Abstract
Mechanisms underlying the pathophysiology of minimal-change nephrotic syndrome (MCNS), the most frequent glomerular disease in children, remain elusive, but recent findings argue for a T cell dysfunction. Starting from a differential cDNA library from T cells of a patient under relapse and remission, we identified 16 transcripts specific for MCNS. All of these transcripts that were selectively up-regulated during the relapse phase of the disease were generated by alternative splicing of known genes. This abnormal RNA expression was associated with a down-regulation of serin-rich protein 75 and serin-rich protein 40, two proteins involved in mRNA splicing. Taken together, these data suggest that T cell dysfunction in MCNS is associated with abnormal mRNA splicing.
Similar content being viewed by others
Main
Our understanding of biologic mechanisms that govern physiologic functions as well as pathologic situations has become more complex with recent insights from genome sequencing projects. In particular, it seems that alternative splicing plays a determinant role in the diversity and the complexity of higher organisms (1).
Alternative splicing displays a strong tissue specificity or involvement at a defined developmental stage (2). Recent genome-wide data of human alternative pre-mRNA splicing using exon-junction microarrays indicate that at least 74% of human multi-exon genes are alternatively spliced (3). Moreover, that alternative splicing plays a crucial role in the biologic complexity of vertebrates indicates the possibility of its involvement in a large number of human diseases or pathologic processes. Thus, it has been estimated that 15–20% of disease-causing mutations in human genes involve misregulation of alternative splicing (4).
In this report, we reveal the possible involvement of abnormal RNA processing in the pathogenesis of minimal-change nephrotic syndrome (MCNS). This human glomerular disease is characterized by a heavy proteinuria with a relapsing/remitting course without histologic evidence of classical immune mechanism–mediated injury (5,6). MCNS is a sporadic disease that occurs in the context of immune activation, and its natural course argues strongly against a fixed genetic defect. It is believed that the mechanism of proteinuria involves the secretion by MCNS immune cells of factors that impair the glomerular filtration barrier (7). How the immune response culminates in MCNS by the production of pathogenic factor remains unresolved.
Recently, by analyzing a differential T cell cDNA library of a patient under relapse and remission, we identified 16 clones corresponding to unknown transcripts. The nucleotide sequences of these clones all match within intronic sequences of genes with defined or putative functions. Finally, we showed that this abnormal RNA processing is associated with a down-regulation of serin-rich protein 75 (SRp75) and SRp40 proteins that play a crucial role in pre-mRNA processing.
METHODS
Patients.
The cohort of patients analyzed in this study has been described previously (8). In all cases, informed consent was obtained, and the study was approved by the applicable Institutional Review Board.
Cell isolation, immunochemistry, and reagents.
Immunoselection of T cell subsets and antibody reagents as well as preparation and quantification of protein extracts and SDS-PAGE immunoblotting were performed as previously described (6). Anti-SR protein Mab and MAb 104 were obtained from ATCC.
RNA isolation, RT-PCR, and DNA sequencing.
Total RNAs were treated by DNase I and purified using RNeasy kit (Qiagen SA Courtaboeuf, France), following the supplier's protocol. Semiquantitative RT-PCRs and DNA sequencing were performed as previously reported (8). The sequence of primers and PCR parameters are indicated in Table 1. PCR reactions were normalized for glyceraldehyde-3-phosphate dehydrogenase expression. Nucleic acid and protein database searches were performed using resources of the National Center Biotechnology Information and the UCSC Genome Bioinformatics site (www.genome.ucsc.edu)
Library construction and screening.
Total RNA from T cell–enriched peripheral blood mononuclear cells (PBMCs) were purified and DNAse I–treated as previously described (8). First-strand cDNA synthesis was performed with Superscript reverse transcriptase (200 UI) using 4 μg of total RNA and 2 μΜ of 5′-AAGCAGTGGTATCAACGCAGAGTGGCCATTATGGCCGGG-3′ and 3′-ATTCTAGAGGCCGAGGCGGCCGACATG-dT(30)-5′ oligonucleotides. After RNA lysis, double-strand cDNA synthesis was performed by primer extension (30 min, 72°C) in 50 μL including the total first-strand reaction product, 0.2 μm of 5′-AAGCAGTGGTATCAACGCAGAGT and 5′-ATTCTAGAGGCCGAGGCGGCCGACATG-3′ PCR primers, 2 mm dNTPs, and 2 μL of TaqDNA polymerase. Double-strand cDNA was purified on a chromaspin-100 column (Clontech, Heidelberg, Germany), then ligated with EcoRI-SalI-NotI adapters (Clontech). Molecules longer than 400 bp were selected by size fractionation on a chromaspin-400 and ligated into the EcorI site of the Bluescript SK(+) plasmid (Stratagene, Amsterdam, The Netherlands). One fifth of the ligation reaction was used to transform 100 μL of XL1 blue ultracompetent cells by heat shock (Stratagene). Selected subtracted inserts obtained previously were used for screening the library according to a protocol already described (8).
