Abstract
Rare cases of Merkel cell carcinoma have been encountered in lymph nodes with unknown extranodal primary, which exhibit similar morphologic and immunophenotypic features to those in primary cutaneous Merkel cell carcinomas. However, it is uncertain whether the nodal Merkel cell carcinoma is a primary tumor of the lymph node or represents a metastasis from an occult or regressed extranodal lesion. To establish an accurate diagnosis of the nodal Merkel cell carcinoma can be challenging because of significant morphologic mimics, including lymphoblastic lymphoma and metastatic small cell carcinoma. Moreover, there is no consensus for a diagnostic term, and many different terms have been used, which can be confusing and may not fully reflect the nature of nodal Merkel cell carcinoma. In this study, we investigated the detailed clinicopathologic features of 22 nodal Merkel cell carcinomas, with comparison to 763 primary cutaneous cases retrieved from the literature. Overall, the nodal and cutaneous Merkel cell carcinomas shared similar clinical presentations, morphologic spectrum, and immunophenotype; both were mostly seen in elderly male with a typical neuroendocrine morphology. Most of cases expressed CK20, synaptophysin, and chromogranin A; and PAX5 and TdT were also positive in majority of cases. However, nodal Merkel cell carcinomas had a significantly lower association with Merkel cell polyomavirus than cutaneous cases (31% vs 76%, P=0.001). Therefore, these two entities may arise from overlapping but not identical biological pathways. We also recommend the use of the diagnostic term ‘Merkel cell carcinoma of lymph node’ to replace many other names used.
Similar content being viewed by others
Main
Merkel cell carcinoma is a rare, high-grade cutaneous neuroendocrine neoplasm, which typically affects elderly white males in their 7th decade.1, 2, 3, 4 At the time of diagnosis, ∼30% of cases have metastatic diseases, mostly to regional lymph nodes and skin of other sites.2 Rare cases of high-grade neuroendocrine tumor have been encountered in the lymph nodes with unknown extranodal primary, and these tumors were often described as ‘Merkel cell carcinoma of lymph node with unknown primary’ as they exhibit similar morphologic and immunophenotypic features to those in the skin Merkel cell carcinoma.5, 6, 7, 8, 9, 10, 11, 12, 13, 14 However, it is not clear whether the nodal Merkel cell carcinoma is a primary tumor of lymph node or represents a metastasis from an occult or regressed extranodal lesion. To establish an accurate diagnosis of nodal Merkel cell carcinoma can be challenging, and it has to be separated from other nodal metastatic neoplasms, such as small cell carcinoma and lymphoblastic lymphoma. Moreover, there is no consensus of diagnosis for this entity; a number of diagnoses have been rendered, including ‘metastatic small cell carcinoma’, ‘small cell neuroendocrine carcinoma’, ‘metastatic neuroendocrine carcinoma’, ‘poorly differentiated carcinoma’, and ‘metastatic Merkel cell carcinoma of unknown primary’. These diagnoses can be confusing and may not fully reflect the nature of nodal Merkel cell carcinoma.
A new development over the past several years was the discovery of Merkel cell polyomavirus in ∼80% of cutaneous Merkel cell carcinoma.15 This virus is clonally integrated into the host genome, and is presumed to have an important role in the oncogenesis of cutaneous Merkel cell carcinoma. However, to date, the association of nodal Merkel cell carcinoma with Merkel cell polyomavirus has not been fully elucidated, and two recent studies showed controversial findings. One study demonstrated absence of Merkel cell polyomavirus in five of five primary parotid high-grade neuroendocrine carcinomas of Merkel cell type;16 and another study detected presence of Merkel cell polyomavirus in all five nodal and one parotid gland Merkel cell carcinomas.17
To further explore the issues raised above, we collected 22 cases of nodal Merkel cell carcinoma with unknown extranodal primary. The detailed clinical presentations, morphologic features, immunohistochemical stains, and Merkel cell polyomavirus status were investigated. We also studied expression of PAX5 and TdT in our cases; both markers have been detected in the majority of cutaneous Merkel cell carcinomas.18, 19, 20, 21, 22
Materials and methods
Case Selection
This study was approved by the Institutional Review Board at the City of Hope National Medical Center. The pathology files in our department from 2000 to 2011 were searched to retrieve cases of nodal Merkel cell carcinoma with an unknown extranodal primary. The cases to be accepted in our study met all of the following criteria: (1) we have carefully reviewed the detailed clinical history, image studies, and tissue biopsy diagnosis of the selected cases; and clinically, the patients did not have any cutaneous Merkel cell carcinoma or neuroendocrine tumor from other sites prior to and following the diagnosis, (2) cytologically, the tumor cells revealed neuroendocrine features with a high nucleus to cytoplasm ratio and fine chromatin, (3) immunohistochemically, the tumor cells were positive for CK20, and, for rare CK20 negative cases, reactivity for CK AE1/AE3 or CAM 5.2 was required, and (4) the tumor expressed neuroendocrine markers, including synaptophysin and/or chromogranin A. Eventually, 22 cases met all the criteria and were included in this study, including 19 cases from our institution and 3 from the outside institutions.
