Abstract
Background
The importance of neonatal resuscitator resistance is currently unknown. In this study we investigated peak flows and pressure stability resulting from differences in imposed resistance during positive pressure ventilation(PPV) and simulated spontaneous breathing (SSB) between the r-PAP, low-resistance resuscitator, and Neopuff™, high-resistance resuscitator.
Methods
In a bench test, 20 inflations during PPV and 20 breaths during SSB were analysed on breath-by-breath basis to determine peak flow and pressure stability using the Neopuff™ with bias gas flow of 8, 12 or 15 L/min and the r-PAP with total gas flow of 15 L/min.
Results
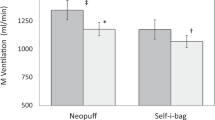
Imposed resistance of the Neopuff™ was significantly reduced when the bias gas flow was increased from 8 to 15 L/min, which resulted in higher peak flows during PPV and SSB. Peak flows in the r-PAP were, however, significantly higher and fluctuations in CPAP during SSB were significantly smaller in the r-PAP compared to the Neopuff™ for all bias gas flow levels. During PPV, a pressure overshoot of 3.2 cmH2O was observed in the r-PAP.
Conclusions
The r-PAP seemed to have a lower resistance than the Neopuff™ even when bias gas flows were increased. This resulted in more stable CPAP pressures with higher peak flows when using the r-PAP.
Impact
-
The traditional T-piece system (Neopuff™) has a higher imposed resistance compared to a new neonatal resuscitator (r-PAP).
-
This study shows that reducing imposed resistance leads to smaller CPAP fluctuations and higher inspiratory and expiratory peak flows.
-
High peak flows might negatively affect lung function and/or cause lung injury in preterm infants at birth. This study will form the rationale for further studies investigating these effects.
-
A possible compromise might be to use the traditional T-piece system with a higher bias gas flow (12 L/min), thereby reducing the imposed resistance and generating more stable PEEP/CPAP pressures, while limiting potentially harmful peak flows.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Kuypers, K. L. A. M. et al. The effect of a higher bias gas flow on imposed T-piece resistance and breathing in preterm infants at birth. Front. Pediatr. 10, 817010 (2022).
Hinder, M., McEwan, A., Drevhammer, T., Donaldson, S. & Tracy, M. B. T-piece resuscitators: how do they compare? Arch. Dis. Child Fetal Neonatal Ed. 104, F122–F7 (2019).
Drevhammar, T., Nilsson, K., Zetterström, H. & Jonsson, B. Comparison of seven infant continuous positive airway pressure systems using simulated neonatal breathing. Pediatr. Crit. Care Med. 13, e113–e119 (2012).
Wald, M. et al. Variety of expiratory resistance between different continuous positive airway pressure devices for preterm infants. Artif. Organs 35, 22–28 (2011).
Donaldsson, S., Drevhammar, T., Taittonen, L., Klemming, S. & Jonsson, B. Initial stabilisation of preterm infants: a new resuscitation system with low imposed work of breathing for use with face mask or nasal prongs. Arch. Dis. Child. Fetal Neonatal Ed. 102, F203–F207 (2017).
Donaldsson, S. et al. Comparison of respiratory support after delivery in infants born before 28 weeks’ gestational age: The CORSAD Randomized Clinical Trial. JAMA Pediatr. 175, 911–918 (2021).
Basser, P. J., McMahon, T. A. & Griffith, P. The mechanism of mucus clearance in cough. J. Biomech. Eng. 111, 288–297 (1989).
Huckstadt, T., Foitzik, B., Wauer, R. R. & Schmalisch, G. Comparison of two different CPAP systems by tidal breathing parameters. Intensive Care Med. 29, 1134–1140 (2003).
Ferhardt, T., Reifenberg, L., Hehre, D., Feller, R. & Bancalari, E. Functional residual capacity in normal neonates and children up to 5 years of age determined by N2 washout method. Pediatr. Res. 20, 668–671 (1986).
LoMauro, A. & Aliverti, A. Physiology masterclass: extremes of age: newborn and infancy. Breathe (Sheff.) 12, 65–68 (2016).
Hinder, M. K. et al. T-piece resuscitators: can they provide safe ventilation in a low compliant newborn lung? Arch. Dis. Child Fetal Neonatal. Ed. 106, 25–30 (2021).
Drevhammar, T., Berg, N., Nilsson, K., Jonsson, B. & Prahl Wittberg, L. Flows and function of the infant flow neonatal continuous positive airway pressure device investigated with computational fluid dynamics. Acta Paediatr. (Oslo, Nor. : 1992) 110, 811–817 (2021).
Funding
This work was supported by Fisher & Paykel Healthcare Limited by an unrestricted grant. Fisher & Paykel Healthcare Limited had no role in study design nor in the collection, analysis, and interpretation of data, writing of the manuscript and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
K.K.: co-conceived the study, conducted the study, collected, analysed and interpreted the data, wrote the first draft of the manuscript and approved the final version of the manuscript. A.K.: co-conceived the study, conducted the study, collected and interpreted the data, reviewed and edited the manuscript and approved the final version of the manuscript. S.C.: data interpretation, reviewed and edited the manuscript and approved the final version of the manuscript. S.H.: co-conceived the study, supervised the study, interpreted the data, reviewed and edited the manuscript and approved the final version. A.B.t.P.: co-conceived the study, supervised the study, interpreted the data, reviewed and edited the first draft of the manuscript and approved the final version. All authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
K.L.A.M. Kuypers is the recipient of an unrestricted research grant from Fisher & Paykel Healthcare Limited; they had no role in study design nor in the collection, analysis, and interpretation of data, writing of the report and decision to submit the paper for publication.
Ethics approval and consent to participate
Patient consent was not required for this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kuypers, K.L.A.M., Kashyap, A.J., Cramer, S.J.E. et al. The effect of imposed resistance in neonatal resuscitators on pressure stability and peak flows: a bench test. Pediatr Res 94, 1929–1934 (2023). https://doi.org/10.1038/s41390-023-02715-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02715-x