using Stata 8.0 (Stata Corporation, College Station, TX).
Calibrated RIP tracings of representative episodes of open suction (A) and in-line suction (B) during TCPLV, showing key time points at which end-expiratory lung volume (EELV) was determined. *Baseline EELV; **disconnection of the ventilator circuit (open suction); †insertion of suction catheter (closed suction); ‡suction onset; §point of minimum volume during the procedure; ∥end of the procedure, defined as reconnection of the ventilator circuit (open suction) or complete withdrawal of the catheter (closed suction); ¶10-s intervals from completion of the procedure. All measurements are expressed as change in volume relative to baseline EELV (ΔVL). Arrows indicate single-point measurements. Gray bars indicate EELV averaged over 3 ventilator inflations (TCPLV) or 3 s (HFOV).
RESULTS
The 12 animals had a weight (mean ± SD) of 5.02 ± 0.54 kg. Alveolar-arterial oxygen difference before experimentation was 548 ± 91 mm Hg during TCPLV and 445 ± 135 mm Hg during HFOV. During TCPLV, PIP was 26.7 ± 4.7 cm H2O and PEEP 8.9 ± 1.2 cm H2O. During HFOV, Paw was 24.7 ± 3.7 cm H2O. Animals suctioned with a pressure of 140 mm Hg were ventilated with higher pressures than those in the other group (PIP 30.0 ± 1.1 versus 23.4 ± 4.7; PEEP 9.7 ± 1.0 versus 8.1 ± 0.8; and Paw 27.2 ± 1.3 versus 22.2 ± 3.7) but in all other respects, the groups were similar. There was no association between ventilator pressures and volume loss.
Univariate analysis.
Figure 2 shows the effect of each suction variable on ΔVL over time, using pooled data from all experimental permutations. All suction techniques resulted in significant changes in lung volume during both TCPLV and HFOV (p < 0.0001, repeated measures ANOVA). Similar patterns of ΔVL were noted during both ventilation modes, with greater volume losses overall recorded during HFOV.
ΔVL over time during TCPLV (panels A, C, and E) and HFOV (panels B, D, and F). Each data point represents mean ± SEM for all experimental permutations of suction method (panels A and B), catheter size (panels C and D), and suction pressure (panels E and F) (n = 36 per data point). Panels A and B, ΔVL with different suction methods. Circles, closed suction with in-line catheter; triangles, closed suction with side-port adaptor; and squares, open suction. Panels C and D, ΔVL with different catheter sizes. Circles, 6 FG; triangles, 7 FG; squares, 8 FG. Panels E and F, ΔVL with different suction pressures. Circles, 80 mm Hg; triangles, 140 mm Hg; squares, 200 mm Hg. TCPLV, time-cycled pressure-limited ventilation; HFOV, high-frequency oscillatory ventilation.
Open suction resulted in greater loss of volume and lower values of ΔVL60 than either closed method during both TCPLV (Fig. 2A) and HFOV (Fig. 2B) (p < 0.0001, all comparisons). The majority of volume loss with open suction (77.2 ± 12.2% of the total during TCPLV and 83.4 ± 10.1% during HFOV, mean ± SD) occurred during disconnection of the ventilator circuit before suction. No differences were found between the two closed suction methods, and data from the two methods were combined for further statistical analysis.
Catheter size influenced ΔVL during both TCPLV (Fig. 2C) and HFOV (Fig. 2D). The 8-FG catheter resulted in lower minimum volume (p < 0.0001 both ventilation modes) and ΔVL60 (p < 0.0001 TCPLV, p = 0.0012 HFOV) than either the 6-FG or the 7-FG.
Suction pressure did not influence either minimum volume or ΔVL60 during TCPLV (Fig. 2E). During HFOV (Fig. 2F), smaller losses resulted from a pressure of 80 mm Hg than the other two pressures (p = 0.028). ΔVL60 did not differ between pressures.
Multivariate analysis.
Discrete data from each combination of catheter size, suction method, and suction pressure are shown in Figure 3, with values for minimum volume and ΔVL60 displayed in Table 1. Analysis of the separate and combined effects of suction variables on lung volume revealed a different pattern for open and closed suction. With open suction, neither catheter size nor suction pressure influenced either minimum volume or ΔVL60 during either ventilation mode. With closed suction, volume loss increased with increasing catheter size and suction pressure (p < 0.001 all comparisons), with the interaction between catheter size and pressure of borderline significance (p = 0.054) during TCPLV and highly significant during HFOV (p = 0.0001). ΔVL60 was independently affected by catheter size (p < 0.0001 TCPLV and HFOV) and suction pressure (p = 0.004 TCPLV; p = 0.0058 HFOV).