In addition, we attempted to compare the clinicopathologic features of our 22 nodal cases with those from the cutaneous Merkel cell carcinoma in the published data. We therefore performed an extensive literature search in the PubMed (www.ncbi.nlm.nih.gov/pubmed) with several sets of keywords, including ‘Merkel cell carcinoma’ in the ‘Title’ field, ‘Merkel cell carcinoma’ and ‘immunohistochemical’, and ‘Merkel cell polyomavirus’. The original articles were reviewed to select cases with clinical and/or pathology studies. Eventually 763 cases of cutaneous Merkel cell carcinoma were retrieved from the English literature and included in our review.15, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29
Immunohistochemical Staining
For all 22 cases, a panel of antibodies was used for an initial diagnostic workup, including CD3, CD20, CD45, CD56, chromogranin A, CK AE1/AE3, CK7, CK20, S100, synaptophysin, and TTF1. A second panel of immunostains was performed in 13 cases with additional blocks or unstained slides, including PAX5, TdT, and Merkel cell polyomavirus large T antigen. The immunostains were performed on a Dako Autostainer with Envision (+) Detection Kit (Dako, Carpinteria, CA). The expression of PAX5, TdT, and Merkel cell polyomavirus large T antigen was graded as negative (−), weakly positive (+), or strongly positive (++), whereas the expression of other antibodies was simply graded as negative (−) or positive (+). The antibody clones, dilutions, antigen retrieval methods, and manufactures were summarized in Table 1.
Merkel Cell Polyomavirus DNA Detection by Polymerase Chain Reaction (PCR)
Thirteen of 22 cases had sufficient tumor cells in the paraffin blocks or unstained slides for PCR assays. Genomic DNA was extracted using 0.4 μg/μl proteinase K in Tris-EDTA buffer. The tissue was digested at 55 °C overnight and was then boiled for 10 min before used for PCR. Two sets of primers were designed to detect MCPyV: a LT3 primer pair with a 308 base-pair PCR product (forward: 5′-TTG TCT CGC CAG CAT TGT AG-3′ and reverse: 5′-ATA TAG GGG CCT CGT CAA CC-3′) and a VP1 primer pair with a 351 base-pair PCR product (forward: 5′-TTT GCC AGC TTA CAG TGT GG-3′ and reverse: 5′-TGG ATC TAG GCC CTG ATT TTT-3′), targeting the coding regions for viral large T antigen and viral capsid protein 1, respectively. Water was used as a PCR-negative control, instead of genomic DNA, and a case of metastatic Merkel cell carcinoma with known Merkel cell polyomavirus infection was used as a positive control. PCR for ß-globin was used as an endogenous control for quality and load of genomic DNA (PCR product 268 base-pair, forward primer 5′-GAA GAG CCA AGG ACA GGT AC-3′, and reverse primer 5′-CAA CTT CAT CCA CGT TCA CC-3′). The PCR assays were carried out on a GeneAmp® PCR System 9700 (Applied Biosystems, Carlsbad, CA). The amplification reactions for all target DNA regions were performed in a reaction volume of 30 μl with the following conditions: initial denaturing at 95 °C for 15 min, then denaturing at 95 °C for 30 s followed by annealing at 58 °C for 30 s and extension at 72 °C for 30 s, 45 cycles, and final extension for 30 min at 72 °C. The amplified products were electrophoresed in a 2% agarose gel.
Results
Clinical Information
For the 22 cases in our study, a number of diagnostic terms had been used by outside institutions, as discussed in the introduction section. In most of the cases, the tumor was considered as a metastatic carcinoma of unknown origin, particularly metastatic Merkel cell carcinoma. However, none of the 22 patients had any history of primary cutaneous Merkel cell carcinoma prior to the diagnosis. Extensive physical and radiological investigations also did not discover any extranodal primary or any signs of regressed lesion after the diagnosis. Nineteen patients were followed up closely, and none of them developed any cutaneous Merkel cell carcinoma with an average interval of 24.3 months, ranging from 2 to 140 months.
