Abstract
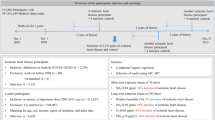
Fine particulate matter (PM2.5) in air pollution, primarily from combustion sources, is recognized as an important risk factor for cardiovascular events but studies of workplace PM2.5 exposure are rare. We conducted a prospective study of exposure to PM2.5 and incidence of ischemic heart disease (IHD) in a cohort of 11,966 US aluminum workers. Incident IHD was identified from medical claims data from 1998 to 2008. Quantitative metrics were developed for recent exposure (within the last year) and cumulative exposure; however, we emphasize recent exposure in the absence of interpretable work histories before follow-up. IHD was modestly associated with recent PM2.5 overall. In analysis restricted to recent exposures estimated with the highest confidence, the hazard ratio (HR) increased to 1.78 (95% CI: 1.02, 3.11) in the second quartile and remained elevated. When the analysis was stratified by work process, the HR rose monotonically to 1.5 in both smelter and fabrication facilities, though exposure was almost an order of magnitude higher in smelters. The differential exposure–response may be due to differences in exposure composition or healthy worker survivor effect. These results are consistent with the air pollution and cigarette smoke literature; recent exposure to PM2.5 in the workplace appears to increase the risk of IHD incidence.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Dong G-H, Qian ZM, Xaverius PK, Trevathan E, Maalouf S, Parker J et al. Association between long-term air pollution and increased blood pressure and hypertension in China. Hypertension 2013; 61: 578–584.
Peters A, Liu E, Verrier RL, Schwartz J, Gold DR, Mittleman M et al. Air pollution and incidence of cardiac arrhythmia. Epidemiology 2000; 11: 11–17.
Peters A, Dockery DW, Muller JE, Mittleman MA . Increased particulate air pollution and the triggering of myocardial infarction. Circulation 2001; 103: 2810–2815.
Brook RD, Rajagopalan S, Pope CA, Brook JR, Bhatnagar A, Diez-Roux AV et al. Particulate matter air pollution and cardiovascular disease. An update to the scientific statement from the American Heart Association. Circulation 2010; 121: 2331–2378.
Dockery DW, Pope CA, Xu X, Spengler JD, Ware JH, Fay ME et al. An association between air pollution and mortality in six US cities. N Engl J Med 1993; 329: 1753–1759.
Law MR, Morris JK, Wald NJ . Environmental tobacco smoke exposure and ischaemic heart disease: an evaluation of the evidence. BMJ 1997; 315: 973–980.
US Department of Health and Human Services The Health Consequences of Smoking: Cardiovascular Disease. A Report of the Surgeon General 1983 p 91–374.
US Department of Health and Human Services The Health Consequences of Smoking: A Report of the Surgeon General 2004 p 21–920.
Mills NL, Donaldson K, Hadoke PW, Boon NA, MacNee W, Cassee FR et al. Adverse cardiovascular effects of air pollution. Nat Clin Practice Cardiovas Med 2009; 6: 36–44.
Gan WQ, Koehoorn M, Davies HW, Demers Pa, Tamburic L, Brauer M . Long-term exposure to traffic-related air pollution and the risk of coronary heart disease hospitalization and mortality. Environ Health Perspect 2011; 119: 501–507.
Pope CA, Burnett RT, Krewski D, Jerrett M, Shi Y, Calle EE et al. Cardiovascular mortality and exposure to airborne fine particulate matter and cigarette smoke: shape of the exposure-response relationship. Circulation 2009; 120: 941–948.
Laden F, Schwartz J, Speizer FE, Dockery DW . Reduction in fine particulate air pollution and mortality: Extended follow-up of the Harvard Six Cities study. Am J Res Crit Care Med 2006; 173: 667–672.
Miller KA, Siscovick DS, Sheppard L, Shepherd K, Sullivan JH, Anderson GL et al. Long-term exposure to air pollution and incidence of cardiovascular events in women. N Engl J Med 2007; 356: 447–458.
Pope CA, Burnett RT, Thurston GD, Thun MJ, Calle EE, Krewski D et al. Cardiovascular mortality and long-term exposure to particulate air pollution: epidemiological evidence of general pathophysiological pathways of disease. Circulation 2004; 109: 71–77.
Pope CA, Burnett RT, Thun MJ, Calle EE, Krewski D, Ito K et al. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA 2002; 287 (9): 1132–1141.
Pope CA, Thun MJ, Namboodiri MM, Dockery DW, Evans JS, Speizer FE et al. Particulate air pollution as a predictor of mortality in a prospective study of U.S. adults. Am J Respir Crit Care Med 1995; 151 (3 Pt 1): 669–674.
US Department of Health and Human Services US Department of Health and Human Services. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta, Ga: US Dept of Health and Human Services, Center for Disease Control and Prevention, Coordinating Cente Atlanta, GA,. 2006.
