Abstract
In lung cancer, targetable activating alterations in cancer genes, such as EGFR, ALK, RET, ROS1 and MET, are usually mutually exclusive. Rare lung cancer cases with coexistent alterations of EGFR and ALK or EGFR mutations with RET or ROS1 rearrangements have been reported. In this study, we report 15 patients (3 men and 12 women; 14 Caucasians and 1 African American) with ages ranging from 43 to 81 years (median 60 years) with lung adenocarcinoma in which coexistent alterations of two cancer-associated genes, including ALK, ROS1, or RET rearrangement or MET amplification were present. The combination of alterations detected by fluorescence in situ hybridization included ALK combined with ROS1 (n=4), ALK with MET (n=3), ALK with RET (n=1); RET with MET (n=4), RET with ROS1 (n=2), and ROS1 combined with MET (n=1). The frequencies of involvement were similar for all 4 genes, 53% for both ALK and MET (n=8), 47% for both RET and ROS1 (n=7). Activating gene mutations were also detected by next-generation sequencing for TP53 (n=6), EGFR (n=5), KRAS (n=3) and STK11 (n=2). Nine patients reported a smoking history (8 heavy and 1 light) and 6 patients were non-smokers. These findings suggest the need for assessing a panel of genes in lung cancer. Since targetable agents are available for each of these activating alterations, treatment with more than one targeted agent may be beneficial for this rare group of patients.
Similar content being viewed by others
Main
Lung cancer is the most common cause of cancer-related deaths in the United States and many other countries.1, 2 The development of tyrosine kinase inhibitors against epidermal growth factor receptor (EGFR) gene mutations (eg, erlotinib) and anaplastic large-cell lymphoma kinase (ALK) gene rearrangement (eg, crizotinib) has dramatically improved the outcome of patients with lung cancer.3, 4, 5, 6 Additional novel oncogenic fusion genes with tyrosine kinase functions, such as RET and ROS1 as well as fusions genes combined with MET amplification have been identified and tyrosine kinase inhibitors targeting these molecular aberrations, eg, vandetanib against RET rearrangement,7, 8, 9 have entered into clinical trials. Historically, activating cancer gene mutations have been considered as mutually exclusive in lung cancer.10 However, a group of patients bearing co-alterations of EGFR and ALK has been reported recently,11, 12, 13, 14 and further studies have demonstrated that the addition of ALK inhibitor therapy improved the overall survival of these patients.15 Co-alterations of EGFR with genes other than ALK (eg, ROS1) have been reported in a few cases,16, 17, 18 but co-alterations of ALK, RET, ROS1 or MET in lung cancer have not been reported to the best of our knowledge. In this study, we report 15 cases of lung adenocarcinoma in which abnormalities of two cancer-associated genes including ALK, RET, ROS1 or MET. In 5 of these cases activating EGFR mutations were also present.
Materials and methods
Patients
We searched the database of the Clinical Cytogenetics Laboratory at The University of Texas MD Anderson Cancer Center for cases of lung cancer assessed by fluorescence in situ hybridization (FISH) for abnormalities of ALK, RET, ROS1 or MET. Fifteen cases with positive results of more than one of these genes were identified and a thorough chart review was performed. The clinical and laboratory information were collected and reviewed by following institutional guidelines with informed consent in accord with the Declaration of Helsinki.
Fluorescence In Situ Hybridization and Scoring
All tissue FISH tests were performed using formalin fixed, paraffin-embedded tissue sections of primary and/or metastatic lung cancer specimen and were validated for these specimens following the American College of Medical Genetics and Genomics guidelines.7, 19 The FDA-approved, LSI ALK dual color, breakapart probe was applied for detection of ALK rearrangement (Abbott Molecular, Des Plaines, IL). This probe hybridizes to band 2p23 (spectrum green on the centromeric side and spectrum orange on the telomeric side of the ALK breakpoint). Fifty nuclei were analyzed routinely, but the analysis was extended to 100 nuclei if results from counting 50 nuclei were indeterminate. The following cutoffs have been established in our laboratory: positive signal pattern in >25 cells of 50-nuclei analysis or in >15% of 100-nuclei analysis (Figure 1a).
