Abstract
Objective:
To assess frequency of very low birth weight (VLBW) births at non-level III hospitals.
Study Design:
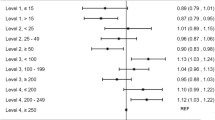
Retrospective cohort study using linked California birth certificate and discharge data of 2008 to 2010 for deliveries of singleton or first-born infant of multiple gestations with birth weight 400 to 1500 g. Delivery rates by neonatal level of care were obtained. Risk of delivery at non-level III centers was estimated in univariable and multivariable models.
Results:
Of the 1 508 143 births, 13 919 (9.2%) were VLBW; birth rate at non-level III centers was 14.9% (8.4% in level I and 6.5% in level II). Median rate of VLBW births was 0.3% (range 0 to 4.7%) annually at level I and 0.5% (range 0 to 1.6%) at level II hospitals. Antepartum stay for >24 h occurred in 14.0% and 26.9% of VLBW births in level I and level II hospitals, respectively.
Conclusion:
Further improvement is possible in reducing VLBW infant delivery at suboptimal sites, given the window of opportunity for many patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Berns SD (ed). Toward Improving the Outcome of Pregnancy III: Enhancing Perinatal Health Through Quality, Safety and Performance Initiatives. Reissued edition. March of Dimes Foundation: White Plains, NY, 2011.
Ryan GM . Toward improving the outcome of pregnancy: recommendations for the regional development of perinatal health services. Obstet Gynecol 1975; 46 (4): 375–384.
Chien LY, Whyte R, Aziz K, Thiessen P, Matthew D, Lee SK et al. Improved outcome of preterm infants when delivered in tertiary care centers. Obstet Gynecol 2001; 98 (2): 247–252.
Menard MK, Liu Q, Holgren EA, Sappenfield WM . Neonatal mortality for very low birth weight deliveries in South Carolina by level of hospital perinatal service. Am J Obstet Gynecol 1998; 179 (2): 374–381.
Stark AR, American Academy of Pediatrics Committee on Fetus and Newborn. Levels of neonatal care. Pediatrics 2004; 114 (5): 1341–1347.
Modanlou HD, Dorchester WL, Thorosian A, Freeman RK . Antenatal versus neonatal transport to a regional perinatal center: a comparison between matched pairs. Obstet Gynecol 1979; 53 (6): 725–729.
Kollée LA, Eskes TK, Peer PG, Koppes JF . Intra- or extrauterine transport? Comparison of neonatal outcomes using a logistic model. Eur J Obstet Gynecol Reprod Biol 1985; 20 (6): 393–399.
Kollée LA, Brand R, Schreuder AM, Ens-Dokkum MH, Veen S, Verloove-Vanhorick SP . Five-year outcome of preterm and very low birth weight infants: a comparison between maternal and neonatal transport. Obstet Gynecol 1992; 80 (4): 635–638.
Hohlagschwandtner M, Husslein P, Klebermass K, Weninger M, Nardi A, Langer M . Perinatal mortality and morbidity. Comparison between maternal transport, neonatal transport and inpatient antenatal treatment. Arch Gynecol Obstet 2001; 265 (3): 113–118.
U.S. Department of Health and Human Services. https://www.healthypeople.gov/2020/topics-objectives/objective/mich-33. Accessed 7 August 2016.
American Academy of Pediatrics Committee on Fetus and Newborn. Levels of neonatal care. Pediatrics 2012; 130 (3): 587–597.
Stark AR . Levels of neonatal care. Pediatrics 2004; 114 (5): 1341–1347.
Gould JB, Sarnoff R, Liu H, Bell DR, Chavez G . Very low birth weight births at non-NICU hospitals: the role of sociodemographic, perinatal, and geographic factors. J Perinatol 1999; 19 (3): 197–205.
Chung JH, Phibbs CS, Boscardin WJ, Kominski GF, Ortega AN, Needleman J . The effect of neonatal intensive care level and hospital volume on mortality of very low birth weight infants. Med Care 2010; 48 (7): 635–644.
Phibbs CS, Baker LC, Caughey AB, Danielsen B, Schmitt SK, Phibbs RH . Level and volume of neonatal intensive care and mortality in very-low-birth-weight infants. N Engl J Med 2007; 356 (21): 2165–2175.
Kastenberg ZJ, Lee HC, Profit J, Gould JB, Sylvester KG . Effect of deregionalized care on mortality in very low-birth-weight infants with necrotizing enterocolitis. JAMA Pediatr 2015; 169 (1): 26–32.
Lorch SA, Baiocchi M, Ahlberg CE, Small DS . The differential impact of delivery hospital on the outcomes of premature infants. Pediatrics 2012; 130 (2): 270–278.
Lorch SA . Ensuring access to the appropriate health care professionals: regionalization and centralization of care in a new era of health care financing and delivery. JAMA Pediatr 2015; 169 (1): 11–12.
Bowman E, Doyle LW, Murton LJ, Roy RN, Kitchen WH . Increased mortality of preterm infants transferred between tertiary perinatal centres. BMJ 1988; 297 (6656): 1098–1100.
American College of Obstetricians and Gynecologists and Society for Maternal–Fetal Medicine American College of Obstetricians and Gynecologists and Society for Maternal–Fetal Medicine, Menard MK American College of Obstetricians and Gynecologists and Society for Maternal–Fetal Medicine, Kilpatrick S American College of Obstetricians and Gynecologists and Society for Maternal–Fetal Medicine, Saade G et al, Hollier LM, Joseph GF Jr, Barfield W Levels of maternal care. Am J Obstet Gynecol 2015; 212 (3): 259–271.
Acknowledgements
We are thankful for the support from the Med Scholars Program of Stanford University School of Medicine (Diana Robles). The project described was supported by Grant K23HD068400 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health and Human Development or the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Robles, D., Blumenfeld, Y., Lee, H. et al. Opportunities for maternal transport for delivery of very low birth weight infants. J Perinatol 37, 32–35 (2017). https://doi.org/10.1038/jp.2016.174
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.174
This article is cited by
-
Survival of infants with congenital diaphragmatic hernia in California: impact of hospital, clinical, and sociodemographic factors
Journal of Perinatology (2020)
-
Prevalence and Predictors of Back-Transport Closer to Maternal Residence After Acute Neonatal Care in a Regional NICU
Maternal and Child Health Journal (2019)