Abstract
Endothelium-derived nitric oxide (EDNO) plays a pivotal role in regulating pulmonary circulation. To determine whether there is a heterogeneity in EDNO-mediated responses of different sized pulmonary vessels, we studied small and large isolated pulmonary arteries of newborn lambs (diameter, 0.4-0.7 and 1.5-2.5 mm, respectively). The isometric tension of vessel rings were recorded while suspended in organ chambers filled with modified Krebs-Ringer bicarbonate solution (95% O2-5% CO2, 37°C). In vessels preconstricted with norepinephrine, acetylcholine and bradykinin induced a greater relaxation of small pulmonary arteries than of large pulmonary arteries. Acetylcholine, bradykinin, and nitric oxide also induced a greater increase in cGMP content in small arteries than in large ones. The responses to acetylcholine and bradykinin were endothelium-dependent and inhibited by nitro-L-arginine, an inhibitor of nitric oxide synthase. In vessels without endothelium, the response to nitric oxide was inhibited by 1H-[1,2,4]oxadiazolo[4,3-a]quinoxalin-1-one, an inhibitor of soluble guanylate cyclase. The activity of soluble guanylyl cyclase of small arteries was greater than that of large arteries under basal conditions and after stimulation with S-nitroso-N-acetylpenicillamine, a nitric oxide donor. These results demonstrate that heterogeneity exists in EDNO-mediated relaxation of small and large pulmonary arteries in newborn lambs. A difference in the soluble guanylate cyclase activity of vascular smooth muscle may have contributed to this phenomenon.
Similar content being viewed by others
Main
The perinatal pulmonary circulation is modulated by EDNO (1–8). Inhibiting the synthesis of EDNO causes pulmonary hypertension (9), attenuates pulmonary vasodilation induced by acetylcholine, bradykinin, ATP, increase in oxygen tension, and ventilation (1,4–6,10,11). These studies indicate a pivotal role for EDNO in modulating the response of perinatal pulmonary vasoactivity (1–13). So far most studies on EDNO-mediated response of isolated pulmonary arteries have been conducted on conduit vessels (2,6–8). There are few studies on ENDO-mediated response of small resistance pulmonary arteries (14). It is not clear whether there is a heterogeneity in EDNO-mediated response of different sized isolated pulmonary vessels.
In the present study we have determined the response of small and large pulmonary arteries of newborn lambs to endothelium-dependent vasodilators and exogenous nitric oxide. Because EDNO and nitric oxide causes vasodilation primarily by activating soluble guanylate cyclase and increasing the intracellular cGMP content (12,13,15), we have also measured the intracellular cGMP content and the activity of soluble guanylate cyclase of these vessels under basal conditions and after stimulation.
METHODS
Lungs of 35 newborn lambs (6-13 d old, either sex, Nebeker Ranch, Lancaster, CA) were used. The lambs were anesthetized with ketamine hydrochloride (30 mg/kg, i.m.) and killed with an overdose of pentobarbital (100 mg/kg, i.v.) (8).
Fourth and sixth generation pulmonary arteries were dissected from the lungs and cut into rings. The generations of pulmonary arteries were defined according to the Weibel and Taylor (16) method, designating the main branch of pulmonary arteries as the first generation. The outside diameters of fourth and sixth generation pulmonary arteries (from here on referred to as large and small pulmonary arteries, respectively) were 1.5-2.5 and 0.4-0.7 mm, respectively.
In some vessels, the endothelium was mechanically removed. The endothelium of large arterial rings was removed by inserting the tips of a watchmaker's forceps into the lumen of the vessel and rolling it back and forth on saline-loaded filter paper. The endothelium of small arterial rings was removed by inserting a stainless steel wire of 120 µm diameter into the lumen of the vessel and rolling it gently back and forth on saline-loaded filter paper. The surface of the stainless steel wire was made coarse with sandpaper. For all vessels, the removal of the endothelium was confirmed by lack of relaxation to acetylcholine (3 × 10-5 M).
