Abstract
Nicotine is the main psychoactive ingredient in tobacco and its rewarding effects are considered primarily responsible for persistent tobacco smoking and relapse. Although dopamine has been extensively implicated in the rewarding effects of nicotine, noradrenergic systems may have a larger role than previously suspected. This study evaluated the role of noradrenergic α1 receptors in nicotine and food self-administration and relapse, nicotine discrimination, and nicotine-induced dopamine release in the nucleus accumbens in rats. We found that the noradrenergic α1 receptor antagonist prazosin (0.25–1 mg/kg) dose dependently reduced the self-administration of nicotine (0.03 mg/kg), an effect that was maintained over consecutive daily sessions; but did not reduce food self-administration. Prazosin also decreased reinstatement of extinguished nicotine seeking induced by either a nicotine prime (0.15 mg/kg) or nicotine-associated cues, but not food-induced reinstatement of food-seeking, and decreased nicotine-induced (0.15 mg/kg) dopamine release in the nucleus accumbens shell. However, prazosin did not have nicotine-like discriminative effects and did not alter the dose-response curve for nicotine discrimination. These findings suggest that stimulation of noradrenergic α1 receptors is involved in nicotine self-administration and relapse, possibly via facilitation of nicotine-induced activation of the mesolimbic dopaminergic system. The findings point to α1 adrenoceptor blockade as a potential new approach to the treatment of tobacco dependence in humans.
Similar content being viewed by others
INTRODUCTION
Nicotine is the main psychoactive component of tobacco smoke and exerts its initial effect on neuronal nicotinic acetylcholine ion channel receptors (nAChRs). Like other addictive drugs, nicotine produces discriminative effects, facilitates intracranial self-stimulation and supports intravenous drug self-administration and the development of conditioned place preferences (CPP) in animals (Di Chiara, 2000; Le Foll and Goldberg, 2009; Stolerman et al., 1999). Nicotine shares with other addictive drugs the property of activating the mesolimbic dopamine (DA) brain reward system (for reviews, see Balfour (2002) and Di Chiara (2000)), an effect considered important for their rewarding addictive effects. However, other neurobiological systems are involved in drug reward and addiction, in particular brain noradrenergic systems.
Brain noradrenergic systems are comprised of two main ascending projections: the dorsal noradrenergic bundle, which originates in the locus coeruleus and projects to the hippocampus, cerebellum and forebrain; and the ventral noradrenergic bundle, which arises in a number of nuclei of the pons and medulla, and innervates the hypothalamus, midbrain and extended amygdala (for review, see (Moore and Bloom, 1979). There are three subclasses of adrenoceptors (α1, α2, and β), each with three known subtypes (α1A, α1B, α1D; α2A/D, α2B, α2C; β1, β2, β3), and all except β3 are expressed in the rat central nervous system (Nicholas et al., 1996).
Activation of brain noradrenergic pathways supports intracranial self-stimulation (ICSS) and modulates drug-induced changes in ICSS threshold. Compounds that interfere with noradrenaline (NA) synthesis or signalling influence a variety of behavioral effects of addictive drugs (for review, see Weinshenker and Schroeder (2007)). Noradrenergic α1 receptors seem to be particularly involved in these effects. Thus, prazosin, a prototype selective antagonist of noradrenergic α1 receptors, reduces rewarding effects of morphine in mice in the CPP paradigm (Zarrindast et al., 2002) and significantly attenuates the reinstatement of extinguished drug-seeking behavior in rats induced by a cocaine prime (Zhang and Kosten, 2005). Prazosin also reduces self-administration of cocaine and heroin in rats that have extended daily access to these drugs and reduces dependence-induced increases in responding for ethanol (Greenwell et al., 2009; Walker et al., 2008; Wee et al., 2008).
The noradrenergic system and its α1 receptors are also involved in the rewarding effects of nicotine. Systemically administered nicotine stimulates NA release in the cortex (Summers and Giacobini, 1995), hypothalamus (Sharp and Matta, 1993), hippocampus and amygdala (Fu et al., 1998), and increased NA levels in the amygdala and hypothalamus are correlated with increased nicotine self-administration by rats (Fu et al., 2001, 2003). In addition, prazosin reduces nicotine self administration in rats chronically receiving a monoamine oxidase inhibitor (Villegier et al., 2007) and blocks development of nicotine-induced CPP in rats (Forget et al., 2009b).
In this study, we investigated whether a selective noradrenergic α1 receptor antagonist (prasozin) would reduce the self-administration and discriminative effects of nicotine, two procedures used to assess drug abuse liability in animals (Carter and Griffiths, 2009). We also investigated the effect of noradrenergic α1 receptor blockade on reinstatement of extinguished nicotine-seeking behavior induced by nicotine priming or by nicotine-associated cues, on nicotine-induced release of DA in the nucleus accumbens shell, and on food self-administration and relapse as a control.
MATERIALS AND METHODS
Animals
Male Long Evans rats for the self-administration (Charles River, Lachine, PQ, Canada) and microdialysis (Charles River, Wilmington, MA, USA) studies were experimentally naive at the start of the study. They initially weighed 250–275 g for the self-administration study and 270–340 g for the microdialysis study. Rats were individually housed in a temperature- and humidity-controlled room on a 12-h reverse light–dark cycle (lights off from 0700 to 1900 h). Experiments were conducted during the dark phase. Before any experimental manipulation, animals were given a minimum of 7 days to habituate to the colony room, during which they were weighed and handled.
For the nicotine discrimination study, Male Sprague Dawley rats (Charles River) initially weighed 250–275 g. They were housed individually in a temperature- and humidity-controlled room on a regular 12-h light–dark cycle (lights on from 0700 to 1900 h). Experiments were conducted during the light phase.