RESULTS
Specific recruitment of unknown transcripts in MCNS patients.
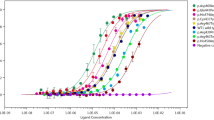
The cDNA subtractive library from MCNS T cells of patients under relapse and remission revealed 16 cDNA clones related to yet unknown transcripts. Before proceeding with any further studies, we wanted to check the specificity of these cDNA for MCNS patients. Thus, we analyzed by semiquantitative RT-PCR the expression level of these transcripts in 10 patients with MCNS, clinical characteristics of which have been previously described (9). We found an increased and specific expression of all of these transcripts in MCNS patients, whereas normal subjects or patients with membranous nephropathy (MN) exhibited very modest levels of these RNA forms (Fig. 1A). In all patients but one tested, the expression level of these transcripts was increased in relapse versus remission. To determine whether the expression of these transcripts was preferentially restricted to PBMC subset, we purified CD4 and non-CD4 T cell fractions by negative immunomagnetic selection from PBMCs of patients who were in relapse. The RT-PCR analyses of six transcripts (cl1, cl2, cl4, cl9, cl10, and cl11) were performed on these cell populations and revealed that the highest level of these cDNA was observed in the CD4+ T cell subset. As an example, the expression of cl2 and 9 are shown in Figure 1B. These results suggest that MCNS relapse is associated with generation of abnormal RNA expression that preferentially occurs in CD4+ T cells.
Selective induction of unknown transcripts in patients with MCNS relapse. (A) Semiquantitative RT-PCR analyses of 16 transcripts (cl1–cl16). PCR reactions were performed using primers specific for each cDNA clone as listed in Table 1. Quantification of PCR products was determined using the Image Quant V 1.11 analysis software. Values for each transcript are given as a bar graph after normalization against the amount of corresponding glyceraldehyde-3-phosphate dehydrogenase (GAPDH) cDNA. (B) Expression of cl10 and cl11 in CD4+ and non-CD4+ (nCD4) subsets purified from PBMC as described in “Methods.” The expression of GAPDH was monitored in parallel.
The alignment of these cDNA sequences with sequences available in Genbank revealed that all of these transcripts either matched with intronic regions or were spanning an intron within different genes. These genes are involved in various functions, including cell-cycle regulation and differentiation, cytoskeletal organization, transcription factors, and regulation of proteasome activity and cytokines (Table 2). To assess whether the presence of these modified transcripts leads to the production of altered protein in MCNS, we next analyzed by Western blot the expression patterns of the proteins encoded by the KIAA1694, ubiquitin-specific protease 16, actin-related protein type 2, and Runx1 genes that gave rise to cl1, cl2, cl3, and cl4 and detected an additional truncated form of the protein exclusively in MCNS patients (data not shown).
Abnormal RNA expression was associated with down-regulation of SR proteins in MCNS relapse. The modification of several transcripts in MCNS led us to investigate the expression of SR proteins. Pre-mRNA splicing takes place in the nucleus and involves SR proteins, a group of presently known nine proteins that contain domains rich in arginine and serine residues (RS domains). SR proteins are essential for constitutive and alternative splicing and have also been implicated in steps downstream of pre-mRNA splicing, including mRNA nuclear-cytoplasmic transport. We analyzed expression of SR proteins in normal resting and activated T cells as well as in 10 nonactivated T cell samples from MCNS patients, using the MAb 104, which recognizes primarily phosphorylated RS domains. We detected two major bands, each consisting of a doublet, corresponding to SRp75 and SRp40. Normal resting T cell expressed a low level of SR proteins. However, upon activation with anti-CD3/CD28 antibodies, the upper bands of the doublets, corresponding to phosphorylated forms, were increased, whereas the nonphosphorylated forms were barely detectable (Fig. 2A). That only SRp75 and SRp40 were detected after 36 h of stimulation is in accordance with previous studies showing that expression of other SR proteins occurs only after 72 h of stimulation. In all 10 patients who were in MCNS relapse, we were not able to detect any signal. Therefore, MCNS relapses were associated with down-regulation of SR proteins when compared with either activated or nonactivated normal T cells.
Down-regulation of SRp75 and SRp40 in patients with MCNS relapse. (A) Immunodetection of SR proteins in normal resting (n = 3) and activated (n = 4) T cells in 10 MCNS PBMCs, using the MAb 104 that recognizes the phosphorylated SR proteins. Four normal PBMC populations were stimulated for 36 h with both anti-CD3 and anti-CD28 antibodies. PBMCs from MCNS patients (n = 4 and n = 6) were not stimulated. (B) Expression level of SRp75 and SRp40 mRNA in normal (n = 5) and MCNS (n = 8) PBMCs by RT-PCR analyses as described in “Methods.”