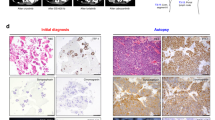
Representative positive signal patterns for ALK, RET, ROS1 rearrangement and MET amplification. (a) Tissue FISH test for ALK gene rearrangement (Case 6). Positive cells are labeled with arrows. Two positive signal patterns are present (1R1G1F indicates an ALK gene rearrangement; 1R1F indicates an ALK gene rearrangement with 5′-ALK deletion (green signal). (b) Tissue FISH test for RET gene rearrangement (Case 14). Three positive cells with a split signal pattern (1R1G1F) are labeled with arrows. (c) Tissue FISH test for ROS1 gene rearrangement (Case 6). Two positive cells with a split signal plus multiple fusion signal patterns (1R1G6~7 F) are labeled with arrows. It’s also noticed that high percentages of interphase cells exhibit either a single fusion (1F) or multiple fusion (3~8F) signal patterns. The clinical significance of these cell populations is unknown. (d) Tissue FISH test for MET gene amplification (Case 6). Three representative cells with>5 MET signals are shown.
The Clear-View FISH RET dual color, breakapart probe from CymoGen DX was applied to detect RET rearrangement (Biocare Medical, Concord, CA). The probe hybridizes to band 10q11.21 (red on the centromeric side and green on the telomeric side of the RET breakpoint). Two hundred interphase nuclei were studied for each case. The cutoff values for a positive RET rearrangement established at 95% (P<0.05) confidence level are: >7.9% for one red, one green, one fusion (1R1G1F) signal pattern (positive for RET rearrangement) and >3.1% for one green, one fusion (1G1F) signal pattern (positive for RET rearrangement with 5′ deletion). A cutoff value of >4.4% was established for one red, one fusion (1R1F) signal pattern, which indicates a positive result for 3′ deletion with unknown clinical significance (Figure 1b).
The XT ROS1 dual color, breakapart probe was used to detect ROS1 rearrangement detection (MetaSystems Group, Newton, MA). This probe hybridizes to 6q22 (red on the centromeric side and green on the telomeric side of the ROS1 breakpoint). Two hundred interphase nuclei were studied for each case. The cutoff values for a positive ROS1 rearrangement established at 95% (P<0.05) confidence level are: >3.5% for either one but not a combination of the following three signal patterns: one red, one green, one fusion (1R1G1F) signal pattern (positive for ROS1 rearrangement) and one red, one fusion (1R1F) signal pattern (positive for ROS1 rearrangement with 5′ deletion). A cutoff value of >3.5% was established for one green, one fusion (1G1F) signal pattern indicating a positive result for 3’ deletion with unknown clinical significance (Figure 1c).
The CymoGen DX MET/CC7 DNA Probe Kit was used for detection of MET amplification (Biocare Medical). The MET probe (red color) is specific for the MET locus (7q31) and CC7 probe (green color) is specific for the alpha satellite DNA sequences at the centromeric region of chromosome 7 (7p11.1-q11.1). Sixty interphase cells were studied for each case. These criteria are used for a positive MET amplification: 1). MET:CC7 ratio ≥2.0; 2). MET:CC7 ratio <2.0, but average MET signal counts in each cell ≥5; 3). Over 10% of the tumor cells showed ≥20 copies of MET signals or signal clusters (Figure 1d).
This is to point out that signal patterns of 1R1G≥2 F were frequently observed in our tissue FISH tests for ALK, RET and ROS1 rearrangement (eg, Figures 1a and c). They were considered as positive results with additional gain/amplification of an intact gene, although the clinical significance of gain/amplification of intact ALK, RET or ROS1 gene generally remains unknown.
Next-Generation DNA Sequencing for Detection of Gene Mutations
DNA was isolated from tumor tissues and targeted next-generation DNA sequencing was performed using the Ion Torrent PGM with the Ion AmpliSeq Cancer Hotspot Panel as described previously.20 Most of the cases included in this study were tested with a 50-gene hotspot panel, while the other cases were recently tested with an expanded 128-gene hotspot panel.