The major clinical features for the 22 patients were summarized in Table 2. There was a male predominance with a male-to-female ratio of 4.5:1 (18 males and 4 females). The mean age was 65.2 years, ranging from 48 to 92 years. The tumors often involved the head and neck lymph nodes (nine cases, including cervical, intraparotid, submandibular, and supraclavicular), inguinal (eight), and axillary (five). The greatest dimension of lymph nodes was available in 17 patients, with a mean size of 6.0 cm. Particularly in the inguinal region, the lymph nodes were often bulky with a mean size of 10.8 cm (eight cases, ranging from 4.5 to 27 cm). Eight patients also presented with other aggressive or systemic tumors, excluding localized basal cell carcinoma, which included pulmonary adenosquamous carcinoma in case 3, colon cancer and urothelial carcinoma in case 9, laryngeal squamous cell carcinoma in case 13, multiple poorly differentiated head/neck squamous cell carcinomas in case 14, and metastatic renal cell carcinoma in case 22. Interestingly, three patients (cases 6, 11, and 16) also had chronic lymphocytic leukemia/small lymphocytic lymphoma prior to the diagnosis of nodal Merkel cell carcinoma. In most of the cases, nodal Merkel cell carcinoma was usually confined to the regional lymph nodes without involvement of extranodal organs despite the bulky lesions. In cases 5 and 15, the tumors disseminated into other regional lymph nodes without extranodal involvement in the fashion similar to that of lymphomas. The patient in case 10 developed brain metastasis from Merkel cell carcinoma, and the patient in case 11 showed possible liver metastasis, but the diagnosis was not confirmed by tissue biopsy.
Five patients received regional lymph node dissection in combination with local radiotherapy and chemotherapy, and other treatment plans included radiotherapy and surgery (2 patients), surgery only (4), and chemotherapy only (6). Of the 19 patients with follow-up, most had good response to the treatments and remained stable and tumor-free. Two patients died of metastatic Merkel cell carcinoma to multiple lymph node regions or to the brain, and 2 other patients died of aggressive squamous cell carcinoma in the head/neck region.
Gross and Histopathologic Features
Grossly, the lymph nodes in most cases were markedly enlarged with entire replacement by the tumor, and large areas of degeneration and necrosis were often present, particularly in the center of the specimen (Figure 1a). Microscopically, the 22 cases of nodal Merkel cell carcinoma displayed a broad morphologic spectrum. Architecturally, there were several identifiable patterns: (1) sheets of growth pattern with geographic necrosis (Figure 1b), (2) solid nests, cords, and organoid arrangements (Figure 1c), (3) occasionally solid nests divided by delicate fibrovascular septa (Figure 1d), and (4) rarely diffuse infiltration, closely mimicking a hematologic neoplasm (Figures 1e and f). Cytologically, the tumor cells in most cases were medium to large in size and had a high nucleus to cytoplasm ratio with scant amounts of cytoplasm. The nuclei were round to oval and had characteristic fine, ‘salt-and-pepper’ chromatin with small or inconspicuous nucleoli (Figure 1c). In a few cases, the tumor cells revealed powdery or watery chromatin and small nucleoli, a finding which was unique to Merkel cell carcinoma (Figure 1d). One case closely resembled lymphoblastic lymphoma, which was composed of diffuse, monotonous small cells with scant cytoplasm and round nuclei with dense but fine chromatin (Figure 1e). The tumor cells in two cases closely mimicked lymphoma of mature lymphocytes, with a diffuse infiltrative pattern, condensed chromatin, visible nucleoli, and moderate amount of cytoplasm, in contrast to the majority of other cases (Figure 1f).
Gross image and morphologic features of nodal Merkel cell carcinoma. (a) A markedly enlarged lymph node with complete replacement by tumor and central necrosis. (b) Sheets of growth pattern and geographic necrosis (Hematoxylin & eosin, 4 × ). (c) Nested and organoid arrangements; and the tumor cells have round to oval nuclei with fine chromatin and inconspicuous nucleoli (Hematoxylin & eosin, 10 × ). (d) Nested growth pattern with delicate fibrovascular septa; and the tumor cells exhibit powdery or watery chromatin, which is diagnostic for Merkel cell carcinoma (Hematoxylin & eosin, 20 × ). (e) Diffuse infiltration by small, monotonous tumor cells, resembling lymphoblastic lymphoma (Hematoxylin & eosin, 4 × ). (f) Diffuse infiltration by large tumor cells, mimicking a large cell lymphoma (Hematoxylin & eosin, 10 × ).