To further elucidate whether the lack of expression of SRp40 and SRp75 proteins was due to a defect of gene transcription, we analyzed the expression of SRp75 and SRp40 mRNA levels in T cells of MCNS patients by semiquantitative RT-PCR (Fig. 2B). Expression of SRp75 and SRp40 transcripts in MCNS patients and normal subjects was similar. Taken together, these results suggest that alteration of splicing RNA in MCNS was associated with translational inhibition of SRp75 and SRp40 transcripts.
DISCUSSION
In the present study, we reported the preliminary identification and characterization of 16 transcripts with an altered expression in the T cells of MCNS patients. The specificity of the expression of all transcripts in MCNS patients was attested by the lack of their expression in normal subjects and especially in patients who exhibited a nephrotic syndrome of unrelated pathophysiology.
The role of RNA processing in human disease is actually highlighted. A large majority of diseases related to RNA processing results from the loss of function of a single gene as a result of mutations in cis-acting elements required for premessenger RNA splicing. Here, we observed that RNA processing anomalies concern several transcripts during MCNS relapse, suggesting a more general event in which the pre-mRNA splicing machinery is affected. Thus, alterations in the trans-acting factors required for RNA processing have recently been described, particularly in neurologic diseases such as myotonic dystrophy, spinal muscular atrophy, and amyotrophic lateral sclerosis and cancer (10).
In the present study, we showed that generation of alternative spliced forms is associated with a down-regulation of SRp75 and SRp40 proteins. These proteins are specifically required for cross-exon interactions in both constitutively and alternatively spliced pre-mRNA. Recently, it was shown that relative levels of several SR proteins change upon T cell activation, inducing change in the pattern of CD45 pre-mRNA splicing (11). As other SR proteins, SRp40 recognizes specific 5 to 7 nucleotide- degenerated consensus sequence named exonic splicing enhancers, and at least 29 SRp40-specific exonic splicing enhancers have already been described (12). The expression, level, phosphorylation, cellular location, and specific mix of SR/nRNP (small ribonucleoprotein particles) are believed to be the major component in the regulation of specific split site choices. This model presumes that SR protein patterns and mRNA alternative splicing are tissue specific, developmentally regulated, and responsive to the metabolic state of the cell. Here, we suggest for the first time that changes in the expression of SR proteins and mRNA-processing alteration could also be related to immune disease such as MCNS.
The links between lack of expression of SR proteins and “abnormal” RNA splicing remain to be determined. It is unlikely that SR proteins are not at all expressed during MCNS relapse, although their expression might be under our detection limits. These results are amazing because 1) an expansion of T cells expressing CD25 activation marker occurred during the MCNS relapse (13), and 2) T cell activation increases the level of expression of SR proteins (11). However, recent studies have revealed the regulatory and inhibitory functions of the CD4+ CD25+ T cells (14).
Such findings are in agreement with the fact that alterations in CD4 T cell–mediated immunity functions are commonly observed in MCNS. They lead to cutaneous hypersensitivity reactions or depression of recall responses to common antigens and might account for the susceptibility to pneumococcal and other pathogen agents during the course of the disease. These studies suggest the presence of a soluble factor inhibiting T cell activation and proliferation (15–17).
Here we demonstrate that abnormal mRNA splicing occurs mainly in CD4+ T cells from patients with MCNS. Whether the lack of expression of SR proteins in MCNS is related to the T cell anergic status remains an open question. Functional implications of the RNA processing anomalies during MCNS remain to be determined as well. We have previously demonstrated that alternative splicing of the KIAA1694 gene leads to a truncated protein named Tc-mip (truncated c-maf inducing protein) and is involved in the Th2 signaling pathway of CD4+ T cells (9). The significance of other mRNAs' alternative splicing forms in the context of pathogenesis of MCNS remain to be determined.
Patients with MCNS tend to have high IgM and low IgG levels. Similar to alteration in SR protein expression during MCNS, these abnormalities are reversible and considered a defect in Ig switching (18). The immunoglobulin RNA-processing regulation is still poorly understood. However, it was demonstrated recently that pre-mRNA processing during B cell development is highly sensitive to artificial change in the SR protein expression (19). Whether defect in Ig class switching during MCNS relapse is related to alteration in SR protein remains unresolved but constitutes an exiting challenge in the future.
