Key Points
-
Imaging high-risk prostate cancer is predominantly conducted using radionuclide bone scan, CT, and MRI
-
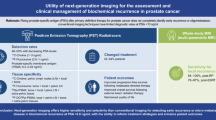
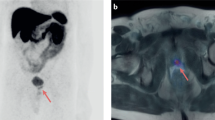
Multiparametric-MRI (mpMRI) and positron emission tomography (PET)–CT, using novel imaging techniques and radiopharmaceuticals, are currently being investigated and incorporated into clinical use
-
mpMRI and PET–CT are more advanced approaches than conventional techniques and offer improved sensitivity and specificity, enabling more accurate assessment of disease
-
Integrated PET–MRI could provide a comprehensive assessment of local disease extent, lymph nodes, and bones, as well as functional assessment of tumour aggressiveness and prognosis
-
Continued studies are warranted to further establish the role of new modalities in the management of patients with high-risk prostate cancer
Abstract
Approximately 15% of men with newly diagnosed prostate cancer have high-risk disease. Imaging is critically important for the diagnosis and staging of these patients, and also for the selection of management. While established prostate cancer staging guidelines have increased the appropriate use of imaging, underuse for high-risk prostate cancer remains substantial. Several factors affect the utility of initial diagnostic imaging, including the variable definition of high-risk prostate cancer, variable guideline recommendations, poor accuracy of existing imaging tests, and the difficulty in validating imaging findings. Conventional imaging modalities, including CT and radionuclide bone scan, have been employed for local and metastatic staging, but their performance characteristics have generally been poor. Emerging modalities including multiparametricMRI, positron emission tomography (PET)–CT, and PET–MRI have shown increased diagnostic accuracy and could improve accuracy in staging patients with high-risk prostate cancer.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2015. CA Cancer J. Clin. 65, 5–29 (2015).
Cooperberg, M. R., Broering, J. M. & Carroll, P. R. Time trends and local variation in primary treatment of localized prostate cancer. J. Clin. Oncol. 28, 1117–1123 (2010).
Bastian, P. J. et al. High-risk prostate cancer: from definition to contemporary management. Eur. Urol. 61, 1096–1106 (2012).
Brawley, O. W. Trends in prostate cancer in the United States. J. Natl Cancer Inst. Monogr. 2012, 152–156 (2012).
Miller, D. C., Hafez, K. S., Stewart, A., Montie, J. E. & Wei, J. T. Prostate carcinoma presentation, diagnosis, and staging: an update form the National Cancer Data Base. Cancer 98, 1169–1178 (2003).
Makarov, D. V. et al. Prostate cancer imaging trends after a nationwide effort to discourage inappropriate prostate cancer imaging. J. Natl Cancer Inst. 105, 1306–1313 (2013).
Makarov, D. V. et al. The population level prevalence and correlates of appropriate and inappropriate imaging to stage incident prostate cancer in the medicare population. J. Urol. 187, 97–102 (2012).
D'Amico, A. V. et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA 280, 969–974 (1998).
NCCN Guidelines Version 1.2015 Prostate Cancer Updates. nccn.org[online].
Roach, M. et al. Four prognostic groups predict long-term survival from prostate cancer following radiotherapy alone on Radiation Therapy Oncology Group clinical trials. Int. J. Radiat. Oncol. Biol. Phys. 47, 609–615 (2000).
Thompson, I. et al. Guideline for the management of clinically localized prostate cancer: 2007 update. J. Urol. 177, 2106–2131 (2007).
Heidenreich, A. et al. EAU guidelines on prostate cancer. Part 1: screening, diagnosis, and treatment of clinically localised disease. Eur. Urol. 59, 61–71 (2011).
Horwich, A., Parker, C., de Reijke, T., Kataja, V. & Group, E. G. W. Prostate cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 24 (Suppl. 6), vi106–114 (2013).
Eberhardt, S. C. et al. ACR Appropriateness Criteria prostate cancer—pretreatment detection, staging, and surveillance. J. Am. Coll. Radiol. 10, 83–92 (2013).
European Assoication of Urology Guidelines on prostate cancer. uroweb.org[online]
National Institute for Health and Care Excellence—Prostate cancer: diagnosis and treatment. nice.org.uk[online].