Despite the significant morphologic variations, the tumors in our study generally shared typically neuroendocrine features, which were superimposable to those seen in cutaneous Merkel cell carcinoma. However, none of our 22 cases showed any squamous differentiation or differentiation to skin adnexal structures, which can be occasionally seen in cutaneous Merkel cell carcinomas. One of the three cases with history of chronic lymphocytic leukemia/small lymphocytic lymphoma showed concurrent Merkel cell carcinoma and chronic lymphocytic leukemia/small lymphocytic lymphoma in the same lymph node.
Immunohistochemistry
CK AE1/AE3 was stained in 19 cases, all of which (100%) showed diffuse and strong positivity. CK20 was positive in 20 of 22 cases (91%) with characteristic perinuclear ‘dot-like’ staining in most (Figure 2a). Three of 22 cases (14%) expressed CK7, with two cases co-expressing CK20. One case (case 3) only expressed CK AE1/AE3 but neither CK7 nor CK20. Synaptophysin was positive in 19 of 19 cases (100%) stained, whereas chromogranin was detected in 13 of 19 cases (68%) (Figures 2b and c). TTF1 immunostain was performed in 21 cases, none of which showed any reactivity. All of the cases were negative for selected lymphoid markers, including CD3 (0/8), CD20 (0/10), and CD45 (0/8).
Immunostains for TdT, PAX5, and Merkel cell polyomavirus large T antigen were also performed in the cases with additional tissue available. Ten of 13 (77%) cases were TdT positive (6 cases with strong staining and 4 weak). The TdT staining pattern was mostly heterogeneous even in the cases with strong positivity (Figure 3a), with strong and diffuse reactivity in only one case (Figure 3b). PAX5 was positive in 8 of 13 cases (62%, 2 moderate and 6 weak) (Figure 3c). The Merkel cell polyomavirus large T antigen was detected in 3 of 13 cases (23%; cases 10, 12, and 13) using the antibody CM2B4, with diffuse and strong nuclear staining (Figure 3d).
Immunohistochemical staining of nodal Merkel cell carcinoma. (a) An example of strong positivity for TdT but with heterogeneous staining (20 × ). (b) A case with strong and homogenous positivity for TdT (20 × ). (c) A case with moderate staining for PAX5, and the background reactive B cells showing strong positivity (20 × ). (d) An example with strong and nuclear reactivity for Merkel cell polyomavirus large T antigen (40 × ).
Detection of Merkel Cell Polyomavirus DNA
PCR assays were performed in 13 cases to detect the presence of Merkel cell polyomavirus. Two sets of primer pairs, LT3 and VP1, were used to cover the coding regions for Merkel cell polyomavirus large T antigen and viral capsid protein 1, respectively. The PCR assays with the LT3 primer pair detected viral DNA in four cases (cases 8, 10, 12, and 13), whereas three cases (cases 8, 10, and 13) were positive for viral DNA using the VP1 primer pair (Figure 4).
Discussion
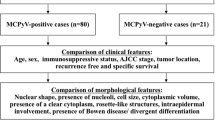
Nodal Merkel Cell Carcinoma Shows Similar Clinical Features and Nearly Identical Morphology and Immunophenotype to Its Cutaneous Counterpart
The clinicopathologic features of our 22 nodal cases were compared with the 763 cases of primary cutaneous Merkel cell carcinoma from the English literature (Tables 3 and 4). Clinically, both entities mostly affected elderly males. Eight of our 22 patients (36%) also had other aggressive or systemic tumors, which is close to that in cutaneous Merkel cell carcinoma (27%).30, 31, 32 Histologically, our cases generally displayed similar morphologic spectrum to the cutaneous Merkel cell carcinoma; however, none of our cases were associated with any non-neuroendocrine differentiation, including squamous cell, basal cell or skin adnexal structure, which can be occasionally seen in cutaneous Merkel cell carcinomas.33 The skin and nodal Merkel cell carcinomas also showed a nearly identical immunoprofile; most of cases expressed CK20, synaptophysin, chromogranin A, PAX5, and TdT, whereas very few expressed CK7 and TTF1. The only significant finding was that the nodal Merkel cell carcinoma had a significantly lower association with Merkel cell polyomavirus than the cutaneous Merkel cell carcinoma (31% vs 76%, P=0.001).