Abbreviations
- MCNS:
-
minimal-change nephrotic syndrome
- PBMC:
-
peripheral blood mononuclear cell
- SR:
-
serin-rich
References
Maniatis T, Tasic B 2002 Alternative pre-mRNA splicing and proteome expansion in metazoans. Nature 418: 236–243
Mironov AA, Fickett JW, Gelfand MS 1999 Frequent alternative splicing of human genes. Genome Res 9: 1288–1293
Johnson JM, Castle J, Garrett-Engele P, Kan Z, Loerch PM, Armour CD, Santos R, Schadt EE, Stoughton R, Shoemaker DD 2003 Genome-wide survey of human alternative pre-mRNA splicing with exon junction microarrays. Science 302: 2141–2144
Caceres JF, Kornblihtt AR 2002 Alternative splicing: multiple control mechanisms and involvement in human disease. Trends Genet 18: 186–193
Niaudet P 1993 Nephrotic syndromes. [Physiopathology, diagnosis, clinical course and treatment of lipoid nephrosis]. Rev Prat 43: 637–639
Sahali D, Pawlak A, Le Gouvello S, Lang P, Valanciute A, Remy P, Loirat C, Niaudet P, Bensman A, Guellaen G 2001 Transcriptional and post-transcriptional alterations of IκBα in active minimal-change nephrotic syndrome. J Am Soc Nephrol 12: 1648–1658
Shalhoub RJ 1974 Pathogenesis of lipoid nephrosis: a disorder of T-cell function. Lancet 2: 556–560
Sahali D, Pawlak A, Valanciute A, Grimbert P, Lang P, Remy P, Bensman A, Guellaen G 2002 A novel approach to investigation of the pathogenesis of active minimal-change nephrotic syndrome using subtracted cDNA library screening. J Am Soc Nephrol 13: 1238–1247
Grimbert P, Valanciute A, Audard V, Pawlak A, Le Gouvelo S, Lang P, Niaudet P, Bensman A, Guellaen G, Sahali D 2003 Truncation of C-mip (Tc-mip), a new proximal signaling protein, induces c-maf Th2 transcription factor and cytoskeleton reorganization. J Exp Med 19: 797–807
Philips AV, Cooper TA 2000 RNA processing and human disease. Cell Mol Life Sci 57: 235–249
ten Dam GB, Zilch CF, Wallace D, Wieringa B, Beverley PC, Poels LG, Screaton GR 2000 Regulation of alternative splicing of CD45 by antagonistic effects of SR protein splicing factors. J Immunol 164: 5287–5295
Shin C, Manley JL 2002 The SR protein SRp38 represses splicing in M phase cells. Cell 111: 407–417
Neuhaus TJ, Shah V, Callard RE, Barratt TM 1995 T-lymphocyte activation in steroid-sensitive nephrotic syndrome in childhood. Nephrol Dial Transplant 10: 348–352
Shevach EM 2001 Certified professionals: CD4(+)CD25(+) suppressor T cells. J Exp Med 193: F41–F46
Fodor P, Saitua MT, Rodriguez E, Gonzalez B, Schlesinger L 1982 T-cell dysfunction in minimal-change nephrotic syndrome of childhood. Am J Dis Child 136: 713–717
Schnaper HW, Aune TM 1987 Steroid-sensitive mechanism of soluble immune response suppressor production in steroid-responsive nephrotic syndrome. J Clin Invest 79: 257–264
Schnaper HW 1990 A regulatory system for soluble immune response suppressor production in steroid-responsive nephrotic syndrome. Kidney Int 38: 151–159
Lin CY, Chen CH, Lee PP 1989 In vitro B-lymphocyte switch disturbance from IgM into IgG in IgM mesangial nephropathy. Pediatr Nephrol 3: 254–258
Bruce SR, Dingle RW, Peterson ML 2003 B-cell and plasma-cell splicing differences: a potential role in regulated immunoglobulin RNA processing. RNA 9: 1264–1273
Acknowledgements
We are indebted to Drs. P Remy, V. Baudouin, P. Niaudet, and M. Broyer for providing blood samples and clinical information as well as for support and advice.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported in part by the Association pour l'Utilisation du Rein Artificiel (AURA, Paris) and an apex grant from the INSERM.V.A. and A.V. contributed equally to this work.
Rights and permissions
About this article
Cite this article
Grimbert, P., Audard, V., Valanciute, A. et al. Abnormal RNA Processing and Altered Expression of Serin-Rich Proteins in Minimal-Change Nephrotic Syndrome. Pediatr Res 57, 133–137 (2005). https://doi.org/10.1203/01.PDR.0000148013.53429.5B
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000148013.53429.5B
This article is cited by
-
Physiopathology of idiopathic nephrotic syndrome: lessons from glucocorticoids and epigenetic perspectives
Pediatric Nephrology (2012)
-
Rituximab therapy for steroid-dependent minimal change nephrotic syndrome
Pediatric Nephrology (2006)