ΔVL over time during TCPLV (panels A, B, and C) and HFOV (panels D, E, and F) with each individual combination of catheter size, suction method, and suction pressure (n = 6 per data point for open suction and 12 for closed suction). Panels A and D, 6 FG; Panels B and E, 7 FG; Panels C and F, 8 FG. Open suction is represented by open symbols, closed suction by gray symbols. Circles, 80 mm Hg; triangles, 140 mm Hg; squares, 200 mm Hg. All data represented as mean ± SEM. TCPLV, time-cycled pressure-limited ventilation; HFOV, high-frequency oscillatory ventilation.
With an 8-FG catheter, volume loss was equivalent with open and closed suction at vacuum pressures of 140 and 200 mm Hg during both TCPLV and HFOV. At 80 mm Hg, closed suction resulted in less volume loss than open suction. During TCPLV, ΔVL60 did not differ between open and closed suction; during HFOV, ΔVL60 was higher with closed suction than open only at a vacuum pressure of 80 mm Hg.
At 60 s after completion of the suction procedure, lung volume was restored to ≥90% of baseline in 46 episodes (28.6%) during TCPLV and 47 episodes (29.2%) during HFOV. Results of the logistic regression are shown in Table 2. During TCPLV, closed suction was more likely to be associated with restoration of lung volume, but this effect was modified by increasing catheter size; catheter size itself had no independent effect. Increasing suction pressure slightly reduced the probability of lung volume being restored, whereas increasing PIP increased its probability. During HFOV, restoration of lung volume was more likely to occur during closed suction, and with increasing Paw. There was a trend toward an increase in restoration of lung volume with both 6-and 7-FG catheters compared with the 8-FG but this did not reach statistical significance.
DISCUSSION
This study examined the individual and combined effects of suction variables on lung volume. Overall, open suction resulted in a greater loss of lung volume than closed suction and was associated with residual deficit 1 min after completion of the procedure. However, the difference between suction methods diminished as both catheter size and suction pressure increased and was not apparent when using an 8-FG catheter at suction pressures of 140 or 200 mm Hg, that is, under conditions likely to be used in clinical practice. In this sense, we contend that the use of closed suction in the clinical setting may not guarantee preservation of lung volume in infants and small children.
Larger catheters, that occlude more of the ETT lumen, have been shown in vitro to generate high negative airway pressures during both open and closed suction (15–17). In adults, it is recommended that the diameter of the suction catheter should be less than half that of the ETT (35). This ratio cannot be achieved with the smallest ETT sizes and is generally seen as impractical with ETT sizes ≤4.0 mm; most authorities recommend either an 8- or a 10-FG be used with a 4.0-mm ETT (21,23,24,26,27,36). Our findings tend to support more recent recommendations for the use of smaller catheters whenever possible (22), at least with respect to closed suction. We found suction pressure had less influence on lung volume loss than catheter size. The range of pressures studied may have been too narrow to show greater differences. Importantly, we found an interaction between catheter size and suction pressure in determining volume loss with closed suction. It was notable that, when using the two smaller catheters at the highest pressure, volume loss was less than or similar to that generated by an 8-FG catheter at the lowest pressure. Guidelines generally seem to treat the two variables as independent entities, recommending severe restriction of suction pressure regardless of catheter size (25–27,36). Our findings support our previous contention that catheter size and suction pressure should be considered in relation to each other (15).
With open suction, lung volume changes were unaffected by catheter size or suction pressure. This finding is consistent with a study of oxygenation and hemodynamic changes with suction in ventilated children (4) but is somewhat surprising in light of in vitro studies (15,17). In contrast, in another pediatric study catheter size was implicated in reduction in dynamic compliance after suction (19). The suction pressure in this study was 360 mm Hg (48 kPa), higher than in our study or that of Singh et al. (4). In a nonrandomized study, right upper lobe collapse occurred in fewer children when suction pressure was limited to 120 mm Hg than when pressure was unregulated (18).
Lung rerecruitment following suction is as important a consideration as derecruitment during the procedure. Both open and closed techniques were associated with persistent volume deficit at 1-min postsuction, during both conventional and high-frequency ventilation. We did not investigate the effect of recruitment maneuvers in this study, but it was notable that higher ventilator pressures (PIP or Paw) were associated with an increased likelihood of restoration of lung volume close to presuction levels. Further research is required to determine the most appropriate rerecruitment techniques, and the conditions under which they are required.