For all experiments, water was available ad libitum and a diet restriction was maintained throughout the studies (∼20 g/day).
Drugs
(-)Nicotine hydrogen tartrate (Sigma-Aldrich, St Louis, MO., USA) was dissolved in saline, the pH was adjusted to 7.0 (±0.2), and the solution was filtered through a 0.22 mm syringe filter (Fisher Scientific, Pittsburgh, PA, USA) for sterilization purposes. All nicotine doses are reported as free base concentrations. Nicotine was administered intravenously in a volume of 100 μl/kg per injection or subcutaneously (s.c.) in a volume of 1 ml/kg.
Prazosin hydrochloride (Sigma-Aldrich) was sonicated in saline and administered intraperitoneally (i.p.) in a volume of 2 ml/kg body weight. The doses of prazosin (0.25–1 mg/kg), time of pretreatment and route of administration of prazosin were chosen based on previous studies (Forget et al., 2009b; Villegier et al., 2007).
Self-Administration Procedure
Initial behavioral conditioning techniques and surgical procedures were similar to those previously reported (Corrigall and Coen, 1989; Corrigall et al., 2001; Forget et al., 2009a) and are presented in the supplementary Materials and Methods.
For all self-administration studies, session duration was 60 min and the time-out (TO) period (house light turned off and cue light above the active lever turned on) following each injection or food pellet (45 mg precision pellets, BioServ) delivery was 1 min.
Testing Under the FR5 Schedule of Reinforcement
After the acquisition period and stabilization of the behavior (less than 20% variation in the number of injections earned per session during two consecutive sessions), one group of rats (group 1, n=14) was tested for the effects of prazosin (0.25–1 mg/kg, i.p., 30 min before the test session) on nicotine self-administration under the FR5 schedule of reinforcement, in comparison with the effects of substitution of nicotine by saline (saline substitution).
Another group of rats (group 2, n=11) was tested for the effects of prazosin (0.5 and 1 mg/kg, i.p., 30 min before the test session) on food self-administration under the same schedule of reinforcement.
A counterbalanced within-subject design was used (including saline substitution).
The test sessions were similar to the acquisition sessions under the FR5 schedule of reinforcement (supplementary Materials and Methods).
Nicotine- or Food-Induced Reinstatement
Another group of rats (group 3, n=10) was submitted to the same acquisition phase than group 1. After behavior stabilized under the FR5 schedule, seven additional daily sessions were conducted. This was followed by an extinction phase during which responses on the active or inactive lever were recorded, but had no consequences. The criterion for extinction was less than 20 active lever presses per 1-h session over two consecutive days.
After this extinction of nicotine-seeking behavior, the rats were tested for nicotine-induced reinstatement of nicotine seeking in a counterbalanced within-subject design, with or without the pharmacological treatment (nicotine prime+prazosin at 0 (vehicle), 0.25, 0.5, and 1 mg/kg; or prazosin alone (0.25–1 mg/kg)). Testing days were separated by at least three extinction sessions and stable extinction over two consecutive sessions was required before further testing. Nicotine priming consisted of a s.c. injection of 0.15 mg/kg nicotine, 10 min before the test-session (house light on during the whole session, no cues). Prazosin or its vehicle (saline) was injected i.p. 30 min before the nicotine prime.
After testing under FR5, the group 2 (n=11) has been submitted to extinction sessions and tested for food (two food pellets at the beginning of the session)-induced reinstatement of food seeking in a counterbalanced within-subject design, with or without prazosin pretreatment (0.5 and 1 mg/kg).
Cue-Induced Reinstatement of Nicotine Seeking
After rats from group 1 were tested for the effects of prazosin on nicotine self-administration (FR5), an additional five nicotine self-administration sessions were conducted without any treatment and the self-administration behavior was then extinguished, as described above (n=12, 2 rats were eliminated from the study because their behavior never extinguished). After stable extinction, these rats were tested for the effects of prazosin (0.25–1 mg/kg) on cue-induced reinstatement of nicotine-seeking behavior or on extinction behavior in a counterbalanced within-subject design. Reinstatement tests were conducted under conditions identical to those of self-administration sessions, except that 1) a single presentation of the cues (light above the active lever on and house-light off for 1 min) was delivered response-independently immediately at the start of the session and 2) responses on the active lever (on an FR5 schedule) resulted in contingent presentation of the cues) without nicotine availability (no injections). Responses on the inactive lever were recorded but had no programmed consequence. The testing sessions lasted 1 h.
Nicotine Discrimination Procedure
Rats (n=12) were trained under a FR schedule of food-pellet delivery to respond on one lever after an injection of a training dose of 0.4 mg/kg. of nicotine (s.c., 10 min before the session) and on the other lever after an injection of saline vehicle as previously described (Gasior et al., 1999). After the acquisition of the nicotine (0.4 mg/kg) discrimination (supplementary Materials and Methods), test sessions with other doses of nicotine or with prazosin were initiated. Test sessions were identical to training sessions, with the exception that both levers were correct and 10 consecutive responses on either one of the two levers resulted in the delivery of a food pellet. Test sessions were usually conducted twice a week on Tuesdays and Fridays. A range of doses of prazosin (0.25–1 mg/kg, 30 min before the session) were given alone to assess if prazosin pretreatment produced responding on the nicotine-associated lever (ie, a ‘nicotine like’ effect). Selected doses of prazosin (0, 0.25, 0.5, and 1 mg/kg) were then administered with various doses of nicotine (0.01, 0.03, 0.1, 0.3, and 0.4 mg/kg) to assess the effect of prazosin on the dose-response curve for nicotine discrimination. The percentage of responses on the nicotine-associated lever (ie, discrimination performance) and the response rate (in responses/sec) were measured.
