Abstract
Background
To compare tidal volume (VT) delivery with compliance at 0.5 and 1.5 mL/cmH2O using four different ventilation (PPV) devices (i.e., self-inflating bag (SIB), T-Piece resuscitator, Next Step (a novel Neonatal Resuscitator), and Fabian ventilator (conventional neonatal ventilator) using a neonatal piglet model.
Design/methods
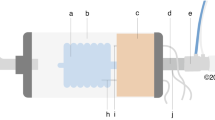
Randomized experimental animal study using 10 mixed-breed neonatal piglets (1–3 days; 1.8–2.4 kg). Piglets were anesthetized, intubated, instrumented, and randomized to receive positive pressure ventilation (PPV) for one minute with a SIB with or without a respiratory function monitor (RFM), T-Piece resuscitator with or without an RFM, Next Step, and Fabian Ventilator with both compliance levels. Compliance changes were achieved by placing a wrap around the piglets’ chest and tightened it. Our primary outcome was targeted VT delivery of 5 mL/kg at 0.5 and 1.5 mL/cmH2O lung compliance.
Results
At 0.5 mL/cmH2O compliance, the mean(SD) expired VT with the Next Step was 5.1(0.2) mL/kg compared to the Fabian 4.8(0.5) mL/kg, SIB 8.9(3.6) mL/kg, SIB + RFM 4.5(1.8) mL/kg, T-Piece 7.4(4.3) mL/kg, and T-Piece+RFM 6.4(3.1) mL/kg. At 1.5 mL/cmH2O compliance, the mean(SD) expired VT with the Next Step was 5.2(0.6) mL/kg compared to the Fabian 4.4(0.7) mL/kg, SIB 12.1(5.3) mL/kg, SIB + RFM 9.4(3.9) mL/kg, T-Piece 8.6(1.5) mL/kg, and T-Piece+RFM 6.5 (1.6) mL/kg.
Conclusion
The Next Step provides consistent VT during PPV, which is comparable to a mechanical ventilator.
Impact
-
Current guidelines recommend fixed peak inflation pressure in resuscitation, linked to lung and brain injury.
-
The Next Step Neonatal Resuscitator, a cost-effective device, offers volume-targeted positive pressure ventilation with consistent tidal volumes.
-
With two different compliances, the Next Step Neonatal Resuscitator delivered a consistent tidal volume which was similar to a mechanical ventilator.
-
The Next Step Neonatal Resuscitator outperformed self-inflating bags and T-Pieces in delivering targeted tidal volumes.
-
The Next Step Neonatal Resuscitator could be an alternative ventilation device for neonatal resuscitation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article. Data used to generate the results reported in this study will be made available following publication to researchers who provide a methodologically sound proposal.
References
Aziz, K., Chadwick, M., Baker, M. & Andrews, W. Ante- and intra-partum factors that predict increased need for neonatal resuscitation. Resuscitation 79, 444–452 (2008).
Schmölzer, G. M., te Pas, A. B., Davis, P. G. & Morley, C. J. Reducing lung injury during neonatal resuscitation of preterm infants. J. Pediatr. 153, 741–745 (2008).
Schmölzer, G. M. et al. Assessment of tidal volume and gas leak during mask ventilation of preterm infants in the delivery room. Arch. Dis. Child - Fetal Neonatal Ed. 95, F393 (2010).
Dawson, J. A. et al. Oxygenation with T-Piece versus Self-Inflating Bag for Ventilation of Extremely Preterm Infants at Birth: A Randomized Controlled Trial. J. Pediatr. 158, 912–918.e2 (2011).
Poulton, D. A., Schmölzer, G. M., Morley, C. J. & Davis, P. G. Assessment of chest rise during mask ventilation of preterm infants in the delivery room. Resuscitation 82, 175–179 (2011).
Kaufman, J., Schmölzer, G. M., Kamlin, C. O. F. & Davis, P. G. Mask ventilation of preterm infants in the delivery room. Arch. Dis. Child Fetal Neonatal Ed. 98, F405–F410 (2013). Sep.
