Abstract
Numerous disease-causing gene mutations have been identified in proteinuric diseases, such as nephrotic syndrome and glomerulosclerosis. This report describes the results of comprehensive genetic diagnosis of Japanese patients with severe proteinuria. In addition, the report describes the clinical characteristics of patients with monogenic disease-causing mutations. We conducted comprehensive gene screening of patients who had either congenital nephrotic syndrome, infantile nephrotic syndrome, steroid-resistant nephrotic syndrome, or focal segmental glomerular sclerosis. Using targeted next-generation sequencing, 60 podocyte-related genes were screened in 230 unrelated patients with proteinuria. A retrospective review of clinical data was conducted for these patients. We detected monogenic disease-causing mutations in 30% (69 of 230) of patients among 19 of the screened genes. Common genes with disease-causing mutations were WT1 (25%), NPHS1 (12%), INF2 (12%), TRPC6 (10%), and LAMB2 (9%). With various immunosuppressive or renoprotective therapies, remission of proteinuria in patients with unknown causative mutations was observed in 26% of patients, whereas only 5% of patients with monogenic disease-causing mutations exhibited complete remission. We assessed the genetic backgrounds of Japanese patients with severe proteinuria. The proportion of patients with gene defects was similar to that of other reports, but the disease-causing gene mutation frequency was considerably different.
Similar content being viewed by others
Introduction
Idiopathic nephrotic syndrome has an estimated incidence of approximately 2 to 6.5 per 100,000 children per year, depending on ethnic background1,2. Steroid-resistant nephrotic syndrome (SRNS) occurs in approximately 10%–20% of children with nephrotic syndrome, and is associated with an increased risk of complications due to persistent proteinuria and therapeutic drug side effects. Most patients with SRNS initially exhibit the histological pattern of focal segmental glomerulosclerosis (FSGS), which is the primary glomerular aetiology of end-stage renal disease (ESRD) in children3,4. Congenital nephrotic syndrome (CNS), which develops at 0–3 months of age, and infantile nephrotic syndrome (INS), which develops at 4–12 months of age, are most commonly associated with gene mutations that encode the structural and regulatory proteins of the glomerular filtration barrier5.
Whole-exome NGS sequencing has revealed new disease-causing gene mutations associated with SRNS. Recently, more than 50 podocyte-related gene mutations have been identified in monogenic forms of CNS/INS/SRNS/FSGS6,7. Genetic aetiologies were identified in 29.5% of patients with SRNS before 25 years of age in a Western population8 and in 28.3% of such patients in Chinese cohort9. The proportion of patients in whom disease-causing gene mutations could be detected decreased with increasing age at the onset of nephrotic syndrome in previous studies10,11. A genetic diagnosis may enable clinicians to begin early management and treatment, such as the discontinuation of immunosuppressant therapy due to its strong side effects, and the initiation of renoprotective drugs. In addition, disease-causing mutations in some genes encoding enzymes of the coenzyme Q10 (CoQ10) pathway can be treated by supplementation with CoQ1012,13. Finally, mutation detection analyses can facilitate the prediction of post-transplant recurrence of nephrotic syndrome7,14.
Studies of Western and Chinese cohorts of paediatric SRNS patients showed that the results of genetic analyses vary among ethnicities8,9. Following the advent of NGS, the discovery of proteinuric disease-causing gene mutations in patients has grown rapidly, although the exact incidence remains unclear. Until now, there have been no large-scale mutation screening studies of Japanese patients with nephrotic syndrome.
In this study, we used targeted NGS for simultaneous sequencing of 60 podocyte-related genes and aimed to clarify the clinical characteristics of Japanese patients with one of the following diseases: CNS, INS, SRNS, FSGS, or asymptomatic proteinuria with likely genetic disease.
Results
Mutations
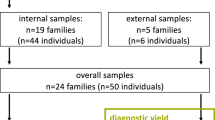
We collected samples from facilities throughout Japan (Supplementary Fig. S1). A total of 230 unrelated patients (132 men/boys and 98 women/girls) were included. Their median age at disease onset was 3 years (range, 1 day to 65 years). Of these 230 patients, 10 were diagnosed with CNS, 14 were diagnosed with INS, 101 were diagnosed with SRNS, and 105 were diagnosed with FSGS or asymptomatic proteinuria. We detected disease-causing gene mutations in 69 of 230 unrelated patients (30%). The coverage depths of detected genes are shown in Supplementary Table S1. One of the 69 patients was from a consanguineous family, whereas 15 patients had a positive family history of proteinuria, and 15 patients had a positive family history of renal failure (Table 1). In the 25 patients harbouring autosomal recessive disease-causing mutations, four homozygous and 21 compound heterozygous mutations were found (Table 2).