In vivo Microdialysis
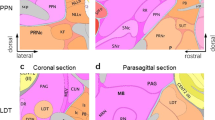
Under anesthesia with Equithesin (0.3 ml/100 g i.p.), rats were placed in a stereotaxic apparatus (David Kopf Instruments, Tujunga, CA, USA) with the skull exposed and a small hole drilled to expose the dura. A concentric self-made dialysis probe (2 mm dialyzing surface, length) (AN 69AF; Hospal-Dasco, Bologna, Italy; cut-off 40 000 Daltons) was inserted vertically into the nucleus accumbens shell (coordinates in millimeters from bregma: Anterior +3.6, Lateral −1.4, Ventral −7.8 from dura) according to the rat brain atlas by Paxinos and Watson (1986). Experiments were performed on freely moving rats 20–24 h after the surgical implant. Ringer's solution (147.0 mM NaCl, 2.2 mM CaCl2, and 4.0 mM KCl) was delivered through the dialysis probes at a constant flow rate of 1 μl/min. Collection of dialysate samples (10 μl) started after 60 min, and samples were taken every 20 min. Dialysate samples (10 μl) were analyzed by high-performance liquid chromatography (HPLC) to quantify DA (supplementary Materials and Methods). Rats were treated only after dopamine values (<10% variability) were stable for at least three consecutive samples. After the experiments, rats were killed with an overdose of Equithesin, the brain was removed and stored with 4% formalin in 0.1 M phosphate buffer until histological verification. Coronal sections (40 μm thick) were made with a Vibratome and the location of probes was verified according to the atlas of Paxinos and Watson (1986). Only data from rats with correct probe placement into the nucleus accumbens shell was included in the analysis of results.
Data Analysis
Data were subjected to repeated measures ANOVAs, followed when appropriate by post hoc Dunnett's tests for comparisons with the baseline (BL) condition (the BL value was the mean of the values the day before each test session with an injection with the appropriate vehicle) for self-administration studies under FR5 schedule of reinforcement; and by post hoc Newman–Keuls tests for multiple comparisons for studies on reinstatement of nicotine seeking behavior and on nicotine discrimination.
For the microdialysis experiment, results are expressed as a percentage of basal DA values. Basal DA values were calculated as the mean of three consecutive samples (differing no more than 10%) immediately preceding either the nicotine or saline injection. Statistical analysis was carried out using one- or two-way ANOVAs for repeated measures over time applied to the data obtained from serial assays of dialysate DA, normalized as a percentage of basal DA values for each group, with results from treatments showing overall changes subjected to post hoc Tukey's tests. Changes were considered significant when p<0.05.
RESULTS
Effects of Prazosin on Nicotine or Food Self-Administration Under the FR5 Schedule
The ANOVA performed on the number of nicotine injections received by the rats (group 1) showed a main effect of treatment (F4,52=14.4, p<0.0001). Pairwise comparisons with the BL level indicated that pretreatment with 0.5 or 1 mg/kg prazosin 30 min before the session, or saline substitution, significantly reduced the number of injections received by the rats during the session (p<0.05; p<0.01 and p<0.001, respectively) (Figure 1a).
(a) Effects of prazosin pretreatment (0.25–1 mg/kg, i.p. 30 min before the session) on self-administration of nicotine (0.03 mg/kg/injection) under a FR5 schedule. N=14. (b) Effects of prazosin pretreatment (0.5–1 mg/kg, i.p. 30 min before the session) on self-administration of food pellets under a FR5 schedule. N=11. Data are expressed as means (±SEM) of the number of injections per session during baseline conditions (BL), during sessions with prazosin pretreatment, and during sessions with vehicle pretreatment and saline substitution (extinction, EXT). *p<0.05; **p<0.01, ***p<0.001 vs baseline (BL), Dunnett's test after significant ANOVA for repeated measures.
The ANOVA performed on the number of food pellets that the rats (group 2) received showed a main effect of treatment (F2,20=5.9, p<0.01). Pairwise comparisons with the BL level indicated that pretreatment with 0.5 mg/kg prazosin 30 min before the session significantly enhanced the number of food pellets received by the rats during the session (p<0.01) (Figure 1b). The number of active lever presses was increased by pretreatment with prazosin at 0.5 and 1 mg/kg during food self-administration sessions (p<0.01 and p<0.05, respectively; data not shown).
These results suggest that noradrenergic α1 receptor blockade by prazosin dose-dependently and selectively reduced the self-administration of nicotine under a FR5 schedule of reinforcement in rats.
Effects of Repeated Prazosin Treatment for Three Consecutive Sessions on Nicotine or Food Self-Administration Under the FR5 Schedule
The administration of prazosin at 0.5 or 1 mg/kg to the rats from group 1, or saline substitution, during three consecutive sessions, induced a significant main effect (ANOVA: F6,48=10.29, p<0.0001). Post hoc analysis indicated that pretreatment with 1 mg/kg prazosin decreased the number of nicotine injections received by the rats in each session (p<0.05, p<0.01 and p<0.001 vs BL for injection days 1, 2, and 3, respectively), as well as the saline substitution (p<0.001 on day 1, 2, and 3 vs BL) (Figure 2a).