Weiner, Zaichkin. Textbook of Neonatal Resuscitation (NRP), 7th Ed. 7th ed. American Academy of Pediatrics; (2016).
Madar, J. et al. European Resuscitation Council Guidelines 2021: Newborn resuscitation and support of transition of infants at birth. Resuscitation 161, 291–326 (2021).
Björklund, L. J. et al. Manual Ventilation with a Few Large Breaths at Birth Compromises the Therapeutic Effect of Subsequent Surfactant Replacement in Immature Lambs. Pediatr. Res. 42, 348–355 (1997).
Hernandez, L. A., Peevy, K. J., Moise, A. A. & Parker, J. C. Chest wall restriction limits high airway pressure-induced lung injury in young rabbits. J. Appl. Physiol. 66, 2364–2368 (1989).
Polglase, G. R. et al. Initiation of resuscitation with high tidal volumes causes cerebral hemodynamic disturbance, brain inflammation and injury in preterm lambs. PLoS ONE 7, e39535 (2012).
Mian, Q. et al. Impact of delivered tidal volume on the occurrence of intraventricular haemorrhage in preterm infants during positive pressure ventilation in the delivery room. Arch. Dis. Child - Fetal Neonatal Ed. 104, F57 (2018).
Hooper, S. B. et al. Expired CO2 levels indicate degree of lung aeration at birth. PLOS ONE 8, e70895 (2013).
Hooper, S. B., te Pas, A. B. & Kitchen, M. J. Respiratory transition in the newborn: a three-phase process. Arch. Dis. Child - Fetal Neonatal Ed. 101, F266 (2016).
te Pas, A. B. et al. Establishing Functional Residual Capacity at Birth: The Effect of Sustained Inflation and Positive End-Expiratory Pressure in a Preterm Rabbit Model. Pediatr. Res. 65, 537–541 (2009).
Schmölzer, G. M. et al. Respiratory monitoring of neonatal resuscitation. Arch. Dis. Child Fetal Neonatal Ed. 95, F295–F303 (2010).
Bowman, T. A., Paget-Brown, A., Carroll, J., Gurka, M. J. & Kattwinkel, J. Sensing and responding to compliance changes during manual ventilation using a lung model: can we teach healthcare providers to improve? J. Pediatr. 160, 372–376.e1 (2012).
Kattwinkel, J., Stewart, C., Walsh, B., Gurka, M. & Paget-Brown, A. Responding to Compliance Changes in a Lung Model During Manual Ventilation: Perhaps Volume, Rather Than Pressure, Should be Displayed. Pediatrics 123, e465–e470 (2009).
Schmölzer, G. M. et al. Respiratory function monitor guidance of mask ventilation in the delivery room: a feasibility study. J. Pediatr. 160, 377–381.e2 (2012).
Sarrato, G. Z. et al. New Strategies of Pulmonary Protection of Preterm Infants in the Delivery Room with the Respiratory Function Monitoring. Am. J. Perinatol. 36, 1368–1376 (2019).
van Zanten, H. A. et al. A multi-centre randomised controlled trial of respiratory function monitoring during stabilisation of very preterm infants at birth. Resuscitation 167, 317–325 (2021).
de Medeiros, S. M. et al. Respiratory function monitoring to improve the outcomes following neonatal resuscitation: a systematic review and meta-analysis. Arch. Dis. Child Fetal Neonatal Ed. 107, 589–596 (2022).
Gupta, A. & Keszler, M. Survey of Ventilation Practices in the Neonatal Intensive Care Units of the United States and Canada: Use of Volume-Targeted Ventilation and Barriers to Its Use. Am. J. Perinatol. 36, 484–489 (2018).
Klingenberg, C., Wheeler, K. I., McCallion, N., Morley, C. J. & Davis, P. G. Volume‐targeted versus pressure‐limited ventilation in neonates. Cochrane Db Syst. Rev. 2017, CD003666 (2017).
Law B. H. Y., Kia T. M., Trinh F. & Schmölzer G. M. Mask ventilation using volume-targeted neonatal ventilator for neonatal resuscitation: a randomised cross-over simulation study. Arch Dis Child - Fetal Neonatal Ed. fetalneonatal-2023-325320 (2023).