Cooperberg, M. R. et al. The University of California, San Francisco Cancer of the Prostate Risk Assessment score: a straightforward and reliable preoperative predictor of disease recurrence after radical prostatectomy. J. Urol. 173, 1938–1942 (2005).
Cooperberg, M. R., Broering, J. M. & Carroll, P. R. Risk assessment for prostate cancer metastasis and mortality at the time of diagnosis. J. Natl Cancer Inst. 101, 878–887 (2009).
Ravery, V. et al. Percentage of cancer on biopsy cores accurately predicts extracapsular extension and biochemical relapse after radical prostatectomy for T1-T2 prostate cancer. Eur. Urol. 37, 449–455 (2000).
O'Brien, M. F. et al. Pretreatment prostate-specific antigen (PSA) velocity and doubling time are associated with outcome but neither improves prediction of outcome beyond pretreatment PSA alone in patients treated with radical prostatectomy. J. Clin. Oncol. 27, 3591–3597 (2009).
Hattab, E. M., Koch, M. O., Eble, J. N., Lin, H. & Cheng, L. Tertiary Gleason pattern 5 is a powerful predictor of biochemical relapse in patients with Gleason score 7 prostatic adenocarcinoma. J. Urol. 175, 1695–1699 (2006).
NCCN Guidelines for patients: prostate cancer version III. nccn.org[online], (2002).
Prostate-specific antigen (PSA) best practice policy. American Urological Association (AUA). Oncology (Williston Park) 14, 267–272, 277–278, 280 passim (2000).
Abuzallouf, S., Dayes, I. & Lukka, H. Baseline staging of newly diagnosed prostate cancer: a summary of the literature. J. Urol. 171, 2122–2127 (2004).
Prostate cancer guideline for the management of clinically localized prostate cancer: 2007 update. aua.org[online].
Crawford, E. D. et al. Challenges and recommendations for early identification of metastatic disease in prostate cancer. Urology 83, 664–669 (2014).
Briganti, A. et al. When to perform bone scan in patients with newly diagnosed prostate cancer: external validation of the currently available guidelines and proposal of a novel risk stratification tool. Eur. Urol. 57, 551–558 (2010).
Schnipper, L. E. et al. American Society of Clinical Oncology identifies five key opportunities to improve care and reduce costs: the top five list for oncology. J. Clin. Oncol. 30, 1715–1724 (2012).
Makarov, D. H. et al. Regional variation and time trends in prostate cancer imaging utilization among veterans with incident disease. [abstract 1219] academyhealth.org[online], (2014).
Abraham, N., Wan, F., Montagnet, C., Wong, Y. N. & Armstrong, K. Decrease in racial disparities in the staging evaluation for prostate cancer after publication of staging guidelines. J. Urol. 178, 82–87 (2007).
Makarov, D. V. et al. Appropriate and inappropriate imaging rates for prostate cancer go hand in hand by region, as if set by thermostat. Health Aff. (Millwood) 31, 730–740 (2012).
Yu, K. K. et al. Detection of extracapsular extension of prostate carcinoma with endorectal and phased-array coil MR imaging: multivariate feature analysis. Radiology 202, 697–702 (1997).
Barentsz, J. O. et al. ESUR prostate MR guidelines 2012. Eur. Radiol. 22, 746–757 (2012).
Chong, Y. et al. Value of diffusion-weighted imaging at 3 T for prediction of extracapsular extension in patients with prostate cancer: a preliminary study. AJR Am. J. Roentgenol. 202, 772–777 (2014).
Futterer, J. J. et al. Staging prostate cancer with dynamic contrast-enhanced endorectal MR imaging prior to radical prostatectomy: experienced versus less experienced readers. Radiology 237, 541–549 (2005).
Augustin, H., Fritz, G. A., Ehammer, T., Auprich, M. & Pummer, K. Accuracy of 3-Tesla magnetic resonance imaging for the staging of prostate cancer in comparison to the Partin tables. Acta Radiol. 50, 562–569 (2009).
Futterer, J. J. et al. Prostate cancer: comparison of local staging accuracy of pelvic phased-array coil alone versus integrated endorectal-pelvic phased-array coils. Local staging accuracy of prostate cancer using endorectal coil MR imaging. Eur. Radiol. 17, 1055–1065 (2007).
Prostate imaging and reporting and data system: Version 2. acr.org[online].