In our study, the patients generally had good response to the treatment and most of them remained tumor-free. One recent study revealed that the nodal Merkel cell carcinoma with an unknown extranodal primary had a lower recurrence rate and a less-aggressive clinical course, compared with the cutaneous Merkel cell carcinoma with nodal metastasis, with a median overall survival of ∼104 months in the nodal cases.34 Another more recently published study showed that the overall 2-year survival of nodal Merkel cell carcinoma patients was significantly improved vs matched stage IIIB cutaneous Merkel cell carcinoma (76.9–36.4%).35
Possible Histogenesis of Nodal Merkel Cell Carcinoma
Currently, it is still not certain whether the ‘nodal Merkel cell carcinoma’ is truly a primary tumor of lymph node or not. Nineteen of our 22 patients were followed up closely, and none of them developed any cutaneous Merkel cell carcinoma within an average interval of 24.3 months. It is hard to imagine that the occult primary tumors would have remained undetectable after such a long period of time, given that Merkel cell carcinoma is a very aggressive and fast-growing tumor. Regression of cutaneous Merkel cell carcinoma and nodal metastasis has rarely been reported, mostly after either surgical excision or needle biopsy of the primary lesion; and it was thought to be due to the procedures, which stimulated cell-mediated immune clearance of the residual tumor cells.36, 37, 38, 39, 40, 41, 42, 43, 44 It is difficult to envision the spontaneous resolution of cutaneous Merkel cell carcinoma without prior medical intervention in all of our cases; moreover, it is very unlikely that all the primary tumors would have regressed without leaving any visible remnants. Therefore, we speculate that some of our nodal cases may represent primary nodal neoplasms.
Others have proposed that the ‘primary’ nodal Merkel cell carcinoma could be the result of malignant transformation from pre-existing intranodal epithelial nests or pluripotent epidermal stem cells. Development of cutaneous Merkel cell carcinoma may be related to ultraviolet light irradiation and immunosupression.45, 46, 47, 48 In our study, 8 of 22 (36%) patients had a history of other aggressive or systemic tumors prior to the diagnosis of nodal Merkel cell carcinoma, and 3 of them had chronic lymphocytic leukemia/small lymphocytic lymphoma. Approximately 27% of patients with cutaneous Merkel cell carcinoma had other invasive non-Merkel cell carcinoma malignancies, with chronic lymphocytic leukemia/small lymphocytic lymphoma the most common one, accounting for 45% of all tumors.30, 31, 32
The discovery of Merkel cell polyomavirus in cutaneous Merkel cell carcinoma may also at least partially account for the infectious etiology in the pathogenesis of Merkel cell carcinoma.15 It has been proven to function in the Merkel cell carcinoma oncogenesis through integration into the host genomic DNA.15 However, we only detected Merkel cell polyomavirus in 4 of 13 cases (31%), which is significantly lower than that in the cutaneous cases. The lower expression of Merkel cell polyomavirus in the nodal Merkel cell carcinoma is not likely due to antigen loss during ‘metastasis’; studies have shown the same frequency and pattern of Merkel cell polyomavirus large T-antigen expression in the paired nodal metastases and corresponding primary cutaneous tumors.29 Recently, one study demonstrated absence of Merkel cell polyomavirus in five cases of primary parotid high-grade neuroendocrine carcinoma of Merkel cell type.16 In contrast, another study revealed Merkel cell polyomavirus in all five nodal and one intraparotid Merkel cell carcinomas with PCR assays alone. In 2012, Rodig et al.17 was able to detect the presence of Merkel cell polyomavirus in nearly all cutaneous Merkel cell carcinomas using a novel monoclonal antibody (Ab3) and quantitative PCR.49 The increased sensitivity of detection is likely related to shorter amplicons of PCR reactions, more primer sets, and utilization of quantitative PCR, which is more sensitive than the agarose-gel-based detection method.
Differential Diagnosis of Nodal Merkel Cell Carcinoma
To establish an accurate diagnosis of nodal Merkel cell carcinoma can be challenging due to lack of cutaneous presentation and presence of a broad morphologic spectrum. The application of needle core biopsies often constrains pathologists with limited amounts of tissue. A unique morphologic feature of nodal Merkel cell carcinoma is the powdery and watery chromatin, which is virtually diagnostic of Merkel cell carcinoma. A number of metastatic tumors must also be considered in the differential diagnosis, including metastatic neuroendocrine carcinoma from the lung or genitourinary tract, small cell melanoma, B-cell lymphoblastic lymphoma, and mature B-cell lymphoma. Nodal Merkel cell carcinoma often has morphologic features indistinguishable from pulmonary small cell carcinoma. However, pulmonary small cell carcinoma typically presents with a mass lesion in the lung, and the tumor cells are positive for TTF1 but not CK20 and Merkel cell polyomavirus. Small cell carcinoma from the urinary bladder and prostate usually does not express CK20, but TTF1 can be positive in 52–83% of cases.50, 51, 52 The distinction between nodal Merkel cell carcinoma and small cell melanoma is usually straightforward as melanoma cells express S100 and other melanocytic markers (HMB45, MITF, and MART1).