Law B. H. Y. & Schmölzer G. M. Volume-targeted mask ventilation during simulated neonatal resuscitation. Arch Dis Child - Fetal Neonatal Ed. fetalneonatal-2023-325902 (2023).
Solevåg, A. et al. A Novel Prototype Neonatal Resuscitator That Controls Tidal Volume and Ventilation Rate: A Comparative Study of Mask Ventilation in a Newborn Manikin. Front. Pediatr. 4, 129 (2016).
Solevåg, A. et al. Comparison of positive pressure ventilation devices in a newborn manikin. J. Matern.-Fetal Neonatal Med. 30, 595–599 (2017).
Kilkenny, C., Altman, D. G., Browne, W. J., Cuthill, I. C. & Emerson, M. Improving Bioscience Research Reporting: The ARRIVE Guidelines for Reporting Animal Research. PLoS Biol. 8, e1000412 (2010).
Cheung, P. Y., Gill, R. S. & Bigam, D. L. A swine model of neonatal asphyxia. J. Vis. Exp. 3166, https://doi.org/10.3791/3166 (2011).
Schmölzer, G. M. et al. Cardiopulmonary resuscitation with chest compressions during sustained inflations: a new technique of neonatal resuscitation that improves recovery and survival in a neonatal porcine model. Circulation 128, 2495–2503 (2013).
Os, S. et al. Exhaled carbon dioxide can be used to guide respiratory support in the delivery room. Acta Paediatr. 103, 796–806 (2014).
Bresesti, I. et al. Pressure and tidal volume delivery in extremely preterm infants at birth using different t-piece resuscitation devices. Early Hum. Dev. 183, 105794 (2023).
Cavigioli, F. et al. Tidal volume optimization and heart rate response during stabilization of very preterm infants. Pediatr. Pulmonol. 58, 550–555 (2023).
Huynh, T., Huynh, T., Hemway, R. J. & Perlman, J. M. Assessment of effective face mask ventilation is compromised during synchronised chest compressions. Arch. Dis. Child. Fetal Neonatal. Ed. 100, F39–F42 (2015).
Law, B. H. Y. et al. Analysis of neonatal resuscitation using eye tracking: a pilot study. Arch. Dis. Child - Fetal Neonatal. Ed. 103, F82 (2018).
Herrick, H. et al. Provider visual attention on a respiratory function monitor during neonatal resuscitation. Arch. Dis. Child - Fetal Neonatal. Ed. 105, 666–668 (2020).
Verbeek, C. et al. Accuracy of currently available neonatal respiratory function monitors for neonatal resuscitation. Eur. J. Pediatr. 175, 1065–1070 (2016).
Funding
We received funding from KM Medical, Auckland, New Zealand to perform the study. The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. K.H.T. is a recipient of a Graduate Scholarship (University of Alberta), a Graduate Scholarship (University of Alberta Faculty of Medicine and Dentistry), a Canada Graduate Scholarships-Master’s program (Canadian Institutes of Health Research), and a Walter H Johns Graduate Fellowship (University of Alberta). M.R. is a recipient of a Graduate Scholarship (University of Alberta), a Graduate Scholarship (University of Alberta Faculty of Medicine and Dentistry), a Canada Graduate Scholarships-Master’s program (Canadian Institutes of Health Research), and a Walter H Johns Graduate Fellowship (University of Alberta). Conception and design: G.M.S., B.L.; Collection and assembly of data: G.M.S., B.L., M.R., K.T.; Analysis and interpretation of the data: G.M.S., B.L., M.R., K.T.; Drafting of the 1st draft: K.T.; Critical revision of the article for important intellectual content: G.M.S., B.L., M.R., K.T. Final approval of the article: G.M.S., B.L., M.R., K.T.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tran, K.H., Ramsie, M., Law, B. et al. Comparison of positive pressure ventilation devices during compliance changes in a neonatal ovine model. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03028-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-024-03028-3