We detected the disease-causing gene mutation in 85% of patients with CNS, 53% of patients with INS, 26% of patients with onset age of 1–3 years, 17% of patients with onset age of 4–6 years, 31% of patients with onset age of 7–12 years, 20% of patients with onset age of 13–18 years, and 20% of patients with onset age of 19 years or older (Supplementary Fig. S2). WT1 gene variants were most common, detected in 17 patients; variants in NPHS1 and INF2 were detected in eight patients, variants in TRPC6 were detected in seven patients, and variants in LAMB2 were detected in six patients (Table 3).
Genes with disease-causing mutations within the first 1 year of life were as follows: 37% of mutations in WT1, 26% of mutations in NPHS1, 26% of mutations in LAMB2, and 11% of mutations in other genes. WT1 was also the most frequent gene mutated in individuals with onset of SRNS after the age of 1 year. In 27 (12%) patients, one or several extra-renal abnormalities were reported; these included symptoms suggestive of Denys-Drash syndrome (caused by WT1 gene mutation and characterised by nephropathy, Wilms tumour, and genital abnormalities) and Pierson syndrome (caused by LAMB2 gene mutation and characterised by the occurrence of congenital nephrotic syndrome and ocular anomalies in combination with microcoria).
Renal prognosis
Seven patients had progressed to chronic kidney disease (CKD) stage 5 by the time of genetic analysis. The estimated glomerular filtration rate was above 90 ml/min/1.73 m2 in 108 of 173 evaluable patients (62%); it was 60 to 89 ml/min/1.73 m2 in 36 patients (21%), 30 to 59 ml/min/1.73 m2 in 18 patients (10%), and below 30 ml/min/1.73 m2 in 11 patients (6%) (Table 4). Kaplan–Meier analysis of renal survival showed that patients with genetic proteinuria exhibited faster progression to CKD stage 4 (p < 0.0221; Supplementary Fig. 3). The most common histopathologic diagnosis was FSGS (62%), followed by minor glomerular abnormalities (28%), mesangioproliferative GN (4%), and diffuse mesangial sclerosis (2%) (Table 5).
Clinical characteristics
When patients were stratified on the basis of causative mutation detection, patients with mutations in the analysed genes had higher frequencies of family history (p = 0.0004) and younger age (p = 0.024) than patients without mutations in the analysed genes. Patients with mutations had lower frequencies of nephrotic syndrome (p = 0.0421), oedema (p = 0.0018), and remission (p = 0.0104) than patients without mutations (Table 6).
Six parameters (age, sex, family history, oedema, remission, and nephrotic syndrome) were entered in multivariate logistic regression analysis. Patients with mutations had a significantly higher frequency of family history than patients without mutations (OR = 8.85; 95% CI = 2.96–26.48; p < 0.0001). Patients with mutations were approximately six-fold more likely to show absence of oedema (OR = 6.67; 95% CI = 2.03–21.84; p = 0.0017) and absence of remission (OR = 4.67; 95% CI = 1.39–15.69; p = 0.0128), relative to patients without mutations. Patients with mutations had higher odds of younger age than patients without mutations (OR = 0.89; 95% CI = 0.82–0.95; p < 0.0001) (Table 7).
