Abstract
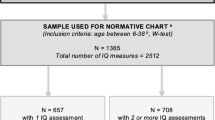
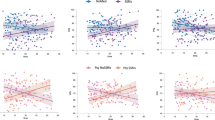
The 22q11.2 deletion syndrome (22q11DS) presents with medical and neuropsychiatric manifestations including neurocognitive deficits. Quantitative neurobehavioral measures linked to brain circuitry can help elucidate genetic mechanisms contributing to deficits. To establish the neurocognitive profile and neurocognitive ‘growth charts’, we compared cross-sectionally 137 individuals with 22q11DS ages 8–21 to 439 demographically matched non-deleted individuals with developmental delay (DD) and medical comorbidities and 443 typically developing (TD) participants. We administered a computerized neurocognitive battery that measures performance accuracy and speed in executive, episodic memory, complex cognition, social cognition and sensorimotor domains. The accuracy performance profile of 22q11DS showed greater impairment than DD, who were impaired relative to TD. Deficits in 22q11DS were most pronounced for face memory and social cognition, followed by complex cognition. Performance speed was similar for 22q11DS and DD, but 22q11DS individuals were differentially slower in face memory and emotion identification. The growth chart, comparing neurocognitive age based on performance relative to chronological age, indicated that 22q11DS participants lagged behind both groups from the earliest age assessed. The lag ranged from less than 1 year to over 3 years depending on chronological age and neurocognitive domain. The greatest developmental lag across the age range was for social cognition and complex cognition, with the smallest for episodic memory and sensorimotor speed, where lags were similar to DD. The results suggest that 22q11.2 microdeletion confers specific vulnerability that may underlie brain circuitry associated with deficits in several neuropsychiatric disorders, and therefore help identify potential targets and developmental epochs optimal for intervention.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Bassett AS, McDonald-McGinn DM, Devriendt K, Digilio MC, Goldenberg P, Habel A et al. Practical guidelines for managing patients with 22q11.2 deletion syndrome. J Pediatrics 2011; 159: 332–339.
Antshel KM, Fremont W, Roizen NJ, Shprintzen R, Higgins AM, Dhamoon A et al. ADHD, major depressive disorder, and simple phobias are prevalent psychiatric conditions in youth with velo cardio facial syndrome. J Am Acad Child Adolesc Psychiatry 2006; 45: 596–603.
Bassett AS, Chow EW, AbdelMalik P, Gheorghiu M, Husted J, Weksberg R . The schizophrenia phenotype in 22q11 deletion syndrome. Am J Psychiatry 2003; 160: 1580–1586.
Fabbro A, Rizzi E, Schneider M, Debbane M, Eliez S . Depression and anxiety disorders in children and adolescents with velo-cardio-facial syndrome (VCFS). Eur Child Adolesc Psychiatry 2012; 21: 379–385.
Gothelf D, Feinstein C, Thompson T, Gu E, Penniman L, Van Stone E et al. Risk factors for the emergence of psychotic disorders in adolescents with 22q11.2 deletion syndrome. Am J Psychiatry 2007; 164: 663–669.
Green T, Gothelf D, Glaser B, Debbane M, Frisch A, Kotler M et al. Psychiatric disorders and intellectual functioning throughout development in velocardiofacial (22q11.2 deletion) syndrome. J Am Acad Child Adolesc Psychiatry 2009; 48: 1060–1068.
Tang SX, Yi JJ, Calkins ME, Whinna DA, Kohler CG, Souders MC et al. Psychiatric disorders in 22q11.2 deletion syndrome are prevalent but under-treated. Psycholo Med 2013; 9: 1–11.
Vorstman JA, Morcus ME, Duijff SN, Klaassen PW, Heineman-de Boer JA, Beemer FA et al. The 22q11.2 deletion in children: high rate of autistic disorders and early onset of psychotic symptoms. J Am Acad Child Adolesc Psychiatry 2006; 45: 1104–1113.
Hiroi N, Takahashi T, Hishimoto A, Izumi T, Boku S, Hiramoto T . Copy number variation at 22q11.2: from rare variants to common mechanisms of developmental neuropsychiatric disorders. Mol Psychiatry 2013; 18 11: 1153–1165.
Jonas RK, Montojo CA, Bearden CE . The 22q11.2 deletion syndrome as a window into complex neuropsychiatric disorders over the lifespan. Biol Psychiatry advance online publication, 27 August 2013; doi:10.1016/j.biopsych.2013.07.019 (e-pub ahead of print).
Karayiorgou M, Simon TJ, Gogos JA . 22q11.2 microdeletions: linking DNA structural variation to brain dysfunction and schizophrenia. Nat Rev Neurosci 2010; 11: 402–416.