Somford, D. M. et al. The predictive value of endorectal 3 Tesla multiparametric magnetic resonance imaging for extraprostatic extension in patients with low, intermediate and high risk prostate cancer. J. Urol. 190, 1728–1734 (2013).
Cornud, F. et al. Endorectal 3D T2-weighted 1 mm-slice thickness MRI for prostate cancer staging at 1.5Tesla: should we reconsider the indirects signs of extracapsular extension according to the D'Amico tumor risk criteria? Eur. J. Radiol. 81, e591–597 (2012).
Rosenkrantz, A. B. et al. Prostate cancer: utility of diffusion-weighted imaging as a marker of side-specific risk of extracapsular extension. J. Magn. Reson. Imaging 38, 312–319 (2013).
Lawrence, E. M. et al. Preoperative 3-T diffusion-weighted MRI for the qualitative and quantitative assessment of extracapsular extension in patients with intermediate- or high-risk prostate cancer. AJR Am. J. Roentgenol. 203, W280–286 (2014).
Ruprecht, O., Weisser, P., Bodelle, B., Ackermann, H. & Vogl, T. J. MRI of the prostate: interobserver agreement compared with histopathologic outcome after radical prostatectomy. Eur. J. Radiol. 81, 456–460 (2012).
Mullerad, M. et al. Prostate cancer: detection of extracapsular extension by genitourinary and general body radiologists at MR imaging. Radiology 232, 140–146 (2004).
Jager, G. J., Ruijter, E. T., de la Rosette, J. J. & van de Kaa, C. A. Amyloidosis of the seminal vesicles simulating tumor invasion of prostatic carcinoma on endorectal MR images. Eur. Radiol. 7, 552–554 (1997).
Soylu, F. N. et al. Seminal vesicle invasion in prostate cancer: evaluation by using multiparametric endorectal MR imaging. Radiology 267, 797–806 (2013).
McClure, T. D. et al. Use of MR imaging to determine preservation of the neurovascular bundles at robotic-assisted laparoscopic prostatectomy. Radiology 262, 874–883 (2012).
Park, B. H. et al. Influence of magnetic resonance imaging in the decision to preserve or resect neurovascular bundles at robotic assisted laparoscopic radical prostatectomy. J. Urol. 192, 82–88 (2014).
Schoder, H. & Larson, S. M. Positron emission tomography for prostate, bladder, and renal cancer. Semin. Nucl. Med. 34, 274–292 (2004).
Shreve, P. D. & Gross, M. D. Imaging of the pancreas and related diseases with PET carbon-11-acetate. J. Nucl. Med. 38, 1305–1310 (1997).
Apolo, A. B., Pandit-Taskar, N. & Morris, M. J. Novel tracers and their development for the imaging of metastatic prostate cancer. J. Nucl. Med. 49, 2031–2041 (2008).
Richter, J. A. et al. Dual tracer 11C-choline and FDG-PET in the diagnosis of biochemical prostate cancer relapse after radical treatment. Mol. Imaging Biol. 12, 210–7 (2010).
Umbehr, M. H., Muntener, M., Hany, T., Sulser, T. & Bachmann, L. M. The role of 11C-choline and 18F-fluorocholine positron emission tomography (PET) and PET/CT in prostate cancer: a systematic review and meta-analysis. Eur. Urol. 64, 106–117 (2013).
Jaeschke, R., Guyatt, G. H. & Sackett, D. L. Users' guides to the medical literature. III. How to use an article about a diagnostic test. B. What are the results and will they help me in caring for my patients? The Evidence-Based Medicine Working Group. JAMA 271, 703–707 (1994).
Picchio, M. et al. The role of choline positron emission tomography/computed tomography in the management of patients with prostate-specific antigen progression after radical treatment of prostate cancer. Eur. Urol. 59, 51–60 (2011).
Kjolhede, H. et al. Combined 18F-fluorocholine and 18F-fluoride positron emission tomography/computed tomography imaging for staging of high-risk prostate cancer. BJU Int. 110, 1501–1506 (2012).
Beheshti, M. et al. 18F choline PET/CT in the preoperative staging of prostate cancer in patients with intermediate or high risk of extracapsular disease: a prospective study of 130 patients. Radiology 254, 925–33 (2010).
Kabasakal, L. et al. Evaluation of PSMA PET/CT imaging using a 68Ga-HBED-CC ligand in patients with prostate cancer and the value of early pelvic imaging. Nucl. Med. Commun. 36, 582–587 (2015).