Discussion
In this study, we found that 30% (69 of 230) of the patients had a single gene defect in one of 60 currently known podocyte-related genes in the Japanese population. In a previous study8, genetic diagnoses were established in 526 patients from 183 families (detection rate of 29.5%); four genes were identified as major SRNS genes: NPHS2 (9.93%), NPHS1 (7.34%), WT1 (4.77%), and PLCE1 (2.17%). The highest rate of mutation detection (69.4%) was recorded in the youngest group of patients (0–3 months); this proportion decreased with age. In the PodoNet study15, genetic disease was identified in 23.6% of patients; the most common mutated genes were NPHS2, WT1, and NPHS1. In that report, the proportion of patients with gene mutations also decreased with age; it was 66% in patients with CNS, whereas it decreased to 15–16% in older children. In the PodoNet study, the distribution of causative genes in patients with CNS was as follows: 40% had mutations in NPHS1, 10.6% had mutations in NPHS2, 8.5% had mutations in WT1, 5.5% had mutations in LAMB2, and 4.7% had mutations in all other genes (combined). In the present study, genetic diagnoses were established in 69 of 230 unrelated patients (30%); the mutation detection rate was similar. Furthermore, common genes were WT1 (25%), NPHS1 (12%), INF2 (12%), TRPC6 (10%), and LAMB2 (9%). In the present study, the distribution of causative genes in patients with CNS was as follows: 36% had mutations in NPHS1, 36% had mutations in LAMB2, and 18% had mutations in WT1. No NPHS2 mutations were detected in our study, which was consistent with the results of a study of Korean children with SRNS (patients with CNS were excluded from that study)16. In China, the most common mutated genes were ADCK4 (6.67%), NPHS1 (5.83%), WT1 (5.83%), and NPHS2 (3.33%)9. The results of these studies show that there are differences in the types and frequencies of mutations among ethnicities and regions.
The Child Welfare Law, passed in 1961 in Japan, mandated urinary screening for preschool children, typically at 3 years of age. The purpose of urinary screening for preschool children was to prevent progression to ESRD or to improve the quality of life of children who were expected to develop ESRD. This first urinalysis is performed by using dip-and-reagent strips. In our study, we detected the disease-causing gene mutation in 41% of patients at the age of 3 years; this high detection rate was likely because of the mandatory urine screening for preschool children, which helped to detect the presence of proteinuria and could increase the likelihood that genetic analyses were conducted in affected children.
The treatment of SRNS is a challenging task for nephrologists because of its poor response to immunosuppressive drugs. High-dose steroids, cyclophosphamide, calcineurin inhibitors, mycophenolate mofetil, and rituximab have been used with variable success rates in children. However, complete remission of non-genetic SRNS was observed in 78% of patients during calcineurin inhibitor therapy17. In contrast, genetic SRNS was associated with a high rate of ESRD development: one patient with genetic SRNS experienced complete remission and 16% of patients with genetic SRNS experienced partial remission after calcineurin inhibitor therapy17. In our study, complete remission of SRNS without mutations was observed in 26% of patients during immunosuppressive therapy. However, this proportion does not reflect the natural clinical course of SRNS because most patients with SRNS who do not have mutations will be treated with immunosuppressants, such as repeated steroid pulses or rituximab treatment after genetic analyses, and there is insufficient long-term follow-up data for these types of patients. Complete remission of nephrotic syndrome in patients with mutations was observed in 5% (2/37) of patients during treatment with immunosuppressive therapies and in one patient during treatment with angiotensin-converting enzyme inhibitors. Notably, angiotensin-converting enzyme inhibitors and angiotensin receptor blockers may cause urinary protein reduction and have renoprotective effects. However, a previous study showed that more patients reached ESRD when using calcineurin inhibitors; the investigators concluded that calcineurin inhibitors may cause proteinuria reduction, but may negatively influence kidney function17. Most patients with nephrotic syndrome who have mutations do not respond to immunosuppressive therapy; however, patients with disease-causing mutations in PLCE118 and TRPC619 at least partially respond to therapy. Thus far, there are insufficient data to determine whether this proteinuria reduction has a renoprotective effect, and further studies of extended cohorts are needed.
The identification of gene mutations is important for decision-making in terms of future treatment strategies and predicting prognosis. However, it is not yet feasible to perform genetic testing in all patients with proteinuria. Therefore, it is necessary to consider which patients should undergo genetic testing. In previous reports of patients with SRNS, the likelihood of identifying a genetic mutation was inversely related to age at disease onset and was increased in patients with positive family history and in those with extra-renal manifestations7. In our study, we compared patients with and without known causative mutations, among all patients. The results showed that risk factors of genetic disease were younger age, family history, absence of oedema, and absence of remission. Importantly, absence of remission was strongly associated with genetic disease in this study. In a previous report of adult-onset FSGS, secondary FSGS (i.e., resistance to immunosuppression and atypical primary FSGS) was considered for genetic evaluation20; our results concur with those of the prior report.
This study had several limitations. First, this was a cross-sectional retrospective study with a small study population, which limits the generalisability of the findings. Second, the examinations of individual patients relied entirely on the attending clinicians’ decisions, due to the retrospective nature of the study. Finally, treatment details were not accessible for some patients, which limited our ability to make inferences regarding their disease characteristics.