We found no difference in performance between the two closed suction methods. Similar findings were obtained in two studies in adult intensive care patients (6,7). A study in preterm infants found in-line suction resulted in less disruption to oxygenation and heart rate than suction using an adaptor (8); however, different protocols were used with each technique, which may have contributed to this finding. The cost of in-line suction systems is considerably higher than that of adaptors, which are used with ordinary disposable catheters. This cost is difficult to justify on current evidence. However, the relative effects of the two techniques on other outcomes, such as infection, should be established before recommendations can be made.
ETT suction is performed to remove secretions, and effectiveness must be taken into consideration when choosing specific techniques. Animal and in vitro data suggest closed suction is less effective than open when used under similar conditions (20,37). Little is known of the effectiveness of various combinations of catheter size and suction pressure, and further research on this topic is warranted.
A strength of our study is that we standardized the volume state of the lung, rather than ventilating with standard pressures, the first study to our knowledge to do so. Despite the standardization of the model, lung volume loss varied considerably between animals, suggesting the involvement of factors additional to those we measured. Moreover, it cannot be assumed that similar results would be seen with absent or different lung pathology, or with a different ventilation strategy.
Our study had some limitations. First, all animals in our study were muscle relaxed, which is not routine in current neonatal ventilatory management. In a study of ventilated neonates, a minority of whom were muscle relaxed, we found lung volume was restored in a shorter timeframe than we have described here (14); however, no studies have directly compared lung volume changes in muscle relaxed and spontaneously breathing subjects. Second, data were obtained from only one pass of the suction catheter; in clinical practice a suction episode consists of 2–3 passes on average. The effect of repeated catheter passes on lung volume change remains to be determined. Third, we did not account for the effect of secretions, the volume of which was observed to vary during the experiment. Aspiration of mucus into the suction catheter is likely to limit the negative pressure generated in the airway and thus may reduce the overall volume loss. In the clinical setting, accumulated secretions can reduce the diameter of the ETT, and if not aspirated, will increase the pressure transmitted to the trachea, potentially increasing volume loss; however, this scenario was unlikely during our experiment because of the frequency with which suction was performed.
Finally, the limitations of RIP need to be considered. RIP measures change in total thoracic volume and cannot distinguish between gas and fluid changes. Changes in thoracic blood volume may have contributed to RIP changes during our experimental protocol. The summed RIP voltage output was calibrated to a known volume at the airway opening during TCPLV, a simple and practical method over short time periods (28,38). Whether the derived calibration factor, which assumes an equal weighting of each RIP signal, remains constant over prolonged periods in severe lung disease states has been questioned, especially during HFOV (31). Irrespective, the raw summed RIP voltage signal is a validated method of assessing global ΔVL over time (29,39). RIP cannot determine where, within the lung, any volume change may occur. Electrical impedance tomography, which allows determination of regional ΔVL, may be an alternative to RIP in the future (13,40,41).
In conclusion, this study in ventilated neonatal piglets found that lung volume changes during endotracheal suction can be influenced by catheter size and suction pressure, as well as suction method. With catheter sizes and suction pressures commonly used in clinical practice, closed suction did not preserve lung volume.