Effects of prazosin pretreatment (0.5 and 1 mg/kg, i.p. 30 min before the session) on self-administration of nicotine (0.03 mg/kg/injection) (a) or food pellets (b) under a FR5 schedule during three consecutive daily sessions. Data are expressed as means (±SEM) of the number of injections or food pellets that the rats received during baseline conditions (BL), during three consecutive sessions with prazosin pretreatment (0.5 and 1 mg/kg) and during three consecutive sessions with vehicle pretreatment and saline substitution (only for nicotine self-administration). N=14 for nicotine self-administration; N=11 for food self-administration. *p<0.05; **p<0.01, ***p<0.001 vs baseline (BL), Dunnett's test after significant ANOVA for repeated measures.
The ANOVA performed on the number of food pellets that the rats from group 2 received during three consecutive sessions with prazosin pretreatment (0 (BL), 0.5, and 1 mg/kg) showed no significant effect of treatment (F6,60=1.9, NS).
These results indicate that the effect of prazosin at 1 mg/kg in reducing nicotine self-administration persists over three consecutive daily sessions.
Effects of Prazosin on Nicotine- or Food-Induced Reinstatement
The ANOVAs performed on active lever presses of rats from group 3 (nicotine priming) or 2 (food priming) indicated a main effect of treatment (F4,36=6.9, p<0.001 and F3,30=6.3, p<0.01, respectively). The post hoc analysis showed that the nicotine or food priming induced a significant reinstatement (p<0.001 and p<0.01 vs BL, for nicotine seeking and for food seeking, respectively) and that pretreatment with prazosin at 0.5 and 1 mg/kg significantly decreased the nicotine-induced reinstatement (p<0.05 and p<0.01 vs reinstatement under vehicle pretreatment, respectively), but not the food-induced reinstatement (Figure 3). In addition, there was no difference between the baseline responding (no priming) and the nicotine-induced reinstatement with prazosin pretreatment at 0.5 and 1 mg/kg. Prazosin (0.25–1 mg/kg), administered i.p., 30 min before an injection of vehicle (s.c., 10 min before the session without nicotine priming), did not modify the number of active lever presses (ANOVA: F3,27=0.37, NS, data not shown).
Effect of prazosin pretreatment (0.25–1 mg/kg, i.p. 40 min before the session) on reinstatement of nicotine (a) or food (b) seeking after extinction induced by a priming injection of nicotine (0.15 mg/kg) or food priming, respectively. Data are expressed as means (±SEM) of the number of active lever presses during baseline conditions (BL) and during sessions with vehicle (0 mg/kg) or prazosin pretreatment. n=10 for nicotine priming and n=11 for food priming. *p<0.05; **p<0.01; ***p<0.001 vs baseline; #p<0.05; ##p<0.01 vs vehicle pretreatment (0); Student Newman–Keuls multiple comparison test after significant ANOVA for repeated measures.
Thus, noradrenergic α1 receptor blockade by prazosin selectively prevented the nicotine-induced reinstatement of nicotine seeking in rats without producing any effect on its own.
Effects of Prazosin on Cue-Induced Reinstatement of Nicotine-Seeking Behavior
The ANOVA performed on the active lever presses of rats from group 1 indicated a main effect of treatment (F4,59=9.2, p<0.0001), and the post hoc analysis showed that the cue presentation induced a significant reinstatement of the presses on the active lever (p<0.001 vs BL) and that pretreatment with prazosin at 0.5 and 1 mg/kg significantly decreased this cue-induced reinstatement (p<0.05 and p<0.01 vs reinstatement under vehicle pretreatment, respectively). In addition, there was no difference between the baseline responding (no cue) and the cue-induced reinstatement with prazosin pretreatment at 0.5 and 1 mg/kg, suggesting a dose-dependent prevention of the cue-induced reinstatement of nicotine seeking in rats by prazosin (Figure 4). Prazosin (0.25–1 mg/kg), administered i.p., 30 min before the session without cue presentation, did not modify the number of active lever presses (ANOVA: F3,33=0.73, NS, data not shown).
Effect of prazosin pretreatment (0.25–1 mg/kg, i.p. H-30 min) on cue-induced reinstatement of nicotine seeking after extinction. Data are expressed as means (±SEM) of the number of active lever presses during baseline conditions (BL, no nicotine-associated cues) and during sessions with vehicle (0 mg/kg) or prazosin pretreatment and the presence of nicotine-associated cues. N=12. ***p<0.001 vs baseline; #p<0.05; ##p<0.01 vs vehicle pretreatment (0); Student Newman–Keuls multiple comparison test after significant ANOVA for repeated measures.
Effects of Prazosin on Inactive Lever Presses During Self-Administration and Reinstatement Studies
The ANOVAs performed on the numbers of inactive lever presses during self-administration of nicotine or food under the FR5 schedule and during reinstatement of extinguished nicotine seeking in all conditions tested were not significant (Table 1), indicating that the effects of prazosin were selective for responding on the active lever.
Effects of Prazosin on Nicotine Discrimination
The two-way ANOVA performed on the percentage of correct responses for the dose-response curve for nicotine discrimination (0.01–0.4 mg/kg), with or without prazosin pretreatment (0.25–1 mg/kg), indicated a significant nicotine effect (F4,44=216.8, p<0.0001), and post hoc analysis showed a dose-dependent increase in nicotine-lever selection with increases in dose, with maximal nicotine-lever selection at the 0.4 mg/kg training dose of nicotine (Figure 5a).
(a) Dose-effect functions for the discriminative-stimulus effects of nicotine in rats (n=12) trained to discriminate 0.4 mg/kg nicotine from saline. The percentage of responses on the lever associated with nicotine administration is shown as a function of dose (mg/kg) during tests with various nicotine doses. Prazosin given acutely at 1 mg/kg 30 min before the session did not modify the discrimination of nicotine (no shift of the curve). (b) Effects of prazosin (0.25–1 mg/kg) on the discrimination of the training dose of nicotine (0.4 mg/kg) (top) and on the responses on the nicotine lever when administered alone (bottom). Results represent the means of the percentage of responses on the nicotine lever±SEM from 12 rats.