In conclusion, we found pathogenic disease-causing gene mutations in Japanese patients with severe proteinuria. Detection of these mutations in podocyte-related genes will be helpful in treatment and prediction of renal outcome.
Methods
Patients
This study protocol was approved by the Institutional Review Board of Kobe University Graduate School of Medicine (IRB approval number 301). Informed consent was obtained from the patients or their family members in this study. The patients were recruited between January 2016 and December 2018. Inclusion in the study was based on fulfilment of one of the following criteria: (i) diagnosis of CNS, which presents within the first 3 months of life; (ii) diagnosis of INS, which presents between 3–12 months of age; (iii) diagnosis of SRNS, which is defined by persistent proteinuria after 4 weeks of daily treatment with 60 mg/m2 prednisone; (iv) diagnosis of FSGS or asymptomatic proteinuria. Asymptomatic proteinuria was defined as the absence of who extra-renal symptoms or the presence of proteinuria and microhaematuria. (Supplementary Table S2). Details regarding family history and other clinical features were obtained from the referring clinician or the patient’s hospital records. eGFR was calculated for ages 3 month to 18 years using the creatinine based eGFR formula in Japanese child21,22. For the patients aged <3 month, eGFR was calculated using the original Schwartz formula23 as follows: k × body length (cm)/serum Cr level (mg/dL). For this study, the k values was set as 0.45.
Genetic analysis
As we previously reported24, genomic DNA was isolated from peripheral blood leukocytes from patients and their family members using the Quick Gene Mini 80 system (Wako Pure Chemical Industries, Ltd., Tokyo, Japan), in accordance with the manufacturer’s instructions. Targeted sequencing using NGS was conducted for genes that are associated with inherited glomerular diseases (Supplementary Table S3). NGS samples were prepared using a HaloPlex target enrichment system kit (Agilent Technologies, Santa Clara, CA, USA), in accordance with the manufacturer’s instructions. All indexed DNA samples were amplified by polymerase chain reaction and sequenced using the MiSeq platform (Illumina, San Diego, CA, USA). Resulting sequence data were analysed (from alignment to categorisation of mutations) using SureCall software (version 4.0, Agilent Technologies). As we previously reported24, pair analysis by SureCall was used to determine copy number changes in experimental samples relative to a reference sample without a copy number change. We conducted an additional custom array comparative genomic hybridisation when the identified exons (more than two exons) in a single patient exhibited deletions that were all consistent with the clinical presentation of the patient.
Custom array comparative genomic hybridisation
As we previously reported25, we conducted custom array comparative genomic hybridisation for one patient. We selected the COQ6 gene and constructed probes for it and the regions surrounding it. We used a custom HD-comparative genomic hybridisation microarray, 8 × 15 K (Agilent Technologies), in accordance with the manufacturer’s instructions. We used Agilent CytoGenomics software (Agilent Technologies) to analyse chromosomal patterns within the microarray profiles.
Confirmation of the pathogenicity
Candidate variants were considered disease-causing mutations when they met at least one of the following criteria: (1) previous identification as a disease-causing mutation in a published paper; (2) predicted truncation (i.e., nonsense, obligatory splice site, or frameshift mutations); (3) for all novel missense variants, in silico testing with MutationTaster (http://mutationtaster.org/), PolyPhen-2 (http://genetics.bwh.havard.edu/pph/), or SIFT (http://sift.jcvi.org/) indicated pathogenicity. In addition to these three criteria, we confirmed the absence of contradictions between familial segregation and symptoms.
Statistical analysis
Results are presented as median and interquartile range (IQR). The chi-squared test or Fisher’s exact test was used to compare variables between two groups. The Mann-Whitney U test was used to compare median differences between two experimental groups. Multivariate logistic regression analysis was performed to calculate odds ratios (ORs) and 95% confidence intervals (95% CIs) after controlling for potential confounders. Statistical analysis was performed using standard statistical software (JMP version 10 for Windows; SAS Institute, Cary, NC, USA). In all tests, p < 0.05 was considered statistically significant.
Data availability
The data are not available for public access because of patient privacy concerns, but are available from the corresponding author on reasonable request.
References
McKinney, P. A., Feltbower, R. G., Brocklebank, J. T. & Fitzpatrick, M. M. Time trends and ethnic patterns of childhood nephrotic syndrome in Yorkshire, UK. Pediatric nephrology 16, 1040–1044, https://doi.org/10.1007/s004670100021 (2001).