Vessel tension study. Rings of pulmonary arteries were suspended in organ chambers filled with 10 mL of modified Krebs-Ringer bicarbonate solution [composition (in mM): NaCl, 118.3; KCl, 4.7; CaCl2, 2.5; MgSO4, 1.2; KH2PO4, 1.2; NaHCO3, 25.0; glucose, 11.1] maintained at 37 ± 0.5°C and aerated with 95% O2-5% CO2 (pH 7.4). Each ring was suspended by two stirrups passed through the lumen. One stirrup was anchored to the bottom of the organ chamber; the other was connected to a strain gauge (model FT03C, Grass Instrument, Quincy, MA) for the measurement of isometric force (7,8). The stirrups used for large arteries were made from stainless steel wires with a 120-µm diameter. The stirrups used for small arteries were made from stainless steel wires with a 200-µm diameter and tungsten wires with a 50-µm diameter. The stainless steel wire was used to keep the shape of the stirrups, and the tungsten wire was passed through the lumen of the vessel to hold the vessel. The transducer sensitivity for the measurement of the isometric tension was set at 0.1 g for large arteries and 0.05 g for small arteries.
At the beginning of the experiment, each vessel ring was brought to its own optimal tension by stretching the tissue progressively by 0.1-0.2-g increments until the contractile response to 100 mM KCl was maximal. One hour of equilibration was allowed before the effects of variable vasoactive agents were examined.
Experimental protocols for vessel tension study. At basal conditions. NLA (10-4 M; an inhibitor of nitric oxide synthase) (17) or control solvent was administrated to small and large pulmonary arteries with and without endothelium to examine the effect of NLA on the tension.
In vessels preconstricted to norepinephrine. Pulmonary arteries were first constricted to similar tensions with norepinephrine (3 × 10-7 M to 3 × 10-5 M). Contraction to norepinephrine was obtained in the presence of hydrocortisone (3 × 10-5 M), cocaine (5 × 10-6 M), and propranolol (5 × 10-6 M) to block neurol uptake, extraneuronal uptake, and β-adrenoceptors, respectively (18–20). These drugs were administered 45 min before norepinephrine and remained in contact with the tissue throughout the experiment.
After the contraction became stable, cumulative concentration-response curves to acetylcholine (10-8 to 10-4 M) and bradykinin (10-10 to 10-6 M) were obtained in arteries with and without endothelium, and in arteries with endothelium treated with NLA (10-4 M). Cumulative concentration-response curves to nitric oxide (1.6 × 10-9 M to 5 × 10-7 M) were obtained in arteries without endothelium under control condition or treated with ODQ (10-5 M, a selective inhibitor of soluble guanylate cyclase) (21,22).
To eliminate the possible involvement of endogenous cyclo-oxygenase products (23), all vessel tension studies were performed in the presence of an cyclooxygenase inhibitor (indomethacin, 10-5 M). Preliminary studies showed that indomethacin at 10-5 did not have a significant effect on the contraction of pulmonary arteries induced by norepinephrine or endothelium-dependent relaxation induced by acetylcholine (data not shown).
RIA of the intracellular content of cGMP. Vessel rings of small and large pulmonary arteries were incubated in 10 mL of modified Krebs-Ringer bicarbonate solution (37°C, 95% O2 and 5% CO2) containing indomethacin (10-5 M) and isobutylmethylxanthine (10-4 M). These inhibitors were used to prevent the involvement of cyclooxygenase products and to prevent the degradation of cGMP by phosphodiesterases (23,24).
After 45 min of equilibration, acetylcholine (3 × 10-6 M or 3 × 10-5 M) and bradykinin (10-6 M) were administered to arteries with and without endothelium and arteries with endothelium pretreated with NLA (10-4 M). Nitric oxide (1.6 × 10-7 M to 5 × 10-7 M) was administrated to arteries without endothelium in the presence and absence of ODQ (10-5 M). After 3 min of administration of acetylcholine or bradykinin and after 1 min of administration of nitric oxide, vessel rings were freeze-clamped rapidly and thawed in trichloroacetic acid (6%). Preliminary study showed that the maximal accumulation of cGMP in newborn ovine pulmonary arteries occurred at 3 min in response to acetylcholine and bradykinin and at 1 min in response to nitric oxide. The vessel rings were then homogenized in glass with a motor-driven Teflon pestle, sonicated for 5 s, and centrifuged at 13 000 × g for 15 min. The supernatant was extracted with four volumes of water-saturated diethyl ether and lyophilized; the pellets were weighed. The lyophilized samples were resuspended in 0.5 mL of sodium acetate buffer (0.05 M, pH 6.2) and their content of cGMP was determined using a cGMP kit (Biomedical Technologies Inc., Stoughton, MA). The content of cGMP is expressed as picomoles/mg of protein. The protein concentrations of the vessels were determined by the Bradford (25) method using BSA as the standard.
