Abstract
MRG15 is a recently identified member of the BRCA multiprotein complex, essential for the maintenance of the genome integrity and DNA repair. The functional relationship between PALB2 and MRG15 makes MRG15 a strong candidate breast cancer susceptibility gene. We screened affected probands from 232 BRCA1/2-negative breast cancer families for mutations in MRG15. We identified seven previously unreported variants but in silico analyses revealed that none of these variants appears to modify the function of MRG15. Thus, it seems unlikely that any constitutional changes in MRG15 confer an increased risk for breast cancer.
Similar content being viewed by others
Description
Proteins encoded by the breast cancer susceptibility genes BRCA1 and BRCA2 and their partners form several networks.1 One such protein complex is responsible for the maintenance of the genome by repairing damaged DNA and preventing harmful gene rearrangements.2, 3 Deleterious germ-line mutations in BRCA1 and BRCA2 are mainly associated with increased risks for breast and ovarian cancers, but pancreas and prostate cancers are also observed at increased frequency in BRCA2 carriers. Nonetheless, most cases of these cancers are not attributable to mutations in these genes. To date, known protein partners of BRCA1 and BRCA2 have been investigated to determine possible associations between their genetic variants and an increase in the risk of developing cancers.4 One example is PALB2, which interacts with both BRCA1 and BRCA2 proteins, and multiple different constitutional mutations have been found to be associated with an elevated risk of breast and pancreatic cancers.5, 6, 7 These and other studies show the importance of investigating additional genes from the BRCA network as potential breast cancer susceptibility genes.
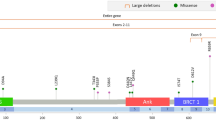
Recently, MRG15 (also known as MORF4L1), a new BRCA complex-interacting protein, has been characterized. It participates in the response to double-strand breaks by recruiting the BRCA complex to sites of damaged DNA.8 MRG15 is encoded by a gene located on 15q24. It is a 41.5 kDa chromodomain protein that directly binds to PALB2.9 This interaction is essential for homologous recombination regulation during DNA repair. This functional relationship with PALB2 means that MRG15 is a candidate breast cancer susceptibility gene. Consequently, we have formally investigated this hypothesis by screening germ-line DNA from a set of BRCA1/2 mutation-negative breast cancer cases for potential cancer-related genetic alterations.
Approval to perform the study was obtained from the local ethical review boards. DNA from blood of affected index cases of 232 breast or breast/ovarian cancer families was screened for MRG15 mutations. All families were negative for the relevant BRCA1/2 founder mutations in the Finnish (n=148), French-Canadian (n=45) and Ashkenazi Jewish groups (n=9) and/or were negative for BRCA1/2 mutations by full sequencing. The average age at diagnosis of the index case was 48.12 years (range 19–89 years) and 225 of 232 (97%) probands presented with breast cancer (including three men), with the remainder presenting with ovarian cancer. A total of 179 families (77%) had three or more affected individuals, 44 families (19%) had two affected individuals and nine index cases (4%) presented with either breast cancer <30 years (n=3) or bilateral breast cancer (n=6), with no family history.
Mutation screening of the coding and exon–intron boundaries of the gene was carried out by a combination of high-resolution melting mutation scanning analysis10 and DNA-sequencing analysis using an ABI 3130 XL DNA analyzer (Applied Biosystems, Foster City, CA, USA). Primer information is summarized in Table 1. Electropherograms were aligned using Lasergene-SeqMan software (DNASTAR, Madison, WI, USA) and every exon was screened for variants by comparing with MRG15 reference sequence (NC_000015.9, range 79165171–79190074).
In total, we identified 21 variants: 17 intronic changes, 3 coding SNPs and 1 variant localized in the 3′UTR (Table 2). Six out of the 17 intronic variants plus the one localized in the 3′UTR were referenced neither in dbSNP nor Ensembl SNP databases. These seven variants were each detected in not more than 1% of the patients indicating they could be rare and potentially harmful variants (Table 2). To gain further insight into possible negative effects of these non-referenced variants, we performed in silico analyses using accurate splicing prediction software: BDGP,11 NetGene 2 server12, 13 and GENSCAN.14 None of these intronic changes were predicted to impact on the splicing of the pre-mRNA. Analysis of the 3′UTR, using TargetScanHuman 5.1 software,15 revealed that the site where the variant in the 3′UTR lies is not a known target of miRNAs. Consequently, it is very unlikely that this variant has any effect on the regulation of MRG15 mRNA expression.