Kikunaga, K. et al. High incidence of idiopathic nephrotic syndrome in East Asian children: a nationwide survey in Japan (JP-SHINE study). Clinical and experimental nephrology 21, 651–657, https://doi.org/10.1007/s10157-016-1319-z (2017).
Mekahli, D. et al. Long-term outcome of idiopathic steroid-resistant nephrotic syndrome: a multicenter study. Pediatric nephrology 24, 1525–1532, https://doi.org/10.1007/s00467-009-1138-5 (2009).
Zagury, A. et al. Steroid-resistant idiopathic nephrotic syndrome in children: long-term follow-up and risk factors for end-stage renal disease. Jornal brasileiro de nefrologia: ‘orgao oficial de Sociedades Brasileira e Latino-Americana de Nefrologia 35, 191–199, https://doi.org/10.5935/0101-2800.20130031 (2013).
Cil, O. et al. Genetic abnormalities and prognosis in patients with congenital and infantile nephrotic syndrome. Pediatric nephrology 30, 1279–1287, https://doi.org/10.1007/s00467-015-3058-x (2015).
Bierzynska, A. et al. Genomic and clinical profiling of a national nephrotic syndrome cohort advocates a precision medicine approach to disease management. Kidney international 91, 937–947, https://doi.org/10.1016/j.kint.2016.10.013 (2017).
Preston, R., Stuart, H. M. & Lennon, R. Genetic testing in steroid-resistant nephrotic syndrome: why, who, when and how? Pediatric nephrology, https://doi.org/10.1007/s00467-017-3838-6 (2017).
Sadowski, C. E. et al. A single-gene cause in 29.5% of cases of steroid-resistant nephrotic syndrome. Journal of the American Society of Nephrology: JASN 26, 1279–1289, https://doi.org/10.1681/ASN.2014050489 (2015).
Wang, F. et al. Spectrum of mutations in Chinese children with steroid-resistant nephrotic syndrome. Pediatric nephrology 32, 1181–1192, https://doi.org/10.1007/s00467-017-3590-y (2017).
Santin, S. et al. Clinical utility of genetic testing in children and adults with steroid-resistant nephrotic syndrome. Clinical journal of the American Society of Nephrology: CJASN 6, 1139–1148, https://doi.org/10.2215/CJN.05260610 (2011).
Bullich, G. et al. Targeted next-generation sequencing in steroid-resistant nephrotic syndrome: mutations in multiple glomerular genes may influence disease severity. Eur J Hum Genet 23, 1192–1199, https://doi.org/10.1038/ejhg.2014.252 (2015).
Cao, Q. et al. Coenzyme Q(10) treatment for one child with COQ6 gene mutation induced nephrotic syndrome and literature review. Zhonghua er ke za zhi. Chinese journal of pediatrics 55, 135–138, https://doi.org/10.3760/cma.j.issn.0578-1310.2017.02.016 (2017).
Desbats, M. A., Lunardi, G., Doimo, M., Trevisson, E. & Salviati, L. Genetic bases and clinical manifestations of coenzyme Q10 (CoQ 10) deficiency. J Inherit Metab Dis 38, 145–156, https://doi.org/10.1007/s10545-014-9749-9 (2015).
Weber, S. & Tonshoff, B. Recurrence of focal-segmental glomerulosclerosis in children after renal transplantation: clinical and genetic aspects. Transplantation 80, S128–134, https://doi.org/10.1097/01.tp.0000187110.25512.82 (2005).
Trautmann, A. et al. Spectrum of steroid-resistant and congenital nephrotic syndrome in children: the PodoNet registry cohort. Clinical journal of the American Society of Nephrology: CJASN 10, 592–600, https://doi.org/10.2215/CJN.06260614 (2015).
Cho, H. Y. et al. WT1 and NPHS2 mutations in Korean children with steroid-resistant nephrotic syndrome. Pediatric nephrology 23, 63–70, https://doi.org/10.1007/s00467-007-0620-1 (2008).
Buscher, A. K. et al. Rapid Response to Cyclosporin A and Favorable Renal Outcome in Nongenetic Versus Genetic Steroid-Resistant Nephrotic Syndrome. Clinical journal of the American Society of Nephrology: CJASN 11, 245–253, https://doi.org/10.2215/CJN.07370715 (2016).