The distinction between nodal Merkel cell carcinoma and hematologic malignancies is not a problem in most cases as Merkel cell carcinoma often forms cohesive solid nests. However, it can be difficult in occasional cases with a diffuse growth pattern. The small cell variant of nodal Merkel cell carcinoma closely resembles B-cell lymphoblastic lymphoma (Figure 1e). Significantly, most cases of Merkel cell carcinoma express PAX5 and TdT, which could be a pitfall together with the absence of CD20. However, both PAX5 and TdT in Merkel cell carcinomas usually show heterogeneous stains, in contrast to the strong and diffuse pattern in B-cell lymphoblastic lymphoma. On occasion, nodal Merkel cell carcinoma may show nonclassic morphologic findings with a diffuse growth pattern, simulating the appearance of a mature large cell lymphoma. Interestingly, nodal Merkel cell carcinoma may disseminate to different regional lymph nodes (eg, axillary and inguinal) in the fashion similar to that of lymphomas.
Therefore, for any tumor in the lymph node with a neuroendocrine appearance, a careful review of the patient’s medical records and communication with the referral physician are necessary to eliminate the possibility of a metastasis from a cutaneous Merkel cell carcinoma. An initial battery of immunostains should include pan-CK, CK7, CK20, TTF1, chromogranin A, synaptophysin, and S100 to rule out a metastatic neuroendocrine carcinoma or melanoma. In some cases, lymphoid markers (CD45, CD3, and CD20) may be necessary to rule out a lymphoma. If PAX5 and TdT are used, the stains should be interpreted cautiously in the context of other immunostains. After excluding the possibility of metastasis from a primary extranodal tumor, we recommend diagnosis of ‘Merkel cell carcinoma of lymph node’ or ‘high-grade neuroendocrine carcinoma of lymph node, favoring Merkel cell carcinoma’. A comment in the final report is necessary to briefly explain the nature of this tumor and to recommend systemic clinical workup and close follow-up to rule out metastasis.
Conclusions
In summary, our findings showed that the nodal and cutaneous Merkel cell carcinomas shared similar clinical presentations (excluding the location, obviously), morphologic spectrum, and immunophenotype. However, nodal Merkel cell carcinoma had a significantly lower association with Merkel cell polyomavirus; therefore, these two entities may arise from overlapping but not identical biological pathways. However, the exact etiology of the nodal Merkel cell carcinoma is still unclear. We also recommend use of the diagnostic term ‘Merkel cell carcinoma of lymph node’ to replace many other names used.
References
Toker C . Trabecular carcinoma of the skin. Arch Dermatol 1972;105:107–110.
Allen PJ, Bowne WB, Jaques DP et al. Merkel cell carcinoma: prognosis and treatment of patients from a single institution. J Clin Oncol 2005;23:2300–2309.
Agelli M, Clegg LX . Epidemiology of primary merkel cell carcinoma in the united states. J Am Acad Dermatol 2003;49:832–841.
Heath M, Jaimes N, Lemos B et al. Clinical characteristics of merkel cell carcinoma at diagnosis in 195 patients: The AEIOU features. J Am Acad Dermatol 2008;58:375–381.
Eusebi V, Capella C, Cossu A et al. Neuroendocrine carcinoma within lymph nodes in the absence of a primary tumor, with special reference to merkel cell carcinoma. Am J Surg Pathol 1992;16:658–666.
Wong KK, Oliver GF . Metastatic merkel cell carcinoma with an unknown primary tumour presenting as lichenoid dermatitis. Australas J Dermatol 2010;51:202–205.
Straka JA, Straka MB . A review of merkel cell carcinoma with emphasis on lymph node disease in the absence of a primary site. Am J Otolaryngol 1997;18:55–65.
Nazarian Y, Shalmon B, Horowitz Z et al. Merkel cell carcinoma of unknown primary site. J Laryngol Otol 2007;121:e1.
Kim EJ, Kim HS, Kim HO et al. Merkel cell carcinoma of the inguinal lymph node with an unknown primary site. J Dermatol 2009;36:170–173.
Huber GF, Khalil M, Falck V et al. Merkel cell carcinoma with solitary parotid metastasis: diagnostic dilemma in the absence of a primary site. J Otolaryngol Head Neck Surg 2008;37:E19–E21.
Fotia G, Barni R, Bellan C et al. Lymph nodal merkel cell carcinoma: primary or metastatic disease? a clinical case. Tumori 2002;88:424–426.
De Cicco L, Vavassori A, Jereczek-Fossa BA et al. Lymph node metastases of merkel cell carcinoma from unknown primary site: report of three cases. Tumori 2008;94:758–761.