Prazosin doses from 0.25 to 1 mg/kg did not significantly alter the percentage of responses on the nicotine lever for any nicotine dose (two-way ANOVA, prazosin effect: F3,33=0.09, NS), indicating that noradrenergic α1 receptor blockade by prazosin did not modify the ability of rats to discriminate nicotine from saline. Figure 5a only shows the effect of the 1 mg/kg dose of prazosin, for clarity. Also, prazosin did not produce any nicotine-like effects (<5% of responses emitted on the nicotine-associated lever) with doses of prazosin ranging from 0.25 to 1 mg/kg (one-way ANOVA: F3,33=0.98, NS) (see Figure 5b, bottom). Finally, prazosin (0.25–1 mg/kg) also did not significantly modify the rate of responding by the rats at any nicotine dose (Table 2).
Effects of Prazosin on Nicotine-Induced Elevations in Dopamine Levels in the Nucleus Accumbens Shell
Administration of 0.15 mg/kg. nicotine (s.c.) significantly increased extracellular DA levels in dialysates from the nucleus accumbens shell (one-way ANOVA, F(10,54)=4.55, p=0.003) (Figure 6). Pretreatment with 1 mg/kg prazosin (i.p.), administered 30 min before nicotine, significantly reduced the effects of 0.15 mg/kg nicotine on extracellular DA levels in the shell of the accumbens (two-way ANOVA; main effect treatment, F(1,8)=6.04, p<0.05; main effect time, F(6,48)=6.16, p<0.001; time–treatment interaction, F(6,48)=1.17, NS). Post hoc tests show a significantly greater release of DA in the saline+nicotine-treated group as compared with the prazosin+nicotine treatment group (p<0.05). Administration of prazosin (1 mg/kg i.p.) by itself did not alter extracellular levels of DA in the shell of the nucleus accumbens (one-way ANOVA, F(10,65)=0.91, NS). These results indicate that nicotine at 0.15 mg/kg, s.c., induced a significant enhancement of DA release in the nucleus accumbens shell, and that pretreatment with prazosin significantly reduced this effect, without producing any effect on its own.
Effects of prazosin on nicotine-induced elevations in dopamine (DA) levels in the nucleus accumbens shell. Arrows represent the times of prazosin and nicotine injection. Results are means, with vertical bars representing SEM of dopamine levels in 20-min dialysate samples, expressed as a percentage of basal values. *p<0.05 vs vehicle+nicotine administration, Tukey's test.
DISCUSSION
In this study, noradrenergic α1 receptor blockade by the selective antagonist prazosin dose dependently and persistently (over three consecutive daily sessions) reduced nicotine self-administration and, as well, reduced the ability of nicotine to increase levels of DA in the nucleus accumbens shell. Noradrenergic α1 receptor blockade by prazosin also dose-dependently blocked the reinstatement of extinguished nicotine-seeking behavior that was induced by a priming injection of nicotine or by nicotine-associated cues. However, prazosin was not discriminated as nicotine-like and failed to change the discriminative stimulus effects of a range of doses of nicotine, suggesting that the effects of prazosin were not a result of a disruption of nicotine's interoceptive effects; but the use of a different rat strain and dark–light phase for the discrimination experiment compared with the self-administration and microdialysis experiments may limit this conclusion. Finally, prasozin did not produce any depressant effects on food self-administration and did not present observable toxicity, either alone or in combination with nicotine. Taken together, these results support further investigation on the effect of noradrenergic α1 receptor blockade using human models of tobacco self-administration and relapse to evaluate the potential of this new approach for assisting in the achievement of smoking cessation (Henningfield et al., 2009).
Several issues concerning the specificity of the effects of prazosin need to be considered. First, in this experiment, nicotine was available 7 days a week, suggesting that any variability in the pattern of nicotine intake cannot be attributed to off days or nicotine withdrawal. Second, the effects of prazosin on nicotine self-administration and on reinstatement of nicotine seeking was not likely due to impairment of operant responding, nor to a possible decrease in general motivation because prazosin did not reduce self-administration of food or food-induced reinstatement of food-seeking. It should be noted that the rate of responding during food self-administration under the FR5 schedule was far higher than that observed during nicotine self-administration under the same schedule, which may raise concerns about the appropriateness of this control for operant performance. However, responding during food- and nicotine-induced reinstatement experiments was similar.
Interestingly, prazosin pretreatment enhanced the number of active lever presses during food self-administration sessions. This effect is consistent with previous studies showing that prazosin increases total cumulative food intake of rats under heroin self-administration (Greenwell et al., 2009) and reverses cocaine-induced hypophagia in rats (Wellman et al., 2002). In addition, previous studies in rats have shown that prazosin, in the same range of doses employed here, does not modify locomotor activity (Forget et al., 2009b) and does not alter the rate of heroin or cocaine self-administration (Greenwell et al., 2009; Wee et al., 2008). Finally, prazosin is used as an antihypertensive drug in humans (see Reid and Vincent (1986) for review), suggesting that a hypotensive effect of the drug could be a confounding factor in our study, but this is unlikely because a prasozin dose of 3.15 mg/kg (a dose far higher than the doses of prasozin that effectively reduced abuse-related behavioral and neurochemical effects of nicotine in this study), does not significantly alter blood pressure in rats (Sommermeyer et al., 1995). Thus, the effects of prazosin on nicotine intake observed in our study were likely due to a reduction of the reinforcing efficacy of nicotine. This is supported by our previous finding that prazosin, at doses similar to those in this study, decreases the development of nicotine-induced CPP in rats without producing any motivational effects of its own (Forget et al., 2009b).