Teo KK, Ounpuu S, Hawken S, Pandey MR, Valentin V, Hunt D et al. Tobacco use and risk of myocardial infarction in 52 countries in the INTERHEART study: a case-control study. Lancet 2006; 368: 647–658.
Cullen MR . Invited commentary: the search for preventable causes of cardiovascular disease—whither work? Am J Epidemiol 2009; 169: 1422–1425.
Fang SC, Cassidy A, Christiani DC . A systematic review of occupational exposure to particulate matter and cardiovascular disease. Int J Environ Res Public Health 2010; 7: 1773–1806.
Benke G, Abramson M, Sim M . exposures in the alumina and primary aluminium industry: an historical review. Ann Occup Hyg 1998; 42: 173–189.
Noth EM, Dixon-Ernst C, Liu S, Cantley L, Tessier-Sherman B, Eisen EA et al. Development of a job-exposure matrix for exposure to total and fine particulate matter in the aluminum industry. J Expo Sci Environ Epidemiol, (in press).
Schafer JL . Analysis of Incomplete Multivariate Data 1st edn. Chapman & Hall/CRC. 1997 pp 113.
Taiwo Oa, Sircar KD, Slade MD, Cantley LF, Vegso SJ, Rabinowitz PM et al. Incidence of asthma among aluminum workers. J Occupation Environ Med Am College Occupation Environ Med 2006; 48: 275–282.
IARC. Monograph 34: polynuclear aromatic compounds, Part3, industrial exposures in aluminum production, coal gasification, coke production, and iron and steel founding. World Health Organization: Geneva. 1984.
Applebaum KM, Malloy EJ, Eisen EA . Reducing healthy worker survivor bias by restricting date of hire in a cohort study of Vermont granite workers. Occup Environ Med 2007; 64: 681–687.
Applebaum KM, Malloy EJ, Eisen EA . Left truncation, susceptibility, and bias in occupational cohort studies. Epidemiology 2011; 22: 599–606.
Tessier-Sherman B, Galusha D, Taiwo OA, Cantley L, Slade MD, Kirsche SR et al. Further validation that claims data are a useful tool for epidemiologic research on hypertension. BMC Public Health 2013; 13: 51.
Jenkins RA, Palausky A, Counts RW, Bayne CK, Dindal AB, Guerin MR . Exposure to environmental tobacco smoke in sixteen cities in the United States as determined by personal breathing zone air sampling. J Exposure Anal Environ Epidemiol 1996; 6: 473–502.
Leaderer BP, Hammond SK . Evaluation of vapor-phase nicotine and respirable suspended particle mass as markers for environmental tobacco smoke. Environ Sci Technol 1991; 25: 770–777.
Dockery DW, Spengler JD . Personal exposure to respirable particulates and sulfates. J Air Pollution Control Assoc 1981; 31: 153–159.
Burstyn I, Kromhout H, Partanen T, Svane O, Langård S, Ahrens W et al. Polycyclic aromatic hydrocarbons and fatal ischemic heart disease. Epidemiology 2005; 16: 744–750.
Costello S, Garcia E, Hammond SK, Eisen EA . Ischemic heart disease mortality and PM 3. 5 in a cohort of autoworkers. Am J Industr Med 2012; 56: 317–325.
Friesen MC, Demers PA, Spinelli JJ, Eisen EA, Lorenzi MF, Le ND . Chronic and acute effects of coal tar pitch exposure and cardiopulmonary mortality among aluminum smelter workers. Am J Epidemiol 2010; 172: 790–799.
Brook RD, Franklin B, Cascio W, Hong Y, Howard G, Lipsett M et al. Air pollution and cardiovascular disease: a statement for healthcare professionals from the Expert Panel on population and prevention science of the American Heart Association. Circulation 2004; 109: 2655–2671.
Peters A . Ambient particulate matter and the risk for cardiovascular disease. Prog Cardiovas Dis 2011; 53: 327–333.
Salvi S, Blomberg A, Rudell B, Kelly F, Sandström T, Holgate ST et al. Acute inflammatory responses in the airways and peripheral blood after short-term exposure to diesel exhaust in healthy human volunteers. Am J Respir Crit Care Med 1999; 159: 702–709.
Ghio AJ, Kim C, Devlin RB . Concentrated ambient air particles induce mild pulmonary inflammation in healthy human volunteers. Am J Respir Crit Care Med 2000; 162 (3 Pt 1): 981–988.
Ghio AJ, Hall A, Bassett MA, Cascio WE, Devlin RB . Exposure to concentrated ambient air particles alters hematologic indices in humans. Inhal Toxicol 2003; 15: 1465–1478.
Libby P, Ridker PM, Maseri A . Inflammation and atherosclerosis. Circulation 2002; 105: 1135–1143.