Eiber, M. et al. Evaluation of hybrid 68Ga-PSMA-ligand PET/CT in 248 patients with biochemical recurrence after radical prostatectomy. J. Nucl. Med. 56, 668–674 (2015).
Eiber, M. et al. Preliminary results for characterization of pelvic lymph nodes in patients with prostate cancer by diffusion-weighted MR-imaging. Invest. Radiol. 45, 15–23 (2010).
Thoeny, H. C. et al. Metastases in Normal-sized Pelvic Lymph Nodes: Detection with Diffusion-weighted MR Imaging. Radiology 273, 125–135 (2014).
Heck, M. M. et al. Prospective comparison of computed tomography, diffusion-weighted magnetic resonance imaging and [11C]choline positron emission tomography/computed tomography for preoperative lymph node staging in prostate cancer patients. Eur. J. Nucl. Med. Mol. Imaging 41, 694–701 (2014).
Kjolhede, H. et al. (18)F-fluorocholine PET/CT compared with extended pelvic lymph node dissection in high-risk prostate cancer. World J. Urol. 32, 965–970 (2014).
Poulsen, M. H. et al. [18F]fluoromethylcholine (FCH) positron emission tomography/computed tomography (PET/CT) for lymph node staging of prostate cancer: a prospective study of 210 patients. BJU Int. 110, 1666–1671 (2012).
Haseebuddin, M. et al. 11C-acetate PET/CT before radical prostatectomy: nodal staging and treatment failure prediction. J. Nucl. Med. 54, 699–706 (2013).
Davis, G. L. Sensitivity of frozen section examination of pelvic lymph nodes for metastatic prostate carcinoma. Cancer 76, 661–668 (1995).
Schuster, D. M. et al. Initial experience with the radiotracer anti-1-amino-3-18F-fluorocyclobutane-1-carboxylic acid with PET/CT in prostate carcinoma. J. Nucl. Med. 48, 56–63 (2007).
Chen, Y. et al. 2-(3-{1-Carboxy-5-[(6-[18F]fluoro-pyridine-3-carbonyl)-amino]-pentyl}-ureido)-pen tanedioic acid, [18F]DCFPyL, a PSMA-based PET imaging agent for prostate cancer. Clin. Cancer Res. 17, 7645–7653 (2011).
Even-Sapir, E. et al. The detection of bone metastases in patients with high-risk prostate cancer: 99mTc-MDP Planar bone scintigraphy, single- and multi-field-of-view SPECT, 18F-fluoride PET, and 18F-fluoride PET/CT. J. Nucl. Med. 47, 287–297 (2006).
D'Amico, A. V. et al. Prostate specific antigen doubling time as a surrogate end point for prostate cancer specific mortality following radical prostatectomy or radiation therapy. J. Urol. 172, S42–S47 (2004).
Leung, D., Krishnamoorthy, S., Schwartz, L. & Divgi, C. Imaging approaches with advanced prostate cancer: techniques and timing. Can. J. Urol. 21, 42–47 (2014).
Imbriaco, M. et al. A new parameter for measuring metastatic bone involvement by prostate cancer: the Bone Scan Index. Clin. Cancer Res. 4, 1765–1772 (1998).
Dennis, E. R. et al. Bone scan index: a quantitative treatment response biomarker for castration-resistant metastatic prostate cancer. J. Clin. Oncol. 30, 519–524 (2012).
Ulmert, D. et al. A novel automated platform for quantifying the extent of skeletal tumour involvement in prostate cancer patients using the Bone Scan Index. Eur. Urol. 62, 78–84 (2012).
Caldarella, C., Treglia, G., Giordano, A. & Giovanella, L. When to perform positron emission tomography/computed tomography or radionuclide bone scan in patients with recently diagnosed prostate cancer. Cancer Manag. Res. 5, 123–131 (2013).
Damle, N. A. et al. The role of 18F-fluoride PET-CT in the detection of bone metastases in patients with breast, lung and prostate carcinoma: a comparison with FDG PET/CT and 99mTc-MDP bone scan. Jpn J. Radiol. 31, 262–269 (2013).
Mari Aparici, C. & Seo, Y. Functional imaging for prostate cancer: therapeutic implications. Semin. Nucl. Med. 42, 328–342 (2012).