The finding that noradrenergic α1 receptor blockade reduced nicotine self-administration in our study may seem inconsistent with several reports that noradrenaline reuptake inhibitors also reduce this behavior (Rauhut et al., 2002; Coen et al., 2009), but this might be explained by the antagonistic activity of these noradrenaline reuptake inhibitors on nAChRs (Hennings et al., 1999, Miller et al., 2002).
We found that prazosin, in parallel with its effects on nicotine self-administration and reinstatement of nicotine seeking, also reduced nicotine-induced elevations in DA levels in the nucleus accumbens shell. This finding suggests that the ability of nicotine to stimulate the mesolimbic DA system is under the control of the noradrenergic system via stimulation of noradrenergic α1 receptors. This is in accordance with several reports describing the modulatory action of the noradrenergic system in general, and of noradrenergic α1 receptors in particular, on the mesolimbic DA system. Indeed, NA neurons provide excitatory input to midbrain DA neurons (Berridge et al., 1997; Morrison et al., 1981), and burst firing of DA neurons in the ventral tegmental area that is induced by electrical stimulation of the locus coeruleus is dose dependently blocked by prazosin (Grenhoff et al., 1993). Similarly, prazosin has been reported to abolish the increase in burst firing of VTA DA neurons induced by d-amphetamine without affecting their basal firing rate (Shi et al., 2000) and to attenuate nicotine-induced elevations in DA levels in the nucleus accumbens shell of rats subjected to subchronic administration of tranylcypromine, an irreversible monoamine oxidase inhibitor that potentiates nicotine self-administration behavior (Villegier et al., 2007).
Considering that the mesolimbic dopaminergic system is critical for the reinforcing effects of drugs of abuse, including nicotine (Balfour, 2002; Di Chiara, 2000; Di Chiara and Imperato, 1988), and for the reinstatement of extinguished drug seeking (Kalivas and McFarland, 2003; Shaham et al., 2003), it is reasonable to hypothesize that inhibition of nicotine-induced DA release in the shell of the nucleus accumbens by prazosin may be responsible for the inhibitory effect of this noradrenergic α1 receptor antagonist on nicotine self-administration and on reinstatement of nicotine seeking by a nicotine priming injection. The modulatory effects of prazosin on the mesolimbic DA system may also explain its effects on cue-induced reinstatement of nicotine seeking, since the presentation of drug-associated cues (including nicotine-associated cues) can induce a release of DA in the nucleus accumbens by itself (Bassareo et al., 2007; Di Ciano et al., 1998; Weiss et al., 2000).
The brain area(s) potentially responsible for the reduction by prazosin of the abuse-related behavioral and biochemical effects of nicotine are still unknown, but the literature can give us several indications. In rats, systemic injection of nicotine or presentation of reward-predicting stimuli enhance NA outflow within the prefrontal cortex (Mingote et al., 2004; Summers and Giacobini, 1995), and NA transmission in the prefrontal cortex is necessary for the rewarding and DA-releasing effects of cocaine and amphetamine in the mesoaccumbens (Ventura et al., 2003; Ventura et al., 2007). In addition, local administration of prazosin in the rat prefrontal cortex blocks both the hyperactivity induced by amphetamine and the DA-releasing effect of amphetamine in the nucleus accumbens (Darracq et al., 1998).
Together, these previous findings suggest that in our present study, nicotine or nicotine-associated cues induced a release of NA in the prefrontal cortex, stimulating noradrenergic α1 receptors in this structure. This may have resulted in the release of DA in the nucleus accumbens shell and, subsequently, the development of nicotine self-administration behavior and relapse to nicotine-seeking behavior.
It would be interesting in future studies to evaluate the effects of local infusion of prazosin within the prefrontal cortex on nicotine self-administration and reinstatement of nicotine seeking.
In conclusion, our results show that the blockade of noradrenergic α1 receptors by prazosin in rats reduces the self-administration of nicotine (but not of food) and reduces both nicotine- and cue-induced reinstatement of extinguished nicotine seeking, without altering food-induced reinstatement of food seeking or discrimination of nicotine. In addition, prazosin reduces the release of DA in the nucleus accumbens shell induced by nicotine. As a recent pilot study indicated that prazosin administration can reduce alcohol consumption in dependent patients without any adverse effects (Simpson et al., 2009), blocking noradrenergic α1 receptors may also be an interesting new therapeutic approach for tobacco dependence.
References
Balfour DJ (2002). Neuroplasticity within the mesoaccumbens dopamine system and its role in tobacco dependence. Curr Drug Targets CNS Neurol Disord 1: 413–421.
Bassareo V, De Luca MA, Di Chiara G (2007). Differential impact of pavlovian drug conditioned stimuli on in vivo dopamine transmission in the rat accumbens shell and core and in the prefrontal cortex. Psychopharmacology (Berlin) 191: 689–703.
Berridge CW, Stratford TL, Foote SL, Kelley AE (1997). Distribution of dopamine beta-hydroxylase-like immunoreactive fibers within the shell subregion of the nucleus accumbens. Synapse 27: 230–241.
Carter LP, Griffiths RR (2009). Principles of laboratory assessment of drug abuse liability and implications for clinical development. Drug Alcohol Depend 105 (Suppl 1): S14–S25.