Soluble guanylate cyclase activity assay. The assay method used for soluble guanylate cyclase activity was similar to that described by Domino et al. (26). Pulmonary arteries without the endothelium were homogenized in Tris/HCl buffer (50 mM, pH 7.6) containing DTT (1 mM), EDTA (1 mM), and phenymethylsulfonyl fluoride (1 mM). The homogenates were centrifuged at 100 000 × g for 1 h at 4°C. The supernatant was collected and kept at -70°C until use for assay. The protein concentrations of the supernatant were determined using the Bradford (25) method with BSA as the standard.
The reaction was started by adding 50 µL of supernatant (containing 20 µg of protein) to 100 µL of incubation buffer (30°C). The reaction mixture contained Tris/HCl (50 mM, pH 7.6), DTT (1 mM), GTP (1 mM), MgCl2 (4 mM), creatine phosphate (23.6 mM), creatine phosphokinase (40.8 µg/150 µλ; 190 U/mg), BSA (0.1 mg/mL), and isobutylmethylxanthine (1 mM). The effect of nitric oxide on the soluble guanylate cyclase activity was determined by the administration of SNAP (10-5 M; a nitric oxide donor) (27). In comparison with that of authentic nitric oxide solution, the administration of SNAP into the small volume of the reaction mixture is technically more feasible. The concentration of SNAP used was based on its effectiveness in the induction of relaxation of pulmonary arteries of newborn lambs as determined in the preliminary organ chamber study. In some experiments, the effect of the inhibitor of the soluble guanylate cyclase activity was determined by using ODQ (10-5 M).
After 10 min of incubation, the assay tubes were placed in a boiling water bath for 5 min and the aliquots of the supernatant were taken to determine the amount of cGMP formed using a RIA kit (Biomedical Technologies Inc., Stoughton, MA). Guanylate cyclase activity is expressed as pmol of cGMP min-1 mg of protein-1. Preliminary experiments confirmed the linearity of guanylate cyclase activity at the protein concentration used within the incubation times.
Preparation of nitric oxide. A gas bulb sealed with a silicone rubber injection septum was filled with nitric oxide from a cylinder (Union Carbide, Chicago, IL). An appropriate volume (0.025, 0.25, and 2.5 mL) was removed with a syringe and injected into another gas bulb filled with 250 mL of distilled water, which had been gassed with helium for over 3 h, giving stock solutions of nitric oxide of 4.2 × 10-6 M, 4.2 × 10-5 M, and 4.2 × 10-4 M (7,8).
Determination of CSASM. First, CSAT was obtained using a formula similar to that of Jiang et al. (28): CSAT = wet weight of vessel (mg) ÷ density of vessel (mg/mm3) ÷ optimal length of the vessel (mm). The vessel density was obtained by dividing the blotted wet weight of the vessel from its volume. The volume was determined by measuring the volume of Krebs-Ringer bicarbonate solution displaced by the vessel rings after the tissues were placed in a 1-mL graduated cylinder with an accuracy of 0.01 mL. The optimal length was determined, with the aid of a magnifying eyepiece and a micrometer with an accuracy of 0.01 mm, by measuring the distance between two stirrups passed through the lumen of the vessel ring under the optimal resting tension of the vessel.
After the CSAT was obtained, the ratio of the cross section are occupied by smooth muscle to the total cross section area of the vessel (CSASM/CSAT) was obtained by counting the total area and the area occupied by smooth muscle cells on histologic transverse section of the pulmonary arteries (5-µm thickness) under a microscope. The histologic sections were treated with either hematoxylin and eosin stain or Van Giesson stain to discriminate between smooth muscle cells and other components. The CSASM/CSAT ratios obtained from hematoxylin and eosin stains and obtained from Van Giesson stain were averaged. The mean values were multiplied by the CSAT to obtained the smooth muscle cross section area of the vessel.