Results and discussion
Our laboratory has provided tissue FISH tests for ALK, RET, ROS1 rearrangement or MET amplification for patients with primary or metastatic lung cancer since February, 2010. At the end of 2016, a total of 5206 cases have been tested, of which 1251 (24%) were tested for all 4 markers, 609 (12%) for 3 markers, 768 (15%) for two markers and 2578 (50%) for one marker, respectively. The rates of a positive result are: 7% (238/3382) for ALK, 2% (32/1782) for ROS1, 1% (33/2379) for RET, and 5% (177/3398) for MET respectively, which are very similar to the prevalence of these abnormalities reported from a study of 1139 Chinese lung cancer patients21 as well as other patient populations.22 Among these positive cases, 15 (Table 1) cases were identified with concurrent rearrangement of two cancer-associated genes including ALK, RET and ROS1 and/or with MET amplification. Fourteen of these cases that were tested for all 4 genes whereas case 5 was tested for 3 markers (not RET). Therefore, the estimated dual positivity rate is 0.6% (15/2628) if cases with two or more tested markers are included or up to 1.1% (14/1251) if the cases with 4 tested markers are included in our study.
To the best of our knowledge, this is the first report showing concurrent rearrangement or amplification of ALK, RET, ROS1 or MET in lung cancer cases. As shown in Table 1, the combination of alterations exists in various forms, eg, ALK rearrangement combined with ROS1 (n=4, cases 5-8) or RET rearrangement (n=1, case 4); RET rearrangement combined with ROS1 rearrangement (n=2, cases 13 and 14); as well as MET amplification combined with ALK (n=3, cases 1-3), RET (n=4, cases 9-12) or ROS1 rearrangement (n=1, case 15). The frequency of involvement is similar for all 4 biomarkers: 53% (8/15) for both ALK and MET and 47% (7/15) for both RET and ROS1 (n=7). Interestingly, two cases (cases 9 and 10) exhibited unusual RET FISH signal patterns that have not been reported previously. In case 9, a signal pattern of 0R3~20G1~3F was detected indicating a simultaneous deletion of 5'RET and duplication/amplification of 3'RET. Lee et al23 has reported a RET rearrangement positive case with a predominant signal pattern of 1R2G1F indicating a gain of an extra copy of 3'RET, but no amplification of 3’RET. In case 10, the predominant signal pattern is 1R1G3~6F, indicating RET rearrangement with gain of multiple extra copies of an intact RET gene. The clinical significance of a RET amplification in lung cancer remains unknown, but a previous study correlated this finding with co-existence of EGFR mutations.24
In the past, mutations involving genes with tyrosine kinase function, such as EGFR, KRAS, HER2, BRAF, ALK, RET, ROS1 and MET were viewed as independent, mutually exclusive events.10 However, in recent years cases of lung cancer with coexistent alterations of EGFR and ALK or other genes have been reported by others. For example, over 20 cases of lung cancer with simultaneous alterations of EGFR and ALK or EGFR and ROS1 have been reported.16, 17, 18 Jurmeister et al has reported 3 ALK rearranged lung cancer cases that also harbored MET protein overexpression, although not MET gene amplification.25 Several research groups have reported that lung cancer patients with alterations of both EGFR and ALK have distinctive clinical characteristics and they have suggested that adding an ALK inhibitor to therapy can improve overall survival.11, 14, 15, 16 All these data therefore show the coexistence of two (or more) driver mutations in lung cancer cases and that these combinations have potential clinical implications in affected patients.3, 5, 16 The low frequency of coexistent driver mutations of two (or more) genes including ALK, RET, ROS1 and MET is likely attributable to two reasons: 1) A low incidence of ALK, RET, ROS1 rearrangement as well as MET amplification in lung cancer;21, 22 2) A change in clinical practice for patients with lung cancer has led to more rigorous testing for these genetic abnormalities. In support to the second reason, less than 25% of all lung cancer cases had been tested for all 4 markers simultaneously during the past 6 years at our center.