Coen KM, Adamson KL, Corrigall WA (2009). Medication-related pharmacological manipulations of nicotine self-administration in the rat maintained on fixed- and progressive-ratio schedules of reinforcement. Psychopharmacology (Berlin) 201: 557–568.
Corrigall WA, Coen KM (1989). Nicotine maintains robust self-administration in rats on a limited-access schedule. Psychopharmacology (Berlin) 99: 473–478.
Corrigall WA, Coen KM, Zhang J, Adamson KL (2001). GABA mechanisms in the pedunculopontine tegmental nucleus influence particular aspects of nicotine self-administration selectively in the rat. Psychopharmacology (Berlin) 158: 190–197.
Darracq L, Blanc G, Glowinski J, Tassin JP (1998). Importance of the noradrenaline-dopamine coupling in the locomotor activating effects of D-amphetamine. J Neurosci 18: 2729–2739.
Di Chiara G (2000). Role of dopamine in the behavioural actions of nicotine related to addiction. Eur J Pharmacol 393: 295–314.
Di Chiara G, Imperato A (1988). Drugs abused by humans preferentially increase synaptic dopamine concentrations in the mesolimbic system of freely moving rats. Proc Natl Acad Sci USA 85: 5274–5278.
Di Ciano P, Blaha CD, Phillips AG (1998). Conditioned changes in dopamine oxidation currents in the nucleus accumbens of rats by stimuli paired with self-administration or yoked-administration of d-amphetamine. Eur J Neurosci 10: 1121–1127.
Forget B, Coen KM, Le Foll B (2009a). Inhibition of fatty acid amide hydrolase reduces reinstatement of nicotine seeking but not break point for nicotine self-administration-comparison with CB(1) receptor blockade. Psychopharmacology (Berlin) 205: 613–624.
Forget B, Hamon M, Thiebot MH (2009b). Involvement of alpha1-adrenoceptors in conditioned place preference supported by nicotine in rats. Psychopharmacology (Berlin) 205: 503–515.
Fu Y, Matta SG, Brower VG, Sharp BM (2001). Norepinephrine secretion in the hypothalamic paraventricular nucleus of rats during unlimited access to self-administered nicotine: An in vivo microdialysis study. J Neurosci 21: 8979–8989.
Fu Y, Matta SG, James TJ, Sharp BM (1998). Nicotine-induced norepinephrine release in the rat amygdala and hippocampus is mediated through brainstem nicotinic cholinergic receptors. J Pharmacol Exp Ther 284: 1188–1196.
Fu Y, Matta SG, Kane VB, Sharp BM (2003). Norepinephrine release in amygdala of rats during chronic nicotine self-administration: an in vivo microdialysis study. Neuropharmacology 45: 514–523.
Gasior M, Shoaib M, Yasar S, Jaszyna M, Goldberg SR (1999). Acquisition of nicotine discrimination and discriminative stimulus effects of nicotine in rats chronically exposed to caffeine. J Pharmacol Exp Ther 288: 1053–1073.
Greenwell TN, Walker BM, Cottone P, Zorrilla EP, Koob GF (2009). The alpha1 adrenergic receptor antagonist prazosin reduces heroin self-administration in rats with extended access to heroin administration. Pharmacol Biochem Behav 91: 295–302.
Grenhoff J, Nisell M, Ferre S, Aston-Jones G, Svensson TH (1993). Noradrenergic modulation of midbrain dopamine cell firing elicited by stimulation of the locus coeruleus in the rat. J Neural Transm Gen Sect 93: 11–25.
Henningfield JE, Shiffman S, Ferguson SG, Gritz ER (2009). Tobacco dependence and withdrawal: science base, challenges and opportunities for pharmacotherapy. Pharmacol Ther 123: 1–16.
Hennings EC, Kiss JP, De Oliveira K, Toth PT, Vizi ES (1999). Nicotinic acetylcholine receptor antagonistic activity of monoamine uptake blockers in rat hippocampal slices. J Neurochem 73: 1043–1050.
Le Foll B, Goldberg SR (2009). Effects of nicotine in experimental animals and humans: an update on addictive properties. Handb Exp Pharmacol 192: 335–367.
Kalivas PW, McFarland K (2003). Brain circuitry and the reinstatement of cocaine-seeking behavior. Psychopharmacology (Berlin) 168: 44–56.
Miller DK, Wong EH, Chesnut MD, Dwoskin LP (2002). Reboxetine: functional inhibition of monoamine transporters and nicotinic acetylcholine receptors. J Pharmacol Exp Ther 302: 687–695.
Mingote S, de Bruin JP, Feenstra MG (2004). Noradrenaline and dopamine efflux in the prefrontal cortex in relation to appetitive classical conditioning. J Neurosci 24: 2475–2480.
Moore RY, Bloom FE (1979). Central catecholamine neuron systems: anatomy and physiology of the norepinephrine and epinephrine systems. Annu Rev Neurosci 2: 113–168.
Morrison JH, Molliver ME, Grzanna R, Coyle JT (1981). The intra-cortical trajectory of the coeruleo-cortical projection in the rat: a tangentially organized cortical afferent. Neuroscience 6: 139–158.
Nicholas AP, Hokfelt T, Pieribone VA (1996). The distribution and significance of CNS adrenoceptors examined with in situ hybridization. Trends Pharmacol Sci 17: 245–255.
Paxinos G, Watson C (1986). The rat brain in stereotaxic coordinates (2nd edn), Academic Press, San Diego, CA.
Rauhut AS, Mullins SN, Dwoskin LP, Bardo MT (2002). Reboxetine: attenuation of intravenous nicotine self-administration in rats. J Pharmacol Exp Ther 303: 664–672.