Drugs. The following drugs were used (unless otherwise specified, all were obtained from Sigma Chemical Co., St. Louis, MO): acetylcholine chloride, bradykinin, L(-)-norepinephrine bitartrate (Research Biochemicals International, Natick, MA), cocaine hydrochloride, hydrocortisone 21-sodium hemisuccinate, indomethacin, isobutylmethylxanthine, ODQ (Biomol Research Laboratories, Inc., Plymouth, PA), NLA (Research Biochemicals International), DL-propranolol, and SNAP (Research Biochemicals International).
Isobutylmethylxanthine was dissolved in ethanol (final concentration in organ chamber, 0.1%). ODQ was dissolved in DMSO (final concentration in organ chamber, 0.1%). Preliminary studies indicated that ethanol and DMSO at concentrations used did not significantly affect the contraction of the vessels to norepinephrine or the endothelium-dependent relaxation of the vessels to acetylcholine (data not shown). Indomethacin (10-5 M) was prepared in equal molar Na2CO3. This concentration of Na2CO3 did not significantly affect the pH of the solution in the organ chamber. The other drugs were prepared using distilled water. All inhibitors and antagonists were added at least 30 min before testing their effects.
Data analyses. The basal tension and contraction are expressed as grams/mm2 CSASM. Relaxation is expressed as percent of contraction. Data are shown as means ± SEM. When mean values of two groups were compared, a t test for unpaired observations was used. When the mean values of the same group before and after stimulation were compared, a t test for paired observations was used. Comparison of mean values of more than two groups was made with a one-way ANOVA test with a Student-Newman-Keuls test for post hoc testing of multiple comparison. All these analyses were performed using a commercially available statistics package (SigmaStat, Jandel Scientific, San Rafael, CA). Statistical significance was accepted when the p value (two-tailed) was less than 0.05. In all experiments, n represents the number of animals studied.
RESULTS
Morphologic data. The weights and optimal length of vessel rings used in the study were significantly different between large and small arteries. The densities and the cross section areas of these vessels were not significantly different. There is no significant difference in tissue cross section area between large and small arteries. However, the ratio of cross section area occupied by smooth muscle to the total cross section area is greater in small arteries than those of large arteries. For all these morphologic values, there was no significant difference between arteries with endothelium and arteries those without endothelium (Table 1).
Vessel tension studies. The optimal resting tension for small arteries with and without endothelium was 1.13 ± 0.09 and 1.25 ± 0.11 g/mm2 CSASM respectively (n = 19 for each group). The optimal resting tension was 0.66 ± 0.05 and 0.68 ± 0.06 g/mm2 CSASM for large arteries with and without endothelium, respectively (n = 19 for each group). The resting tensions of small arteries were greater than those of large arteries. There is no significant difference in the resting tensions between vessels with and without endothelium (p < 0.05).
Under basal conditions, NLA (10-4 M, an inhibitor of nitric oxide synthase) (17), had no effect on the basal tension of large arteries with and without endothelium (n = 6 for each group). NLA (10-4 M) also had no effect on the basal tension of small arteries without endothelium but caused an increase in the tension of small arteries with endothelium by 0.53 ± 0.6 g/mm2 CSASM (n = 6, p < 0.05).
The effects of acetylcholine, bradykinin, and nitric oxide were examined in arteries preconstricted with norepinephrine (3 × 10-7 M to 3 × 10-5 M) to a similar tension (Table 2). In some experiments, the effect of nitric oxide was also tested in small and large arteries without endothelium after the vessel tensions were raised by norepinephrine (3 × 10-7 M for large arteries and 3 × 10-5 M for small arteries) to comparable levels (Table 2).