Meechan DW, Maynard TM, Tucker ES, LaMantia AS . Three phases of DiGeorge/22q11 deletion syndrome pathogenesis during brain development: patterning, proliferation, and mitochondrial functions of 22q11 genes. Int J Dev Neurosci 2011; 29: 283–294.
Harper KM, Hiramoto T, Tanigaki K, Kang G, Suzuki G, Trimble W et al. Alterations of social interaction through genetic and environmental manipulation of the 22q11.2 gene Sept5 in the mouse brain. Hum Mol Genet 2012; 21: 3489–3499.
Duijff SN, Klaassen PW, de Veye HF, Beemer FA, Sinnema G, Vorstman JA . Cognitive development in children with 22q11.2 deletion syndrome. Br J Psychiatry 2012; 200: 462–468.
Bearden CE, Woodin MF, Wang PP, Moss E, McDonald-McGinn D, Zackai E et al. The neurocognitive phenotype of the 22q11.2 deletion syndrome: selective deficit in visual-spatial memory. J Clin Exper Neuropsychol 2001; 23: 447–464.
De Smedt B, Devriendt K, Fryns J-P, Vogels A, Gewillig M, Swillen A . Intellectual abilities in a large sample of children with velo—cardio—facial syndrome: an update. J Intellect Disabil Res 2007; 51: 666–670.
Bish JP, Ferrante SM, McDonald-McGinn D, Zackai E, Simon TJ . Maladaptive conflict monitoring as evidence for executive dysfunction in children with chromosome 22q11.2 deletion syndrome. Dev Sci 2005; 8: 36–43.
Campbell LE, Azuma R, Ambery F, Stevens A, Smith A, Morris RG et al. Executive functions and memory abilities in children with 22q11.2 deletion syndrome. Aust N Z J Psychiatry 2010; 44: 364–371.
Henry JC, van Amelsvoort T, Morris RG, Owen MJ, Murphy DG, Murphy KC . An investigation of the neuropsychological profile in adults with velo-cardio-facial syndrome (VCFS). Neuropsychologia 2002; 40: 471–478.
Rockers K, Ousley O, Sutton T, Schoenberg E, Coleman K, Walker E et al. Performance on the modified card sorting test and its relation to psychopathology in adolescents and young adults with 22q11.2 deletion syndrome. J Intellect Disabil Res 2009; 53: 665–676.
Sobin C, Kiley-Brabeck K, Daniels S, Blundell M, Anyane-Yeboa K, Karayiorgou M . Networks of attention in children with the 22q11 deletion syndrome. Dev Neuropsychol 2004; 26: 611–626.
Cabaral MH, Beaton EA, Stoddard J, Simon TJ . Impaired multiple object tracking in children with chromosome 22q11.2 deletion syndrome. J Neurodev Disord 2012; 4: 6.
Majerus S, Van der Linden M, Braissand V, Eliez S . Verbal short-term memory in individuals with chromosome 22q11.2 deletion: specific deficit in serial order retention capacities? Am J Ment Retard 2007; 112: 79–93.
Woodin M, Wang PP, Aleman D, McDonald-McGinn D, Zackai E, Moss E . Neuropsychological profile of children and adolescents with the 22q11.2 microdeletion. Genet Med 2001; 3: 34–39.
Gur RC, Richard J, Hughett P, Calkins ME, Macy L, Bilker WB et al. A cognitive neuroscience based computerized battery for efficient measurement of individual differences: standardization and initial construct validation. J Neurosci Methods 2010; 187: 254–262.
Roalf DR, Ruparel K, Gur RE, Bilker W, Gerraty R, Elliott MA et al.Neuroimaging predictors of cognitive performance across a standardized neurocognitive battery. Neuropschycology advance online publication, 23 December 2013 (e-pub ahead of print).
Calkins ME, Ray A, Gur RC, Freedman R, Green MF, Greenwood TA et al. Sex differences in familiality effects on neurocognitive performance in schizophrenia. Biol Psychiatry 2013; 73: 976–984.
Greenwood TA, Swerdlow NR, Gur RE, Cadenhead KS, Calkins ME, Dobie DJ et al. Genome-wide linkage analyses of 12 endophenotypes for schizophrenia from the consortium on the genetics of schizophrenia. Am J Psychiatry 2013; 170: 521–532.
Roalf DR, Gur RC, Almasy L, Richard J, Gallagher RS, Prasad K et al. Neurocognitive performance stability in a multiplex multigenerational study of schizophrenia. Schizophr Bull 2013; 39: 1008–1017.
Calkins ME, Tepper P, Gur RC, Ragland JD, Klei L, Wiener HW et al. Project among African-Americans to explore risks for schizophrenia (PAARTNERS): evidence for impairment and heritability of neurocognitive functioning in families of schizophrenia patients. Am J Psychiatry 2010; 167: 459–472.