Langsteger, W. et al. Imaging of bone metastases in prostate cancer: an update. Q. J. Nucl. Med. Mol. Imaging 56, 447–458 (2012).
Perlmutter, M. A. & Lepor, H. Androgen deprivation therapy in the treatment of advanced prostate cancer. Rev. Urol. 9 (Suppl. 1), S3–S8 (2007).
Rakheja, R. et al. Fluorodeoxyglucose positron emission tomography/magnetic resonance imaging: current status, future aspects. PET Clin. 9, 237–252 (2014).
Cachovan, M., Vija, A. H., Hornegger, J. & Kuwert, T. Quantification of 99mTc-DPD concentration in the lumbar spine with SPECT/CT. EJNMMI Res. 3, 45 (2013).
Cook, G. J. & Fogelman, I. The role of positron emission tomography in skeletal disease. Semin. Nucl. Med. 31, 50–61 (2001).
Fogelman, I., Cook, G., Israel, O. & Van der Wall, H. Positron emission tomography and bone metastases. Semin. Nucl. Med. 35, 135–142 (2005).
Schiepers, C. et al. Fluoride kinetics of the axial skeleton measured in vivo with fluorine-18-fluoride PET. J. Nucl. Med. 38, 1970–1976 (1997).
Israel, O. et al. FDG-PET and CT patterns of bone metastases and their relationship to previously administered anti-cancer therapy. Eur. J. Nucl. Med. Mol. Imaging 33, 1280–1284 (2006).
Barrett, T. et al. DCE and DW MRI in monitoring response to androgen deprivation therapy in patients with prostate cancer: a feasibility study. Magn. Reson. Med. 67, 778–785 (2012).
Michoux, N. et al. Evaluation of DCE-MRI postprocessing techniques to assess metastatic bone marrow in patients with prostate cancer. Clin. Imaging 36, 308–315 (2012).
Luboldt, W. et al. Prostate carcinoma: diffusion-weighted imaging as potential alternative to conventional MR and 11C-choline PET/CT for detection of bone metastases. Radiology 249, 1017–25 (2008).
Nakanishi, K. et al. Whole-body MRI for detecting metastatic bone tumor: diagnostic value of diffusion-weighted images. Magn. Reson. Med. Sci. 6, 147–155 (2007).
Lecouvet, F. E. et al. Can whole-body magnetic resonance imaging with diffusion-weighted imaging replace Tc 99m bone scanning and computed tomography for single-step detection of metastases in patients with high-risk prostate cancer? Eur. Urol. 62, 68–75 (2012).
Lee, K. C. et al. A feasibility study evaluating the functional diffusion map as a predictive imaging biomarker for detection of treatment response in a patient with metastatic prostate cancer to the bone. Neoplasia 9, 1003–1011 (2007).
Reischauer, C. et al. Bone metastases from prostate cancer: assessing treatment response by using diffusion-weighted imaging and functional diffusion maps—initial observations. Radiology 257, 523–531 (2010).
Messiou, C. et al. Assessing response in bone metastases in prostate cancer with diffusion weighted MRI. Eur. Radiol. 21, 2169–2177 (2011).
Koh, D. M. & Collins, D. J. Diffusion-weighted MRI in the body: applications and challenges in oncology. AJR Am. J. Roentgenol. 188, 1622–1635 (2007).
Usuda, K. et al. Diffusion-weighted imaging is superior to positron emission tomography in the detection and nodal assessment of lung cancers. Ann. Thorac. Surg. 91, 1689–1695 (2011).
Choi, S. H. et al. Correlation of 18F-FDG uptake with apparent diffusion coefficient ratio measured on standard and high b value diffusion MRI in head and neck cancer. J. Nucl. Med. 52, 1056–62 (2011).
Nakajo, M. et al. FDG PET/CT and diffusion-weighted imaging for breast cancer: prognostic value of maximum standardized uptake values and apparent diffusion coefficient values of the primary lesion. Eur. J. Nucl. Med. Mol. Imaging 37, 2011–2020 (2010).
Wong, C. S. et al. Correlation of measurements from diffusion weighted MR imaging and FDG PET/CT in GIST patients: ADC versus SUV. Eur. J. Radiol. 81, 2122–2126 (2012).
Ho, K. C. et al. Correlation of apparent diffusion coefficients measured by 3T diffusion-weighted MRI and SUV from FDG PET/CT in primary cervical cancer. Eur. J. Nucl. Med. Mol. Imaging 36, 200–208 (2009).