Abbreviations
- ΔVL:
-
change in end-expiratory lung volume
- ΔVL60:
-
change in end-expiratory lung volume 60 seconds after suction
- ETT:
-
endotracheal tube
- FG:
-
French gauge
- HFOV:
-
high-frequency oscillatory ventilation
- Paw:
-
mean airway pressure
- PEEP:
-
positive end-expiratory pressure
- PIP:
-
peak inspiratory pressure
- RIP:
-
respiratory inductive plethysmography
- TCPLV:
-
time-cycled pressure-limited ventilation
References
Brandstater B, Muallem M 1969 Atelectasis following tracheal suction in infants. Anesthesiology 31: 468–473
Kerem E, Yatsiv I, Goitein KJ 1990 Effect of endotracheal suctioning on arterial blood gases in children. Intensive Care Med 16: 95–99
Simbruner G, Coradello H, Fodor M, Havelec L, Lubec G, Pollak A 1981 Effect of tracheal suction on oxygenation, circulation, and lung mechanics in newborn infants. Arch Dis Child 56: 326–330
Singh NC, Kissoon N, Frewen T, Tiffin N 1991 Physiological responses to endotracheal and oral suctioning in paediatric patients: the influence of endotracheal tube sizes and suction pressures. Clin Intensive Care 2: 345–350
Paul-Allen J, Ostrow CL 2000 Survey of nursing practices with closed-system suctioning. Am J Crit Care 9: 9–19
Fernandez MD, Piacentini E, Blanch L, Fernandez R 2004 Changes in lung volume with three systems of endotracheal suctioning with and without pre-oxygenation in patients with mild-to-moderate lung failure. Intensive Care Med 30: 2210–2215
Maggiore SM, Lellouche F, Pigeot J, Taille S, Deye N, Durrmeyer X, Richard JC, Mancebo J, Lemaire F, Brochard L 2003 Prevention of endotracheal suctioning-induced alveolar derecruitment in acute lung injury. Am J Respir Crit Care Med 167: 1215–1224
Tan AM, Gomez JM, Mathews J, Williams M, Paratz J, Rajadurai VS 2005 Closed versus partially ventilated endotracheal suction in extremely preterm neonates: physiologic consequences. Intensive Crit Care Nurs 21: 234–242
Kalyn A, Blatz S, Feuerstake S, Paes B, Bautista C 2003 Closed suctioning of intubated neonates maintains better physiologic stability: a randomized trial. J Perinatol 23: 218–222
Woodgate PG, Flenady V 2001 Tracheal suctioning without disconnection in intubated ventilated neonates. Cochrane Database Syst Rev CD003065
Cereda M, Villa F, Colombo E, Greco G, Nacoti M, Pesenti A 2001 Closed system endotracheal suctioning maintains lung volume during volume-controlled mechanical ventilation. Intensive Care Med 27: 648–654
Choong K, Chatrkaw P, Frndova H, Cox PN 2003 Comparison of loss in lung volume with open versus in-line catheter endotracheal suctioning. Pediatr Crit Care Med 4: 69–73
Wolf GK, Grychtol B, Frerichs I, van Genderingen HR, Zurakowski D, Thompson JE, Arnold JH 2007 Regional lung volume changes in children with acute respiratory distress syndrome during a derecruitment maneuver. Crit Care Med 35: 1972–1978
Hoellering AB, Copnell B, Dargaville PA, Mills JF, Morley CJ, Tingay DG 2008 Lung volume and cardiorespiratory changes during open and closed endotracheal suction in ventilated newborn infants. Arch Dis Child Fetal Neonatal Ed 93: F436–F441
Kiraly NJ, Tingay DG, Mills JF, Morley CJ, Copnell B 2008 Negative tracheal pressure during neonatal endotracheal suction. Pediatr Res 64: 29–33
Monaco FJ, Meredith KS 1992 A bench test evaluation of a neonatal closed tracheal suction system. Pediatr Pulmonol 13: 121–123
Morrow BM, Futter MJ, Argent AC 2004 Endotracheal suctioning: from principles to practice. Intensive Care Med 30: 1167–1174
Boothroyd AE, Murthy BV, Darbyshire A, Petros AJ 1996 Endotracheal suctioning causes right upper lobe collapse in intubated children. Acta Paediatr 85: 1422–1425
Morrow B, Futter M, Argent A 2006 Effect of endotracheal suction on lung dynamics in mechanically-ventilated paediatric patients. Aust J Physiother 52: 121–126
Lindgren S, Almgren B, Hogman M, Lethvall S, Houltz E, Lundin S, Stenqvist O 2004 Effectiveness and side effects of closed and open suctioning: an experimental evaluation. Intensive Care Med 30: 1630–1637
Goldsmith J, Karotkin E 1996 Assisted Ventilation of the Neonate. W.B. Saunders, Philadelphia pp 116–117
Morrow BM, Argent AC 2008 A comprehensive review of pediatric endotracheal suctioning: effects, indications, and clinical practice. Pediatr Crit Care Med 9: 465–477
Runton N 1992 Suctioning artificial airways in children: appropriate technique. Pediatr Nurs 18: 115–118
Shann F 2005 Drug Doses, 13th Ed. Collective Pty Ltd, Melbourne