Lin, T. et al. A Chinese girl with novel PLCE1 mutations and proliferation of the mesangium responded to tacrolimus therapy. Nephrology 19, 173, https://doi.org/10.1111/nep.12178 (2014).
Schlondorff, J., Del Camino, D., Carrasquillo, R., Lacey, V. & Pollak, M. R. TRPC6 mutations associated with focal segmental glomerulosclerosis cause constitutive activation of NFAT-dependent transcription. Am J Physiol Cell Physiol 296, C558–569, https://doi.org/10.1152/ajpcell.00077.2008 (2009).
Lepori, N., Zand, L., Sethi, S., Fernandez-Juarez, G. & Fervenza, F. C. Clinical and pathological phenotype of genetic causes of focal segmental glomerulosclerosis in adults. Clinical kidney journal 11, 179–190, https://doi.org/10.1093/ckj/sfx143 (2018).
Uemura, O. et al. Creatinine-based equation to estimate the glomerular filtration rate in Japanese children and adolescents with chronic kidney disease. Clinical and experimental nephrology 18, 626–633, https://doi.org/10.1007/s10157-013-0856-y (2014).
Uemura, O., Ishikura, K., Gotoh, Y. & Honda, M. Creatinine-based estimated glomerular filtration rate for children younger than 2 years. Clinical and experimental nephrology 22, 483–484, https://doi.org/10.1007/s10157-017-1460-3 (2018).
Schwartz, G. J., Brion, L. P. & Spitzer, A. The use of plasma creatinine concentration for estimating glomerular filtration rate in infants, children, and adolescents. Pediatr Clin North Am 34, 571–590, https://doi.org/10.1016/s0031-3955(16)36251-4 (1987).
Nagano, C. et al. Detection of copy number variations by pair analysis using next-generation sequencing data in inherited kidney diseases. Clinical and experimental nephrology 22, 881–888, https://doi.org/10.1007/s10157-018-1534-x (2018).
Nakanishi, K. et al. Pair analysis and custom array CGH can detect a small copy number variation in COQ6 gene. Clinical and experimental nephrology 23, 669–675, https://doi.org/10.1007/s10157-018-1682-z (2019).
Acknowledgements
We thank all study participants and their families. Our sincere thanks to all participating doctors for providing samples. In particular, we are extremely grateful to Dr. Akira Ashida, Dr. Yasuhiro Inaba, and Dr. Koichi Kamei for the collection of blood samples and clinical information. We thank Ryan Chastain-Gross, Ph.D., from Edanz Group (https://en-author-services.edanzgroup.com) for editing a draft of this manuscript. This study was supported by a Grant-in-Aid for Scientific Research (KAKENHI) from the Ministry of Education, Culture, Sports, Science and Technology of Japan (Subject ID: 18K15713 to China Nagano, 17H04189 to Kazumoto Iijima, and 19K08726 to Kandai Nozu).
Author information
Authors and Affiliations
Contributions
C.N. designed the study and wrote the initial draft of the manuscript. Ka.N. contributed to the analysis and interpretation of data, and assisted in the preparation of the manuscript. T.Y., T.H., Y.A., S.I. and N.S. interpreted the data. Y.S., K.O.N., H.N. and K.I. critically reviewed the manuscript. All authors approved the final version of the manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nagano, C., Yamamura, T., Horinouchi, T. et al. Comprehensive genetic diagnosis of Japanese patients with severe proteinuria. Sci Rep 10, 270 (2020). https://doi.org/10.1038/s41598-019-57149-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-57149-5
This article is cited by
-
Hidden genetics behind glomerular scars: an opportunity to understand the heterogeneity of focal segmental glomerulosclerosis?
Pediatric Nephrology (2024)
-
WT1 exon 10 missense variant in a pediatric patient with focal segmental glomerulosclerosis with embryonal hyperplasia
Pediatric Nephrology (2024)
-
Rituximab in combination with cyclosporine and steroid pulse therapy for childhood-onset multidrug-resistant nephrotic syndrome: a multicenter single-arm clinical trial (JSKDC11 trial)
Clinical and Experimental Nephrology (2024)
-
Characterization of cytoskeletal and structural effects of INF2 variants causing glomerulopathy and neuropathy
Scientific Reports (2023)
-
Precise clinicopathologic findings for application of genetic testing in pediatric kidney transplant recipients with focal segmental glomerulosclerosis/steroid-resistant nephrotic syndrome
Pediatric Nephrology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.