The demographic data for the 15 patients in this study shows a female predominance (12 women and 3 men) with a median age of 60 years (range, 43 to 81 years). Fourteen patients are Caucasians and one is an African American. Nine patients reported a smoking history (8 heavy and 1 light) and 6 patients were non-smokers. The pathological diagnosis of lung adenocarcinoma was established in these patients from 3 to 79 months (median 20 months) before FISH testing was performed. Three patients had an early-stage lung adenocarcinoma (stage I: case 6; stage II: cases 13 and 14) and 12 patients had advanced-stage lung adenocarcinoma (stage III: cases 4, 9 and 11; stage IV: all the rest cases). Therefore, a dual positivity of these 4 markers can be found in early stage lung adenocarcinoma cases. However, ALK rearrangement (7/8) and MET amplification (8/8) are mostly found in advanced stage lung adenocarcinoma cases (stage III+stage IV), whereas ROS1 and RET rearrangement are present in both early stage and advanced stage lung adenocarcinoma cases in this study (Table 2). Interestingly, 6 cases (cases 2, 6, 10, 12, 13 and 15) also had coexistent TP53 mutations; 5 cases (cases 1, 12-15) had EGFR mutations; 3 cases (cases 1, 8, 9) had KRAS mutations; and 2 cases (cases 6 and 14) had STK11 mutations detected by next-generation DNA sequencing. Although rare, all these cases demonstrate that co-alterations of tyrosine kinase function genes and tumor suppressor genes can be detected in lung adenocarcinoma cases. This phenomenon may be attributable to recurrence of disease even after an effective target-specific therapy.
All patients were treated according to stages with a combination of surgical resection, radiation therapy and therapeutic agents. Several patients received target-specific therapies, 5 with EGFR inhibitors (cases 1, 12-15), 3 with ALK inhibitors (cases 2, 5, and 7), and 3 with PD-1 inhibitors (cases 7, 8 and 12), but their clinical courses all show a temporarily partial response with local recurrence or new metastasis. One patient (case 12) is currently enrolled in a RET inhibitor trial, whereas no patients have been treated on a trial with ROS1 or MET inhibitor agents, although newly developed target-specific tyrosine kinase inhibitors may be an option during the course of their disease.4, 8, 11 At last follow up, 3 patients (cases 1, 9 and 15) died and 12 patients remain alive with partial response to their treatments.
In summary, this is the first report showing concurrent rearrangement or amplification of ALK, RET, ROS1 or MET in lung cancer cases. Several of the cases in this study also had coexistent EGFR, KRAS and/or TP53 mutations. As recommended by the 2015 World Health Organization classification of lung tumors, comprehensive molecular profiling is very important for the workup of lung cancer, and the finding of multiple molecular alterations in lung cancer may have potential clinical implications for these patients.
References
Lung and Bronchus. In: American Cancer Society. Cancer Facts & Figures 2016. American Cancer Society Inc.: Atlanta, GA, 2016, pp 13–16.
Didkowska J, Wojciechowska U, Manczuk M, Lobaszewski J . Lung cancer epidemiology: contemporary and future challenges worldwide. Ann Transl Med 2016;4:150.
Zhang J, Fujimoto J, Zhang J et al. Intratumor heterogeneity in localized lung adenocarcinomas delineated by multiregion sequencing. Science 2014;346:256–259.
Berge EM, Doebele RC . Targeted therapies in non-small cell lung cancer: emerging oncogene targets following the success of epidermal growth factor receptor. Semin Oncol 2014;41:110–125.
Travis WD, Brambilla E, Nicholson AG et al. The 2015 World Health Organization Classification of lung tumors: impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol 2015;10:1243–1260.
Vargas AJ, Harris CC . Biomarker development in the precision medicine era: lung cancer as a case study. Nat Rev Cancer 2016;16:525–537.
Subbiah V, Berry J, Roxas M et al. Systemic and CNS activity of the RET inhibitor vandetanib combined with the mTOR inhibitor everolimus in KIF5B-RET re-arranged non-small cell lung cancer with brain metastases. Lung Cancer 2015;89:76–79.
Falchook GS, Ordonez NG, Bastida CC et al. Effect of the RET Inhibitor Vandetanib in a Patient With RET Fusion-Positive Metastatic Non-Small-Cell Lung Cancer. J Clin Oncol 2016;34:e141–e144.
Shea M, Costa DB, Rangachari D . Management of advanced non-small cell lung cancers with known mutations or rearrangements: latest evidence and treatment approaches. Ther Adv Respir Dis 2016;10:113–129.