Cozzolino I, Zeppa R, Zeppa P . Lymph nodal merkel cell carcinoma: primary tumor or metastasis from unknown primary site? J Cutan Pathol 2011;38:836–837.
Boghossian V, Owen ID, Nuli B et al. Neuroendocrine (merkel cell) carcinoma of the retroperitoneum with no identifiable primary site. World J Surg Oncol 2007;5:117.
Feng H, Shuda M, Chang Y et al. Clonal integration of a polyomavirus in human merkel cell carcinoma. Science 2008;319:1096–1100.
Chernock RD, Duncavage EJ, Gnepp DR et al. Absence of merkel cell polyomavirus in primary parotid high-grade neuroendocrine carcinomas regardless of cytokeratin 20 immunophenotype. Am J Surg Pathol 2011;35:1806–1811.
de Biase D, Ragazzi M, Asioli S et al. Extracutaneous merkel cell carcinomas harbor polyomavirus DNA. Hum Pathol 2012;43:980–985.
Buresh CJ, Oliai BR, Miller RT . Reactivity with TdT in merkel cell carcinoma: a potential diagnostic pitfall. Am J Clin Pathol 2008;129:894–898.
Sidiropoulos M, Hanna W, Raphael SJ et al. Expression of TdT in merkel cell carcinoma and small cell lung carcinoma. Am J Clin Pathol 2011;135:831–838.
Sur M, AlArdati H, Ross C et al. TdT expression in merkel cell carcinoma: potential diagnostic pitfall with blastic hematological malignancies and expanded immunohistochemical analysis. Mod Pathol 2007;20:1113–1120.
Mhawech-Fauceglia P, Saxena R, Zhang S et al. Pax-5 immunoexpression in various types of benign and malignant tumours: a high-throughput tissue microarray analysis. J Clin Pathol 2007;60:709–714.
Dong HY, Liu W, Cohen P et al. B-cell specific activation protein encoded by the PAX-5 gene is commonly expressed in merkel cell carcinoma and small cell carcinomas. Am J Surg Pathol 2005;29:687–692.
Bobos M, Hytiroglou P, Kostopoulos I et al. Immunohistochemical distinction between merkel cell carcinoma and small cell carcinoma of the lung. Am J Dermatopathol 2006;28:99–104.
Llombart B, Monteagudo C, Lopez-Guerrero JA et al. Clinicopathological and immunohistochemical analysis of 20 cases of merkel cell carcinoma in search of prognostic markers. Histopathology 2005;46:622–634.
Fields RC, Busam KJ, Chou JF et al. Five hundred patients with merkel cell carcinoma evaluated at a single institution. Ann Surg 2011;254:465 73; discussion 473-475.
Andres C, Belloni B, Puchta U et al. Prevalence of MCPyV in merkel cell carcinoma and non-MCC tumors. J Cutan Pathol 2010;37:28–34.
Busam KJ, Jungbluth AA, Rekthman N et al. Merkel cell polyomavirus expression in merkel cell carcinomas and its absence in combined tumors and pulmonary neuroendocrine carcinomas. Am J Surg Pathol 2009;33:1378–1385.
Sihto H, Kukko H, Koljonen V et al. Clinical factors associated with merkel cell polyomavirus infection in merkel cell carcinoma. J Natl Cancer Inst 2009;101:938–945.
Ly TY, Walsh NM, Pasternak S . The spectrum of merkel cell polyomavirus expression in merkel cell carcinoma, in a variety of cutaneous neoplasms, and in neuroendocrine carcinomas from different anatomical sites. Hum Pathol 2012;43:557–566.
Tadmor T, Liphshitz I, Aviv A et al. Increased incidence of chronic lymphocytic leukaemia and lymphomas in patients with merkel cell carcinoma – a population based study of 335 cases with neuroendocrine skin tumour. Br J Haematol 2012;157:457–462.
Khezri F, Brewer JD, Weaver AL . Merkel cell carcinoma in the setting of chronic lymphocytic leukemia. Dermatol Surg 2011;37:1100–1105.
Koljonen V, Kukko H, Pukkala E et al. Chronic lymphocytic leukaemia patients have a high risk of merkel-cell polyomavirus DNA-positive merkel-cell carcinoma. Br J Cancer 2009;101:1444–1447.
Gould E, Albores-Saavedra J, Dubner B et al. Eccrine and squamous differentiation in merkel cell carcinoma. an immunohistochemical study. Am J Surg Pathol 1988;12:768–772.
Deneve JL, Messina JL, Marzban SS et al. Merkel cell carcinoma of unknown primary origin. Ann Surg Oncol 2012;19:2360–2366.