Greenwood TA, Lazzeroni LC, Murray SS, Cadenhead KS, Calkins ME, Dobie DJ et al. Analysis of 94 candidate genes and 12 endophenotypes for schizophrenia from the Consortium on the Genetics of Schizophrenia. Am J Psychiatry 2011; 168: 930–946.
Gur RE, Nimgaonkar VL, Almasy L, Calkins ME, Ragland JD, Pogue-Geile MF et al. Neurocognitive endophenotypes in a multiplex multigenerational family study of schizophrenia. Am J Psychiatry 2007; 164: 813–819.
Gur RC, Richard J, Calkins ME, Chiavacci R, Hansen JA, Bilker WB et al. Age group and sex differences in performance on a computerized neurocognitive battery in children age 8-21. Neuropsychology 2012; 26: 251–265.
Goldenberg PC, Calkins ME, Richard J, McDonald-McGinn D, Zackai E, Mitra N et al. Computerized neurocognitive profile in young people with 22q11.2 deletion syndrome compared to youths with schizophrenia and at-risk for psychosis. Am J Med Genet B Neuropsychiatr Genet 2012; 159B: 87–93.
Gur RC, Calkins ME, Satterthwaite TD, Ruparel K, Bilker WB, Moore TM et al. Neurocognitive growth charting in psychosis spectrum youths. JAMA Psychiatry (in press)..
Brown TT, Kuperman JM, Chung Y, Erhart M, McCabe C, Hagler DJ et al. Neuroanatomical assessment of biological maturity. Curr Biol 2012; 22: 1693–1698.
Dosenbach NU, Nardos B, Cohen AL, Fair DA, Power JD, Church JA et al. Prediction of individual brain maturity using fMRI. Science 2010; 329: 1358–1361.
Satterthwaite TD, Elliott MA, Ruparel K, Loughead J, Prabhakaran K, Calkins ME et al. Neuroimaging of the Philadelphia Neurodevelopmental Cohort. Neuroimage 2013 doi:S1053-8119: 00833–1.
Kaufman J, Bismaher B, Brent DA, Rao U, Flynn C, Moreci P et al. Schedule for Affective Disorders and Schizophrenia for School-Aged Children - Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adol Psychiatry 1997; 36: 980–988.
Wilkinson GS, Robertson GJ . Wide Range Achievement Test Fourth Edition (WRAT4). Psychological Assessment Resources: Lutz, FL, USA, 2006.
Jalbrzikowski M, Carter C, Senturk D, Chow C, Hopkins JM, Green MF et al. Social cognition in 22q11.2 microdeletion syndrome: relevance to psychosis? Schizophr Res 2012; 142: 99–107.
Campbell L, McCabe K, Leadbeater K, Schall U, Loughland C, Rich D . Visual scanning of faces in 22q11.2 deletion syndrome: attention to the mouth or the eyes? Psychiatry Res 2010; 177: 211–215.
Andersson F, Glaser B, Spiridon M, Debbane M, Vuilleumier P, Eliez S . Impaired activation of face processing networks revealed by functional magnetic resonance imaging in 22q11.2 deletion syndrome. Biol Psychiatry 2008; 63: 49–57.
Gur RE, Loughead J, Kohler CG, Elliott MA, Lesko K, Ruparel K et al. Limbic activation associated with misidentification of fearful faces and flat affect in schizophrenia. Arch Gen Psychiatry 2007; 64: 1356–1366.
Pinkham AE, Loughead J, Ruparel K, Overton E, Gur RE, Gur RC . Abnormal modulation of amygdala activity in schizophrenia in response to direct- and averted-gaze threat-related facial expressions. Am J Psychiatry 2011; 168: 293–301.
Dalton KM, Nacewicz BM, Johnstone T, Schaefer HS, Gernsbacher MA, Goldsmith HH et al. Gaze fixation and the neural circuitry of face processing in autism. Nat Neurosci 2005; 8: 519–526.
Tottenham N, Hertzig ME, Gillespie-Lynch K, Gilhooly T, Millner AJ, Casey BJ . Elevated amygdala response to faces and gaze aversion in autism spectrum disorder. Soc Cogn Affect Neurosci 2014; 9: 106–117.
Shashi V, Veerapandiyan A, Schoch K, Kwapil T, Keshavan M, Ip E et al. Social skills and associated psychopathology in children with chromosome 22q11.2 deletion syndrome: implications for interventions. J Intellect Disabil Res 2012; 56: 865–878.
Scherer NJ, D'Antonio LL, Rodgers JR . Profiles of communication disorder in children with velocardiofacial syndrome: comparison to children with Down syndrome. Genet Med 2001; 3: 72–78.