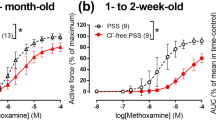
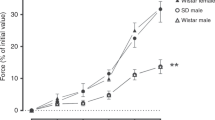
During contraction to norepinephrine, acetylcholine and bradykinin induced a concentration-dependent relaxation of arteries with endothelium. In arteries with endothelium treated with NLA (10-4 M; Figs. 1 and 2) and in vessels without endothelium (data not shown, n = 4 to 5 for each group), acetylcholine and bradykinin had no significant effect. The endothelium-dependent relaxation of small arteries was significantly greater than that of large arteries (Figs. 1 and 2). In pulmonary arteries without endothelium, nitric oxide induced a greater relaxation of small vessels than of large vessels (Fig 3). Relaxation to nitric oxide was abolished by ODQ, a specific inhibitor of soluble guanylate cyclase (21,22) (10-5 M; Fig. 3).
Responses of small and large pulmonary arteries to acetylcholine. Active tension in arteries was raised to a similar level by norepinephrine (3 × 10-7 M to 3 × 10-5 M). Changes in tension induced by acetylcholine are expressed as percent of contraction. PA, pulmonary arteries. Control, arteries with endothelium. NLA, arteries with endothelium-treated NLA (10-4 M). n = 6 for each group. *Significant difference between control large PA and those treated with NLA; †significant difference between control small and large PA (p < 0.05).
Responses of small and large pulmonary arteries to bradykinin. Active tension in arteries was raised to a similar level by norepinephrine (3 × 10-7 M to 3 × 10-5 M). Changes in tension induced by bradykinin are expressed as percent of contraction. PA, pulmonary arteries. Control, arteries with endothelium. NLA, arteries with endothelium treated NLA (10-4 M). n = 6 for each group. *Significant difference between control large PA and those treated with NLA; †significant difference between control small and large PA (p < 0.05).
Responses of small and large pulmonary arteries (without endothelium) to nitric oxide. Active tension in arteries was raised to a similar level by norepinephrine (3 × 10-7 M to 3 × 10-5 M). Changes in tension induced by nitric oxide are expressed as percent of contraction. PA, pulmonary arteries. Control, arteries without endothelium. ODQ, arteries without endothelium treated with ODQ (10-5 M). Data are shown as means ± SEM; n = 6 for each group. *Significant difference between control large PA and those treated with ODQ; †significant difference between control small and large PA (p < 0.05).
cGMP content. Under basal conditions, the intracellular content of cGMP of small pulmonary arteries with endothelium was greater than that of large arteries with endothelium. The basal cGMP contents of all arteries with endothelium were greater than those of arteries without endothelium or those of arteries with endothelium treated with NLA (10-4 M; Table 3).
Acetylcholine and bradykinin induced an endothelium-dependent increase in the intracellular content of cGMP of pulmonary vessels. The increase was greater in small arteries than in large ones. In the presence of NLA (10-4 M), the effects of acetylcholine and bradykinin on the cGMP content were eliminated (Figs. 4 and 5).
Effect of acetylcholine (3 × 10-6 M for small arteries and 3 × 10-5 M for large arteries, incubated for 3 min) on the intracellular content of cGMP of pulmonary arteries. PA, pulmonary arteries; NLA, 10-4 M. n = 6-9 for each group. *Significantly different from vessel with endothelium; †significantly different from small arteries (p < 0.05).
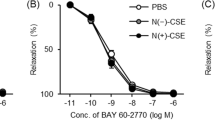
In vessels without endothelium, nitric oxide induced a significantly greater increase in the cGMP content in small arteries than in large arteries. In all vessels, the change in cGMP content induced by nitric oxide was abolished by ODQ (10-5 M; Fig 6).
Effect of nitric oxide (NO, incubated for 1 min) on the intracellular cGMP content of pulmonary arteries (without endothelium) in the presence and absence of ODQ (10-5 M). PA, pulmonary arteries. Data are shown as means ± SEM; n = 7 for each group. *Significantly different from small arteries; †significantly different from vessels stimulated with nitric oxide at 1.6 × 10-7 M; ‡significantly different from vessels not treated with ODQ (p < 0.05).