Matsushima, N. et al. Relation between FDG uptake and apparent diffusion coefficients in glioma and malignant lymphoma. Ann. Nucl. Med. 26, 262–271 (2012).
Schoder, H. et al. 2-[18F]fluoro-2-deoxyglucose positron emission tomography for the detection of disease in patients with prostate-specific antigen relapse after radical prostatectomy. Clin. Cancer Res. 11, 4761–9 (2005).
Morris, M. J. et al. Fluorodeoxyglucose positron emission tomography as an outcome measure for castrate metastatic prostate cancer treated with antimicrotubule chemotherapy. Clin. Cancer Res. 11, 3210–3216 (2005).
Yeh, S. D. et al. Detection of bony metastases of androgen-independent prostate cancer by PET-FDG. Nucl. Med. Biol. 23, 693–697 (1996).
Salminen, E., Hogg, A., Binns, D., Frydenberg, M. & Hicks, R. Investigations with FDG-PET scanning in prostate cancer show limited value for clinical practice. Acta Oncol. 41, 425–429 (2002).
Tolvanen, T. et al. Biodistribution and radiation dosimetry of [(11)C]choline: a comparison between rat and human data. Eur. J. Nucl. Med. Mol. Imaging 37, 874–883 (2010).
Picchio, M. et al. [11C]Choline PET/CT detection of bone metastases in patients with PSA progression after primary treatment for prostate cancer: comparison with bone scintigraphy. Eur. J. Nucl. Med. Mol. Imaging 39, 13–26 (2012).
Bauman, G. et al. 18F-fluorocholine for prostate cancer imaging: a systematic review of the literature. Prostate Cancer Prostatic Dis. 15, 45–55 (2012).
Beheshti, M. et al. Detection of bone metastases in patients with prostate cancer by 18F fluorocholine and 18F fluoride PET-CT: a comparative study. Eur. J. Nucl. Med. Mol. Imaging 35, 1766–1774 (2008).
Pinaquy, J. B. et al. Comparative effectiveness of [18F]-fluorocholine PET-CT and pelvic MRI with diffusion-weighted imaging for staging in patients with high-risk prostate cancer. Prostate 75, 323–331 (2015).
FDA approves production of imaging agent that helps detect prostate cancer. fda.gov[online].
Oyama, N. et al. 11C-acetate PET imaging of prostate cancer. J. Nucl. Med. 43, 181–186 (2002).
Oyama, N. et al. 11C-acetate PET imaging of prostate cancer: detection of recurrent disease at PSA relapse. J. Nucl. Med. 44, 549–555 (2003).
Fricke, E. et al. Positron emission tomography with 11C-acetate and 18F-FDG in prostate cancer patients. Eur. J. Nucl. Med. Mol. Imaging 30, 607–611 (2003).
Yu, E. Y. et al. C11-acetate and F-18 FDG PET for men with prostate cancer bone metastases: relative findings and response to therapy. Clin. Nucl. Med. 36, 192–198 (2011).
Matthies, A. et al. Imaging of prostate cancer metastases with 18F-fluoroacetate using PET/CT. Eur. J. Nucl. Med. Mol. Imaging 31, 797 (2004).
Silver, D. A., Pellicer, I., Fair, W. R., Heston, W. D. & Cordon-Cardo, C. Prostate-specific membrane antigen expression in normal and malignant human tissues. Clin. Cancer Res. 3, 81–85 (1997).
O'Keefe, D. S. et al. Mapping, genomic organization and promoter analysis of the human prostate-specific membrane antigen gene. Biochim. Biophys. Acta 1443, 113–127 (1998).
Manyak, M. J. Indium-111 capromab pendetide in the management of recurrent prostate cancer. Expert Rev. Anticancer Ther. 8, 175–181 (2008).
Bander, N. H. Technology insight: monoclonal antibody imaging of prostate cancer. Nat. Clin. Pract. Urol. 3, 216–225 (2006).
Evans, M. J. et al. Noninvasive measurement of androgen receptor signaling with a positron-emitting radiopharmaceutical that targets prostate-specific membrane antigen. Proc. Natl Acad. Sci. USA 108, 9578–9582 (2011).
van de Watering, F. C. et al. Zirconium-89 labeled antibodies: a new tool for molecular imaging in cancer patients. Biomed. Res. Int. 2014, 203601 (2014).