Carlier M, Desplanches AG, Philip N, Stephanini S, Vicari S, Volterra V et al. Laterality preference and cognition: cross-syndrome comparison of patients with trisomy 21 (Down), del7q11.23 (Williams-Beuren) and del22q11.2 (DiGeorge or Velo-Cardio-Facial) syndromes. Behav Genet 2011; 41: 413–422.
Simon TJ, Yakarae Y, DeBoer T, McDonald-McGinn DM, Zackai EH, Ross JL . Overlapping numerical impairments in children with chromosome 22q11.2 deletion or Turner syndromes. Neuropsychologia 2007; 46: 82–94.
McNeil TF, Cantor-Graae E, Blennow G . Mental correlates of neuromotoric deviation in 6-year olds at heightened risk for schizophrenia. Schizophr Res 2003; 60: 219–228.
Buka SL, Seidman LJ, Tsuang MT, Goldstein JM . The New England family study high-risk project: Neurological impairments among offspring of parents with schizophrenia and other psychoses. Am J Med Genet B Neuropsychiatr Genet 2013; 162: 653–660.
Baker K, Vorstman JA . Is there a core neuropsychiatric phenotype in 22q11.2 deletion syndrome? Curr Opin Neurol 2012; 25: 131–137.
Kates WR, Antshel KM, Fremont WP, Shprintzen RJ, Strunge LA, Burnette CP et al. Comparing phenotypes in patients with idiopathic autism to patients with velocardiofacial syndrome (22q11 DS) with and without autism. Am J Med Genet A 2007; 143A: 2642–2650.
Suzuki G, Harper KM, Hiramoto T, Sawamura T, Lee M, Kang G et al. Sept5 deficiency exerts pleiotropic influence on affective behaviors and cognitive functions in mice. Hum Mol Genet 2009; 18: 1652–1660.
Hiroi N, Hiramoto T, Harper KM, Suzuki G, Boku S . Mouse models of 22q11.2-associated autism spectrum disorder. Autism 2012; S1: 1–9.
Babovic D, O’Tuathaigh CM, O’Connor AM, O’Sullivan GJ, Tighe O, Croke DT et al. Phenotypic characterization of cognition and social behavior in mice with heterozygous versus homozygous deletion of catechol-O-methyltransferase. Neuroscience 2008; 155: 1021–1029.
Hiramoto T, Kang G, Suzuki G, Satoh Y, Kucherlapati R, Watanabe Y et al. Tbx1: identification of a 22q11.2 gene as a risk factor for autism spectrum disorder in a mouse model. Hum Mol Genet 2011; 20: 4775–4785.
Acknowledgements
This study was supported by NIH grants MH087626, MH087636, MH089983 and MH089924. Additional support came from T32 MH019112 (JJY), the Doris Duke Charitable Foundation Clinical Research Fellowship (SXT) and K08 MH 079364 (MEC). We are grateful to the research participants and their parents. We thank Emily Wilkins, Catherine Conroy, Omar Abbas, Amy Cassidy, Allison Mott and Kosha Ruparel of the Neuropsychiatry Section at the University of Pennsylvania for data acquisition and coordination. We also thank Alice Bailey and Jhonna Corson of the ‘22q and You’ Center for clinical coordination of 22q11DS participants and Colleen Franconi and Meghan McNamara of the Human Genetics Division at the Children’s Hospital of Philadelphia for the genetic laboratory assessments of the 22q11DS participants. We also thank Dr Hakon Hakonarson and the Center for Applied Genomics at the Children’s Hospital of Philadelphia for their collaboration in establishing the Philadelphia Neurodevelopmental Cohort.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
PowerPoint slides
Rights and permissions
About this article
Cite this article
Gur, R., Yi, J., McDonald-McGinn, D. et al. Neurocognitive development in 22q11.2 deletion syndrome: comparison with youth having developmental delay and medical comorbidities. Mol Psychiatry 19, 1205–1211 (2014). https://doi.org/10.1038/mp.2013.189
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/mp.2013.189
Keywords
This article is cited by
-
A Developmentally Informed Systematic Review and Meta-Analysis of the Strength of General Psychopathology in Childhood and Adolescence
Clinical Child and Family Psychology Review (2024)
-
Altered functional brain dynamics in chromosome 22q11.2 deletion syndrome during facial affect processing
Molecular Psychiatry (2022)
-
Tbx1, a gene encoded in 22q11.2 copy number variant, is a link between alterations in fimbria myelination and cognitive speed in mice
Molecular Psychiatry (2022)
-
Two novel mouse models mimicking minor deletions in 22q11.2 deletion syndrome revealed the contribution of each deleted region to psychiatric disorders
Molecular Brain (2021)
-
Social cognition in 22q11.2 deletion syndrome and idiopathic developmental neuropsychiatric disorders
Journal of Neurodevelopmental Disorders (2021)