Soluble guanylate cyclase activity. The basal activity of the guanylate cyclase of the supernatant of small pulmonary arteries without endothelium (11.58 ± 1.9 pmol of GMP min-1 mg of protein-1, n = 6) was significantly greater than that of large arteries without endothelium (8.1 ± 0.9 pmol of cGMP min-1 mg of protein-1, n = 6; p < 0.05). In the presence of ODQ (10-5 M), the basal activity of the guanylate cyclase of the supernatant of small and large pulmonary arteries without endothelium was reduced to 1.37 ± 0.6 and 1.06 ± 0.41 pmol of cGMP min-1 mg of protein-1, respectively (n = 6 for each group). These values are significantly lower than those of the supernatant not treated with ODQ (p < 0.05).
SNAP (10-5 M, a nitric oxide donor) (27) caused a greater increase in guanylate cyclase activity in the supernatant of small arteries without endothelium than that of large arteries without endothelium. The effect of SNAP was inhibited by ODQ (10-5 M) (Fig. 7).
Guanylate cyclase activity of the 1 000 000 × g supernatant of large and small pulmonary arteries (PA) after stimulation with SNAP (10-5 M) in the presence and absence of ODQ (10-5 M). Data are shown as means ± SEM; n = 6 for each group. *Significantly different from small arteries; †significantly different from those not treated with ODQ (p < 0.05).
DISCUSSION
In perinatal pulmonary circulation, the endothelium inhibits the vascular tone by releasing a number of vasodilators including EDNO. EDNO is synthesized from L-arginine by nitric oxide synthase. It causes vasodilation by stimulating soluble guanylate cyclase and cGMP production in vascular smooth muscle cells (15). In the present study, NLA, an inhibitor of nitric oxide synthase (17), had no significant effect in large pulmonary arteries but caused an endothelium-dependent contraction in small arteries. Furthermore, the basal cGMP content of small arteries with endothelium was greater than that of intact large arteries. Such a difference was abolished by NLA. These results suggest that small pulmonary arteries are more actively regulated by basal EDNO than are large arteries in newborn lambs. The basal tension of small arteries appears to be modulated not only by vasodilators such as EDNO but also by some vasoconstrictors (12). This would explain the constriction unmasked after the inhibition of EDNO by NLA.
A variety of agonists including acetylcholine and bradykinin causes vasodilation by stimulating the release of nitric oxide from the endothelium (12,13). In our study, the relaxation and the increase in cGMP content of pulmonary arteries in response to acetylcholine and bradykinin were endothelium-dependent and inhibited by NLA, indicating that they were mediated by EDNO (15). The EDNO-mediated responses were more pronounced in small pulmonary arteries than in the large ones. The relaxation and the increase in cGMP content induced by exogenous nitric oxide were also greater in small arteries without endothelium than in large ones. These results demonstrate that small pulmonary arteries were more responsive to EDNO and nitric oxide than large arteries.
Although EDNO and nitric oxide may cause vasodilation by mechanisms such as the activation of potassium channels (30) and sodium-potassium pumps (31), studies so far suggest that the activation of soluble guanylate cyclase is the primary mechanism for vasodilation induced by EDNO and nitric oxide (12,15). In our study, nitric oxide-induced relaxation of pulmonary arteries was eliminated by ODQ, a highly selective inhibitor of soluble guanylate cyclase (21,22). Thus, it is likely that the relaxation of newborn ovine pulmonary arteries to nitric oxide is predominately via the soluble guanylate cyclase-cGMP pathway. Our biochemical study demonstrates that, both under basal conditions and after stimulation with SNAP (a nitric oxide donor) (27), the activity of soluble guanylate cyclase was greater in small arteries than in the large ones. Therefore, the greater activity of soluble guanylate cyclase in small arteries in comparison with large arteries may have contributed to the heterogeneity in EDNO-mediated relaxation of these different sized pulmonary vessels of newborn lambs. In an immunohistologic study, it was found that the staining for guanylate cyclase was denser in small than in large pulmonary arteries of fetal lambs (29).