Suwa T, Hogg JC, Quinlan KB, Ohgami A, Vincent R, Van Eeden SF . Particulate air pollution induces progression of atherosclerosis. J Am College Cardiol 2002; 39: 935–942.
Monn C, Becker S . Cytotoxicity and induction of proinflammatory cytokines from human monocytes exposed to fine (PM2.5) and coarse particles (PM10-2.5) in outdoor and indoor air. Toxicol Appl Pharmacol 1999; 155: 245–252.
Brook RD, Urch B, Dvonch JT, Bard RL, Speck M, Keeler G et al. Insights into the mechanisms and mediators of the effects of air pollution exposure on blood pressure and vascular function in healthy humans. Hypertension 2009; 54: 659–667.
Oberdörster G, Sharp Z, Atudorei V, Elder A, Gelein R, Lunts A et al. Extrapulmonary translocation of ultrafine carbon particles following whole-body inhalation exposure of rats. J Toxicol Environ Health 2002; 65: 1531–1543.
Nemmar A, Vanbilloen H, Hoylaerts MF, Hoet PH, Verbruggen A, Nemery B . Passage of intratracheally instilled ultrafine particles from the lung into the systemic circulation in hamster. Am J Respir Crit Care Med 2001; 164: 1665–1668.
Nemmar A, Hoet PHM, Vanquickenborne B, Dinsdale D, Thomeer M, Hoylaerts MF et al. Passage of inhaled particles into the blood circulation in humans. Circulation 2002; 105: 411–414.
Chevrier J, Picciotto S, Eisen Ea . A comparison of standard methods with g-estimation of accelerated failure-time models to address the healthy-worker survivor effect: application in a cohort of autoworkers exposed to metalworking fluids. Epidemiology 2012; 23: 212–219.
Park RM . Mortality at an automotive engine foundry and machining complex. J Occupation Environ Med 2001; 43: 483–493.
Rønneberg A . Mortality and cancer morbidity in workers from an aluminium smelter with prebaked carbon anodes—Part III: Mortality from circulatory and respiratory diseases. Occupation Environ Med 1995; 52: 255–261.
Cavallari JM, Eisen EA, Fang SC, Schwartz J, Hauser R, Herrick RF et al. PM2.5 metal exposures and nocturnal heart rate variability: a panel study of boilermaker construction workers. Environ Health 2008; 7: 36.
Bonde JP, Kolstad Ha . Noise and ischemic heart disease. Scand J Work Environ Health 2012; 38: 1–3.
Kivimäki M, Nyberg ST, Batty GD, Fransson EI, Heikkilä K, Alfredsson L et al. Job strain as a risk factor for coronary heart disease: a collaborative meta-analysis of individual participant data. Lancet 2012; 380: 1491–1497.
Robins JM, Hernán Ma, Brumback B . Marginal structural models and causal inference in epidemiology. Epidemiology 2000; 11: 550–560.
Acknowledgements
This work was supported by National Institutes of Health, Institute of Aging (R01 AG026291-01) and Center for Disease Control and Prevention, National Institute of Occupational Safety and Health (R01OH009939-01) and by Alcoa.
NIA Data Sharing: As an alternative to providing a de-identified data set to the public domain, we allow access for the purpose of re-analyses or appropriate “follow-on” analyses by any qualified investigator willing to sign a contractual covenant with the host Institution limiting use of data to a specific agreed upon purpose and observing the same restrictions as are limited in our contract with Alcoa, such as 60-day manuscript review for compliance purposes.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Drs Costello, Brown, Noth and Eisen do not have any conflicts of interest to declare. Ms Cantley and Ms Tessier-Sherman receive salary support from Alcoa, Inc through contracts with Yale University. Dr Cullen receives salary support from Alcoa, Inc through contracts with Stanford University. Dr Hammond receives compensation as a member of the scientific advisory board for Alcoa, Inc and has also consulted on exposure assessment and received compensation.
Rights and permissions
About this article
Cite this article
Costello, S., Brown, D., Noth, E. et al. Incident ischemic heart disease and recent occupational exposure to particulate matter in an aluminum cohort. J Expo Sci Environ Epidemiol 24, 82–88 (2014). https://doi.org/10.1038/jes.2013.47
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jes.2013.47
Keywords
This article is cited by
-
Acute Exposure of Atmospheric Ultrafine Particles Induced Inflammation Response and Dysregulated TGFβ/Smads Signaling Pathway in ApoE−/− Mice
Cardiovascular Toxicology (2021)
-
Economy Versus Environment: How Corporate Actors Harm Both
Critical Criminology (2019)
-
Exposure to occupational air pollution and cardiac function in workers of the Esfahan Steel Industry, Iran
Environmental Science and Pollution Research (2016)