Gainor JF, Varghese AM, Ou SH et al. ALK rearrangements are mutually exclusive with mutations in EGFR or KRAS: an analysis of 1,683 patients with non-small cell lung cancer. Clin Cancer Res 2013;19:4273–4281.
Yang JJ, Zhang XC, Su J et al. Lung cancers with concomitant EGFR mutations and ALK rearrangements: diverse responses to EGFR-TKI and crizotinib in relation to diverse receptors phosphorylation. Clin Cancer Res 2014;20:1383–1392.
Won JK, Keam B, Koh J et al. Concomitant ALK translocation and EGFR mutation in lung cancer: a comparison of direct sequencing and sensitive assays and the impact on responsiveness to tyrosine kinase inhibitor. Ann Oncol 2015;26:348–354.
Cabillic F, Gros A, Dugay F et al. Parallel FISH and immunohistochemical studies of ALK status in 3244 non-small-cell lung cancers reveal major discordances. J Thorac Oncol 2014;9:295–306.
Sweis RF, Thomas S, Bank B et al. Concurrent EGFR mutation and ALK translocation in non-small cell lung cancer. Cureus 2016;8:e513.
Lou NN, Zhang XC, Chen HJ et al. Clinical outcomes of advanced non-small-cell lung cancer patients with EGFR mutation, ALK rearrangement and EGFR/ALK co-alterations. Oncotarget 2016;7:65185–65195.
Barlesi F, Mazieres J, Merlio JP et al. Routine molecular profiling of patients with advanced non-small-cell lung cancer: results of a 1-year nationwide programme of the French Cooperative Thoracic Intergroup (IFCT). Lancet 2016;387:1415–1426.
Ju L, Han M, Zhao C et al. EGFR, KRAS and ROS1 variants coexist in a lung adenocarcinoma patient. Lung Cancer 2016;95:94–97.
Zhu YC, Xu CW, Ye XQ et al. Lung cancer with concurrent EGFR mutation and ROS1 rearrangement: a case report and review of the literature. Onco Targets Ther 2016;9:4301–4305.
Mascarello JT, Hirsch B, Kearney HM et al. Section E9 of the American College of Medical Genetics technical standards and guidelines: fluorescence in situ hybridization. Genet Med 2011;13:667–675.
Goswami RS, Luthra R, Singh RR et al. Identification of factors affecting the success of next-generation sequencing testing in solid tumors. Am J Clin Pathol 2016;145:222–237.
Pan Y, Zhang Y, Li Y et al. ALK, ROS1 and RET fusions in 1139 lung adenocarcinomas: a comprehensive study of common and fusion pattern-specific clinicopathologic, histologic and cytologic features. Lung Cancer 2014;84:121–126.
Hirsch FR, Suda K, Wiens J et al. New and emerging targeted treatments in advanced non-small-cell lung cancer. Lancet 2016;388:1012–1024.
Lee SE, Lee B, Hong M et al. Comprehensive analysis of RET and ROS1 rearrangement in lung adenocarcinoma. Mod Pathol 2015;28:468–479.
Yang HS, Horten B . Gain of copy number and amplification of the RET gene in lung cancer. Exp Mol Pathol 2014;97:465–469.
Jurmeister P, Lenze D, Berg E et al. Parallel screening for ALK, MET and ROS1 alterations in non-small cell lung cancer with implications for daily routine testing. Lung Cancer 2015;87:122–129.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Tang, Z., Zhang, J., Lu, X. et al. Coexistent genetic alterations involving ALK, RET, ROS1 or MET in 15 cases of lung adenocarcinoma. Mod Pathol 31, 307–312 (2018). https://doi.org/10.1038/modpathol.2017.109
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2017.109
This article is cited by
-
Designing highly multiplex PCR primer sets with Simulated Annealing Design using Dimer Likelihood Estimation (SADDLE)
Nature Communications (2022)
-
The investigation of the healing effect of active ingredients in traditional medicinal plants on lung cancer
Medical Oncology (2020)
-
The rarity of concomitant genetic alterations in lung cancer
Modern Pathology (2018)
-
Reply to Lambros et al
Modern Pathology (2018)