Reid JL, Vincent J (1986). Clinical pharmacology and therapeutic role of prazosin and related alpha-adrenoceptor antagonists. Cardiology 73: 164–174.
Shaham Y, Shalev U, Lu L, De Wit H, Stewart J (2003). The reinstatement model of drug relapse: history, methodology and major findings. Psychopharmacology (Berlin) 168: 3–20.
Sharp BM, Matta SG (1993). Detection by in vivo microdialysis of nicotine-induced norepinephrine secretion from the hypothalamic paraventricular nucleus of freely moving rats: dose-dependency and desensitization. Endocrinology 133: 11–19.
Shi WX, Pun CL, Zhang XX, Jones MD, Bunney BS (2000). Dual effects of D-amphetamine on dopamine neurons mediated by dopamine and nondopamine receptors. J Neurosci 20: 3504–3511.
Simpson TL, Saxon AJ, Meredith CW, Malte CA, McBride B, Ferguson LC et al. (2009). A pilot trial of the alpha-1 adrenergic antagonist, prazosin, for alcohol dependence. Alcohol Clin Exp Res 33: 255–263.
Sommermeyer H, Frielingsdorf J, Knorr A (1995). Effects of prazosin on the dopaminergic neurotransmission in rat brain. Eur J Pharmacol 276: 267–270.
Stolerman IP, Naylor C, Elmer GI, Goldberg SR (1999). Discrimination and self-administration of nicotine by inbred strains of mice. Psychopharmacology (Berlin) 141: 297–306.
Summers KL, Giacobini E (1995). Effects of local and repeated systemic administration of (-)nicotine on extracellular levels of acetylcholine, norepinephrine, dopamine, and serotonin in rat cortex. Neurochem Res 20: 753–759.
Ventura R, Cabib S, Alcaro A, Orsini C, Puglisi-Allegra S (2003). Norepinephrine in the prefrontal cortex is critical for amphetamine-induced reward and mesoaccumbens dopamine release. J Neurosci 23: 1879–1885.
Ventura R, Morrone C, Puglisi-Allegra S (2007). Prefrontal/accumbal catecholamine system determines motivational salience attribution to both reward- and aversion-related stimuli. Proc Natl Acad Sci USA 104: 5181–5186.
Villegier AS, Lotfipour S, Belluzzi JD, Leslie FM (2007). Involvement of alpha1-adrenergic receptors in tranylcypromine enhancement of nicotine self-administration in rat. Psychopharmacology (Berlin) 193: 457–465.
Walker BM, Rasmussen DD, Raskind MA, Koob GF (2008). alpha1-noradrenergic receptor antagonism blocks dependence-induced increases in responding for ethanol. Alcohol 42: 91–97.
Wee S, Mandyam CD, Lekic DM, Koob GF (2008). Alpha 1-noradrenergic system role in increased motivation for cocaine intake in rats with prolonged access. Eur Neuropsychopharmacol 18: 303–311.
Weinshenker D, Schroeder JP (2007). There and back again: a tale of norepinephrine and drug addiction. Neuropsychopharmacology 205: 613–624.
Weiss F, Maldonado-Vlaar CS, Parsons LH, Kerr TM, Smith DL, Ben-Shahar O (2000). Control of cocaine-seeking behavior by drug-associated stimuli in rats: effects on recovery of extinguished operant-responding and extracellular dopamine levels in amygdala and nucleus accumbens. Proc Natl Acad Sci USA 97: 4321–4326.
Wellman P, Ho D, Cepeda-Benito A, Bellinger L, Nation J (2002). Cocaine-induced hypophagia and hyperlocomotion in rats are attenuated by prazosin. Eur J Pharmacol 455: 117–126.
Zarrindast MR, Bahreini T, Adl M (2002). Effect of imipramine on the expression and acquisition of morphine-induced conditioned place preference in mice. Pharmacol Biochem Behav 73: 941–949.
Zhang XY, Kosten TA (2005). Prazosin, an alpha-1 adrenergic antagonist, reduces cocaine-induced reinstatement of drug-seeking. Biol Psychiatry 57: 1202–1204.
Acknowledgements
We declare that this work was supported by a Research Student Grant from the Canadian Tobacco Control Research Initiative awarded to BF (PI) and by the Intramural Research Program of the National Institute on drug Abuse, National Institutes of Health, Department of Health and Human Services. We declare that over the past 3 years, BLF has received financial support by Pfizer and Nuvis for research grants and speaker fees.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors do not have any conflicts of interest, financial or otherwise, that might bias this work.
Additional information
Supplementary Information accompanies the paper on the Neuropsychopharmacology website
Supplementary information
Rights and permissions
About this article
Cite this article
Forget, B., Wertheim, C., Mascia, P. et al. Noradrenergic α1 Receptors as a Novel Target for the Treatment of Nicotine Addiction. Neuropsychopharmacol 35, 1751–1760 (2010). https://doi.org/10.1038/npp.2010.42
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2010.42
Keywords
This article is cited by
-
Tobacco and nicotine use
Nature Reviews Disease Primers (2022)
-
The role of anterior insula–brainstem projections and alpha-1 noradrenergic receptors for compulsion-like and alcohol-only drinking
Neuropsychopharmacology (2021)
-
Nicotine-induced enhancement of a sensory reinforcer in adult rats: antagonist pretreatment effects
Psychopharmacology (2021)
-
Effects of disulfiram on choice behavior in a rodent gambling task: association with catecholamine levels
Psychopharmacology (2018)
-
Nicotine self-administration research: the legacy of Steven R. Goldberg and implications for regulation, health policy, and research
Psychopharmacology (2016)