EDNO plays a pivotal role in modulating the fetal and neonatal pulmonary circulation (1–13). In the present study, we showed that the role of EDNO was more pronounced in small than in large pulmonary arteries of newborn lambs. Our data provide direct evidence that a difference in the activity of soluble guanylate cyclase may have contributed to the heterogeneity in EDNO-dependent responses of different sized pulmonary arteries. In the pulmonary circulation, small arteries contribute significantly to the total pulmonary vascular resistance under both physiologic conditions and a variety of pathologic conditions (32). A greater role for EDNO in the modulation of the response of small arteries may be important in reducing pulmonary vascular resistance at birth and in maintaining normal pulmonary blood flow in the neonate.
Abbreviations
- EDNO:
-
endothelium-derived nitric oxide
- NLA:
-
NG-nitro-L-arginine
- SNAP:
-
S-nitroso-N-acetylpenicillamine
- ODQ:
-
1H-[1,2,4]oxadiazolo[4,3,-a]quinoxalin-1-one
- CSASM:
-
the smooth muscle cross section area
- CSAT:
-
the total cross section area of the vessel
References
Abman SH, Chatfield BA, Rodman DM, Hall SL, McMurtry IF 1991 Maturational changes in endothelium-derived relaxing factor activity of ovine pulmonary arteries in vitro. Am J Physiol 260: L280–L285
Zellers TM, Vanhoutte PM 1991 Endothelium-dependent relaxations of piglet pulmonary arteries augment with maturation. Pediatr Res 30: 176–180
Liu SF, Hislop AA, Haworth SG, Barnes PJ 1992 Developmental changes in endothelium-dependent pulmonary vasodilation in pigs. Br J Pharmacol 106: 324–338
Moore P, Velvis H, Fineman JR, Soifer SJ, Heymann MA 1992 EDRF inhibition attenuates the increase in pulmonary blood flow due to oxygen ventilation in fetal lambs. J Appl Physiol 73: 2151–2157
Shaul PW, Farrar MA, Magness RR 1993 Pulmonary endothelial nitric oxide production is developmentally regulated in the fetus and newborn. Am J Physiol 265: H1056–H1063
Steinhorn RH, Morin FC, Gugino SF, Giese EC, Russell JA 1993 Developmental differences in endothelium-dependent responses in isolated ovine pulmonary arteries and veins. Am J Physiol 264: H2162–H2167
Gao Y, Zhou H, Raj JU 1995 Heterogeneity in role of endothelium-derived NO in pulmonary arteries and veins of full-term fetal lambs. Am J Physiol 268: H1586–H1592
Gao Y, Zhou H, Raj JU 1995 Endothelium-derived nitric oxide plays a larger role in pulmonary veins than in arteries of newborn lambs. Circ Res 76: 559–565
Gordon JB, Tod ML 1993 Effects of Nω-nitro-L-arginine on total and segmental vascular resistance in developing lamb lungs. J Appl Physiol 75: 76–85
Fineman JR, Heymann MA, Soifer SJ 1991 Nω-Nitro-L-arginine attenuates endothelium-dependent pulmonary vasodilation in lambs. Am J Physiol 260: H1299–H1306
Cornfield DN, Chatfield BA, McQueston JA, McMurtry IF, Abman SH 1992 Effects of birth-related stimuli on L-arginine-dependent pulmonary vasodilation in ovine fetus. Am J Physiol 262: H1474–H1481
Barnes PJ, Liu SF 1995 Regulation of pulmonary vascular tone. Pharmacol Rev 47: 87–131
Fineman JR, Soifer SJ, Heymann MA 1995 Regulation of pulmonary vascular tone in the perinatal period. Annu Rev Physiol 57: 115–134
Wang Y, Coceani F 1994 EDRF in pulmonary resistance vessels from fetal lamb: stimulation by oxygen and bradykinin. Am J Physiol 266: H936–H943
Hobbs AJ, Ignarro LJ 1996 Nitric oxide-cyclic GMP signal transduction system. Methods Enzymol 269: 134–148
Weibel ER, Taylor CR 1988 Design and structure of the human lung. In: Fishman AP (ed) Pulmonary Diseases and Disorders, 2nd Ed. McGraw-Hill, New York, pp 11–33.