In conclusion, we found no evidence that mutations in MRG15 strongly predispose to breast cancer. Given our relatively small sample size, it remains possible that rare, or very rare, variants in this gene will be found to increase the risk for breast cancer. Moreover, sequencing of other novel genes whose products interact with BRCA proteins and their partners should be undertaken as members of this network are some of the most important contributors to the inherited susceptibility to breast cancer.
References
Narod, S. A. & Foulkes, W. D. BRCA1 and BRCA2: 1994 and beyond. Nat. Rev. Cancer 4, 665–676 (2004).
Chen, J., Silver, D. P., Walpita, D., Cantor, S. B., Gazdar, A. F., Tomlinson, G. et al. Stable interaction between the products of the BRCA1 and BRCA2 tumor suppressor genes in mitotic and meiotic cells. Mol. Cell 2, 317–328 (1998).
Tutt, A. & Ashworth, A. The relationship between the roles of BRCA genes in DNA repair and cancer predisposition. Trends Mol. Med. 8, 571–576 (2002).
Campeau, P. M., Foulkes, W. D. & Tischkowitz, M. D. Hereditary breast cancer: new genetic developments, new therapeutic avenues. Hum. Genet. 124, 31–42 (2008).
Rahman, N., Seal, S., Thompson, D., Kelly, P., Renwick, A., Elliott, A. et al. PALB2, which encodes a BRCA2-interacting protein, is a breast cancer susceptibility gene. Nat. Genet. 39, 165–167 (2007).
Jones, S., Hruban, R. H., Kamiyama, M., Borges, M., Zhang, X., Parsons, D. W. et al. Exomic sequencing identifies PALB2 as a pancreatic cancer susceptibility gene. Science 324, 217 (2009).
Erkko, H., Xia, B., Nikkila, J., Schleutker, J., Syrjakoski, K., Mannermaa, A. et al. A recurrent mutation in PALB2 in Finnish cancer families. Nature 446, 316–319 (2007).
Hayakawa, T., Zhang, F., Hayakawa, N., Ohtani, Y., Shinmyozu, K., Nakayama, J. et al. MRG15 binds directly to PALB2 and stimulates homology-directed repair of chromosomal breaks. J. Cell Sci. 123, 1124–1130 (2010).
Sy, S. M., Huen, M. S. & Chen, J. MRG15 is a novel PALB2-interacting factor involved in homologous recombination. J. Biol. Chem. 284, 21127–21131 (2009).
Reed, G. H. & Wittwer, C. T. Sensitivity and specificity of single-nucleotide polymorphism scanning by high-resolution melting analysis. Clin. Chem. 50, 1748–1754 (2004).
Reese, M. G., Eeckman, F. H., Kulp, D. & Haussler, D. Improved splice site detection in Genie. J. Comput. Biol. 4, 311–323 (1997).
Hebsgaard, S. M., Korning, P. G., Tolstrup, N., Engelbrecht, J., Rouze, P. & Brunak, S. Splice site prediction in Arabidopsis thaliana pre-mRNA by combining local and global sequence information. Nucleic Acids Res. 24, 3439–3452 (1996).
Brunak, S., Engelbrecht, J. & Knudsen, S. Prediction of human mRNA donor and acceptor sites from the DNA sequence. J. Mol. Biol. 220, 49–65 (1991).
Burge, C. & Karlin, S. Prediction of complete gene structures in human genomic DNA. J. Mol. Biol. 268, 78–94 (1997).
Lewis, B. P., Burge, C. B. & Bartel, D. P. Conserved seed pairing, often flanked by adenosines, indicates that thousands of human genes are microRNA targets. Cell 120, 15–20 (2005).
Acknowledgements
This work was supported by the Susan G Komen Foundation for the Cure, the Canadian Breast Cancer Research Alliance, the Cedars Cancer Institute, the Jewish General Hospital Weekend to End Breast Cancer, the Research Institute of the MUHC, the Finnish Cancer Foundation, the Northern Finnish Cancer Foundation, the Sigrid Jusélius Foundation, the Academy of Finland, the Orion-Farmos Research Foundation, the Northern Ostrobothnia Fund of the Finnish Cultural Foundation, the University of Oulu and the Oulu University Hospital. WDF holds a Fonds de la Recherche en Santé du Québec (FRSQ) national scientist award and MT holds an FRSQ clinician-scientist award.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Frio, T., Haanpää, M., Pouchet, C. et al. Mutation analysis of the gene encoding the PALB2-binding protein MRG15 in BRCA1/2-negative breast cancer families. J Hum Genet 55, 842–843 (2010). https://doi.org/10.1038/jhg.2010.112
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2010.112
Keywords
This article is cited by
-
Structural and functional insights into the epigenetic regulator MRG15
Acta Pharmacologica Sinica (2024)