Afshar-Oromieh, A. et al. The diagnostic value of PET/CT imaging with the Ga-labelled PSMA ligand HBED-CC in the diagnosis of recurrent prostate cancer. Eur. J. Nucl. Med. Mol. Imaging 42, 197–209 (2015).
Schmidt, G. P. et al. Screening for bone metastases: whole-body MRI using a 32-channel system versus dual-modality PET-CT. Eur. Radiol. 17, 939–949 (2007).
Mosavi, F. et al. Whole-body diffusion-weighted MRI compared with (18)F-NaF PET/CT for detection of bone metastases in patients with high-risk prostate carcinoma. AJR Am. J. Roentgenol. 199, 1114–1120 (2012).
Dietrich, O., Biffar, A., Reiser, M. F. & Baur-Melnyk, A. Diffusion-weighted imaging of bone marrow. Semin. Musculoskelet. Radiol. 13, 134–144 (2009).
Wetter, A. et al. Quantitative evaluation of bone metastases from prostate cancer with simultaneous [18F] choline PET/MRI: combined SUV and ADC analysis. Ann. Nucl. Med. 28, 405–410 (2014).
Woodrum, D. A. et al. Magnetic resonance imaging-guided cryoablation of recurrent prostate cancer after radical prostatectomy: initial single institution experience. Urology 82, 870–875 (2013).
Chang, C. H. et al. Detecting metastatic pelvic lymph nodes by 18F-2-deoxyglucose positron emission tomography in patients with prostate-specific antigen relapse after treatment for localized prostate cancer. Urol. Int. 70, 311–315 (2003).
Beheshti, M. et al. Impact of 18F-choline PET/CT in prostate cancer patients with biochemical recurrence: influence of androgen deprivation therapy and correlation with PSA kinetics. J. Nucl. Med. 54, 833–40 (2013).
Mullenders, L., Atkinson, M., Paretzke, H., Sabatier, L. & Bouffler, S. Assessing cancer risks of low-dose radiation. Nat. Rev. Cancer 9, 596–604 (2009).
Prasad, K. N., Cole, W. C. & Hasse, G. M. Health risks of low dose ionizing radiation in humans: a review. Exp. Biol. Med. (Maywood) 229, 378–382 (2004).
Lin, E. C. Radiation risk from medical imaging. Mayo Clin. Proc. 85, 1142–1146 (2010).
Huang, B., Law, M. W. & Khong, P. L. Whole-body PET/CT scanning: estimation of radiation dose and cancer risk. Radiology 251, 166–174 (2009).
Lam, D. L., Larson, D. B., Eisenberg, J. D., Forman, H. P. & Lee, C. I. Communicating Potential Radiation-Induced Cancer Risks From Medical Imaging Directly to Patients. AJR Am. J. Roentgenol. 21, 1–9 (2015).
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to discussion of article content, writing; reviewing, and editing the article before submission. M.A.B., A.B.R., L.S.B. and R.A.R. researched data for the article.
Corresponding author
Ethics declarations
Competing interests
S.S.T. has been a speaker for Eigen, a consultant for Hitachi-Aloka Medical and HealthTronics, and a sponsored trial investigator for Trod Medical. All other authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Bjurlin, M., Rosenkrantz, A., Beltran, L. et al. Imaging and evaluation of patients with high-risk prostate cancer. Nat Rev Urol 12, 617–628 (2015). https://doi.org/10.1038/nrurol.2015.242
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrurol.2015.242
This article is cited by
-
Patient-specific 3D printed and augmented reality kidney and prostate cancer models: impact on patient education
3D Printing in Medicine (2019)
-
Multiparametric whole-body 3.0-T MRI in newly diagnosed intermediate- and high-risk prostate cancer: diagnostic accuracy and interobserver agreement for nodal and metastatic staging
European Radiology (2019)
-
68Ga-PSMA-617 PET/CT: a promising new technique for predicting risk stratification and metastatic risk of prostate cancer patients
European Journal of Nuclear Medicine and Molecular Imaging (2018)
-
Molecular imaging of fibrosis using a novel collagen-binding peptide labelled with 99mTc on SPECT/CT
Amino Acids (2017)
-
Cytoreductive radical prostatectomy in metastatic prostate cancer: Does it really make sense?
World Journal of Urology (2017)