Mhlsch A, Busse R 1990 NG-Nitro-L-arginine(N5-[imino(nitroamino)methyl]-L-ornithine) impairs endothelium-dependent dilations by inhibiting cytosolic nitric oxide synthesis from L-arginine. Naunyn-Schmiedeberg's Arch Pharmacol 341: 143–147
Trendelenburg U 1980 A kinetic analysis of the extraneuronal uptake and metabolism of catecholamine. Rev Physiol Biochem Pharmacol 87: 33–115
Bhagat B, Bovell G, Robinson IM 1967 Influence of cocaine on the uptake of H3-norepinephrine and on the responses of isolated guinea-pig atria to sympathomimetic amine. J Pharmacol Exp Ther 155: 472–478
Gao Y, Tolsa J-F, Botello M, Raj JU 1998 Developmental change in isoproterenol-mediated relaxation of pulmonary veins of fetal and newborn lambs. J Appl Physiol 84: 1535–1539
Schrammel A, Behrends S, Schmidt K, Koesling D, Mayer B 1996 Characterization of 1H-[ 1,2,4]oxadiazolo[4,3-a]quinoxalin-1-one as a heme-site inhibitor of nitric oxide-sensitive guanylyl cyclase. Mol Pharmacol 50: 1–5
Garthwaite J, Southam E, Boulton CL, Nielsen EB, Schmidt K, Mayer B 1995 Potent and selective inhibition of nitric oxide-sensitive guanylyl cyclase by 1H-[ 1,2,4]oxadiazolo[4,3-a]quinoxalin-1-one. Mol Pharmacol 48: 184–188
Cassin S 1980 Role of prostaglandins and thromboxanes in the control of the pulmonary circulation in the fetus and newborn. Semin Perinatol 4: 101–107
Polson JB, Strada SJ 1996 Cyclic nucleotide phosphodiesterases and vascular smooth muscle. Annu Rev Pharmacol Toxicol 1996 36: 403–427
Bradford MM 1973 A rapid method for the quantitation of microgram quantities of protein utilizing the principle of protein dye binding. Anal Chem 72: 249–254
Domino SE, Tubb DJ, Garbers DL 1991 Assay of guanylate cyclase catalytic activity. Methods Enzymol 195: 345–355
Carrier GO, Fuchs LC, Winecoff AP, Giulumian AD, White RE 1997 Nitrovasodilators relax mesenteric microvessels by cGMP-induced stimulation of Ca-activated K channels. Am J Physiol 273: H76–H84
Jiang H, Halayko AJ, Rao K, Cunningham P, Stephens NL 1991 Normalization of force generated by canine airway smooth muscles. Am J Physiol 260: L522–L529
D'Angelis CA, Nickerson PA, Steinhorn RH, Morin FC 1998 Heterogeneous distribution of soluble guanylate cyclase in the pulmonary vasculature of the fetal lamb. Anat Rec 250: 62–69
Bolotina VM, Najibi S, Palacino JJ, Pagano PJ, Cohen RA 1994 Nitric oxide directly activates calcium-dependent potassium channels in vascular smooth muscle. Nature 368: 850–853
Gupta S, McArthur C, Grady C, Ruderman NB 1994 Stimulation of vascular N+-K+-ATPase activity by nitric oxide: a cGMP-independent effect. Am J Physiol 266: H2146–H2151
Raj JU, Chen P 1986 Microvascular pressures measured by micropuncture in isolated perfused lamb lungs. J Appl Physiol 61: 2194–2201
Acknowledgements
The authors thank Dr. Srinivas Dhanakoti for valuable advice, Jean Morris for technical assistance, and Mona Unutoa and Becky Saldana for secretarial assistance.
Author information
Authors and Affiliations
Additional information
Supported by National Institutes of Health, National Heart, Lung, and Blood Institute Grants HL-38438 and HL-47804 and by Le Center Hospitalier Universitaire Vaudois, Lausanne, Switzerland.
Rights and permissions
About this article
Cite this article
Gao, Y., Tolsa, JF. & Raj, J. Heterogeneity in Endothelium-Derived Nitric Oxide-Mediated Relaxation of Different Sized Pulmonary Arteries of Newborn Lambs. Pediatr Res 44, 723–729 (1998). https://doi.org/10.1203/00006450-199811000-00015
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199811000-00015