Tarantola TI, Vallow LA, Halyard MY et al. Unknown primary merkel cell carcinoma: 23 new cases and a review. J Am Acad Dermatol 2013;68:433–440.
Wooff JC, Trites JR, Walsh NM et al. Complete spontaneous regression of metastatic merkel cell carcinoma: a case report and review of the literature. Am J Dermatopathol 2010;32:614–617.
Connelly T . Regarding complete spontaneous regression of merkel cell carcinoma. Dermatol Surg 2009;35:721.
Ciudad C, Aviles JA, Alfageme F et al. Spontaneous regression in merkel cell carcinoma: Report of two cases with a description of dermoscopic features and review of the literature. Dermatol Surg 2010;36:687–693.
Connelly TJ, Cribier B, Brown TJ et al. Complete spontaneous regression of merkel cell carcinoma: a review of the 10 reported cases. Dermatol Surg 2000;26:853–856.
Karkos PD, Sastry A, Hampal S et al. Spontaneous regression of merkel cell carcinoma of the nose. Head Neck 2010;32:411–414.
Richetta AG, Mancini M, Torroni A et al. Total spontaneous regression of advanced merkel cell carcinoma after biopsy: review and a new case. Dermatol Surg 2008;34:815–822.
Sais G, Admella C, Soler T . Spontaneous regression in primary cutaneous neuroendocrine (merkel cell) carcinoma: a rare immune phenomenon? J Eur Acad Dermatol Venereol 2002;16:82–83.
Val-Bernal JF, Garcia-Castano A, Garcia-Barredo R et al. Spontaneous complete regression in merkel cell carcinoma after biopsy. Adv Anat Pathol 2011;18:7 author reply 177.
Yagi Y, Fujisawa A, Makiura M et al. Spontaneous regression of merkel cell carcinoma after biopsy. J Dermatol 2009;36:312–313.
Lunder EJ, Stern RS . Merkel-cell carcinomas in patients treated with methoxsalen and ultraviolet A radiation. N Engl J Med 1998;339:1247–1248.
Engels EA, Frisch M, Goedert JJ et al. Merkel cell carcinoma and HIV infection. Lancet 2002;359:497–498.
Stoff B, Salisbury C, Parker D et al. Dermatopathology of skin cancer in solid organ transplant recipients. Transplant Rev (Orlando) 2010;24:172–189.
Tadmor T, Aviv A, Polliack A . Merkel cell carcinoma, chronic lymphocytic leukemia and other lymphoproliferative disorders: an old bond with possible new viral ties. Ann Oncol 2011;22:250–256.
Rodig SJ, Cheng J, Wardzala J et al. Improved detection suggests all merkel cell carcinomas harbor merkel polyomavirus. J Clin Invest 2012;122:4645–4653.
Alijo Serrano F, Sanchez-Mora N, Angel Arranz J et al. Large cell and small cell neuroendocrine bladder carcinoma: immunohistochemical and outcome study in a single institution. Am J Clin Pathol 2007;128:733–739.
Wang W, Epstein JI . Small cell carcinoma of the prostate. A morphologic and immunohistochemical study of 95 cases. Am J Surg Pathol 2008;32:65–71.
Yao JL, Madeb R, Bourne P et al. Small cell carcinoma of the prostate: An immunohistochemical study. Am J Surg Pathol 2006;30:705–712.
Acknowledgements
The authors thank Lisa Litzenberger (Department of Pathology, University of Colorado Anschutz Medical Campus, Aurora, CO) for her expert assistance in assembling the digital figures in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Pan, Z., Chen, YY., Wu, X. et al. Merkel cell carcinoma of lymph node with unknown primary has a significantly lower association with Merkel cell polyomavirus than its cutaneous counterpart. Mod Pathol 27, 1182–1192 (2014). https://doi.org/10.1038/modpathol.2013.250
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2013.250
Keywords
This article is cited by
-
Clinical-Pathological Evaluation and Prognostic Analysis of 228 Merkel Cell Carcinomas Focusing on Tumor-Infiltrating Lymphocytes, MCPYV Infection and ALK Expression
Endocrine Pathology (2022)
-
Diagnostic accuracy of a panel of immunohistochemical and molecular markers to distinguish Merkel cell carcinoma from other neuroendocrine carcinomas
Modern Pathology (2019)
-
Update from the 4th Edition of the World Health Organization Classification of Head and Neck Tumours: What Is New in the 2017 WHO Blue Book for Tumors and Tumor-Like Lesions of the Neck and Lymph Nodes
Head and Neck Pathology (2017)