Turner BS 1990 Maintaining the artificial airway: current concepts. Pediatr Nurs 16: 487–493
Wallace JL 1998 Suctioning—a two-edged sword: reducing the theory-practice gap. J Neonatal Nurs 4: 12–17
Young CS 1984 Recommended guide lines for suction. Physiotherapy 70: 106–108
Tingay DG, Copnell B, Mills JF, Morley CJ, Dargaville PA 2007 Effects of open endotracheal suction on lung volume in infants receiving HFOV. Intensive Care Med 33: 689–693
Tingay DG, Mills JF, Morley CJ, Pellicano A, Dargaville PA 2006 Describing the deflation limb of the pressure volume relationship in newborn infants receiving HFOV. Am J Respir Crit Care Med 173: 414–420
Leino K, Nunes S, Valta P, Takala J 2001 Validation of a new respiratory inductive plethysmograph. Acta Anaesthesiol Scand 45: 104–111
Markhorst DG, Van Gestel JP, Van Genderingen HR, Haitsma JJ, Lachmann B, Van Vught AJ 2006 Respiratory inductive plethysmography accuracy at varying PEEP levels and degrees of acute lung injury. J Med Eng Technol 30: 166–175
Goddon S, Fujino Y, Hromi J, Kacmarek R 2001 Optimal mean airway pressure during high-frequency oscillation: predicted by the pressure-volume curve. Anesthesiology 94: 862–869
De Jaegere A, van Veenendaal MB, Michiels A, van Kaam AH 2006 Lung recruitment using oxygenation during open lung high-frequency ventilation in preterm infants. Am J Respir Crit Care Med 174: 639–645
van Kaam AH, De Jaegere A, Haitsma JJ, van Aalderen WM, Kok JH, Lachmann B 2003 Positive pressure ventilation with the open lung concept optimizes gas exchange and reduces ventilator-induced lung injury in newborn piglets. Pediatr Res 53: 245–253
Vanner R, Bick E 2008 Tracheal pressures during open suctioning. Anaesthesia 63: 313–315
Hodge D 1991 Endotracheal suctioning and the infant: a nursing care protocol to decrease complications. Neonatal Netw 9: 7–15
Copnell B, Tingay DG, Kiraly NJ, Sourial M, Gordon MJ, Mills JF, Morley CJ, Dargaville PA 2007 A comparison of the effectiveness of open and closed endotracheal suction. Intensive Care Med 33: 1655–1662
Sackner MA, Watson H, Belsito AS, Feinerman D, Suarez M, Gonzalez G, Bizousky F, Krieger B 1989 Calibration of respiratory inductive plethysmograph during natural breathing. J Appl Physiol 66: 410–420
Brazelton TB, Watson KF, Murphy M, Al Khadra E, Thompson JE, Arnold JH 2001 Identification of optimal lung volume during high-frequency oscillatory ventilation using respiratory inductive plethysmography. Crit Care Med 29: 2349–2359
Frerichs I, Dargaville PA, van Genderingen H, Morel DR, Rimensberger PC 2006 Lung volume recruitment after surfactant administration modifies spatial distribution of ventilation. Am J Respir Crit Care Med 174: 772–779
Lindgren S, Odenstedt H, Olegard C, Sundergaard S, Lundin S, Stenqvist O 2007 Regional lung derecruitment after endotracheal suction during volume- or pressure-controlled ventilation: a study using electric impedance tomography. Intensive Care Med 33: 172–180
Acknowledgements
We thank Mr Magdy Sourial and the staff of the Murdoch Childrens Research Institute Animal Research Facility for assistance with animal preparation, Scott Dunlop and Michael Gordon for assistance with the experiments, and Associate Professor Damien Jolley of the School of Public Health and Preventive Medicine, Monash University, for statistical advice.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by an unconditional Murdoch Children's Research Institute project grant (Grant ID 05028), and in part by National Health and Medical Research Council program grant 384100 (B.C.) and a National Health and Medical Research Council Medical Postgraduate Research Scholarship (D.G.T.).
Rights and permissions
About this article
Cite this article
Copnell, B., Dargaville, P., Ryan, E. et al. The Effect of Suction Method, Catheter Size, and Suction Pressure on Lung Volume Changes During Endotracheal Suction in Piglets. Pediatr Res 66, 405–410 (2009). https://doi.org/10.1203/PDR.0b013e3181b337b9
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e3181b337b9
This article is cited by
-
Can ventilator settings reduce the negative effects of endotracheal suctioning? Investigations in a mechanical lung model
BMC Anesthesiology (2015)
-
Endotracheal suctioning in hypoxemic patients
Réanimation (2011)
-
The effect of endotracheal suction on regional tidal ventilation and end-expiratory lung volume
Intensive Care Medicine (2010)