Abstract
There is an imperative need to discover novel antimicrobials and anti-infective agents and build up innovative strategies to combat multidrug-resistant Salmonella. In this context, we had earlier confirmed that nisin has the potential to act in conjunction with β-lactams against murine salmonellosis using standard strain. However, evaluation of efficacy of these combinations against clinical isolates of Salmonella could be the next key step to confirm the value added potential of this peptide. The present study was therefore planned to validate the synergistic effects of nisin–β-lactams combinations against clinical isolates of Salmonella enterica serovar Typhi. MICs of the selected β-lactams, EDTA and nisin were determined by micro and macro broth dilution assays. In-vitro synergism between the agents was evaluated by fractional inhibitory concentration (FIC) index (checkerboard test) and time-kill assay. All the tested combinations showed synergy against the tested clinical strains except three, as evident by FIC index (checkerboard test) and time-kill assay. Especially, nisin–ceftriaxone and nisin–cefotaxime combinations demonstrated excellent synergistic activity. In view of the encouraging results obtained from the previous and present study, further studies need to be carried out using large number of strains from different regions to take into account the clinical variability of the strains. Though it is a simple study but highlights an important point about the possibility of using the said combination while making strategies to develop newer formulations.
Similar content being viewed by others
Introduction
Enteric fever, a systemic disease, with Salmonella enterica serovar Typhi being the main agent, remains a serious health concern. Although there is a wide variation in incidence rates and severity of typhoid worldwide, but in many developing countries, it is a life-threatening febrile disease turning into a major cause of mortality. There are an estimated 16 million to 21.6 million cases of typhoid fever every year, with the highest incidence being reported from Southeast Asia,1 mainly 493.5 cases per 100 000 persons/year in India, 15.3 per 100 000 persons/year in China to 451.7 per 100 000/year in Pakistan.2, 3 The true magnitude is difficult to quantify because the clinical picture is confused with many other febrile illnesses and most typhoid endemic areas lack facilities to confirm the diagnosis. However, the cumulative global death toll from typhoid fever is considerable and highlights the need for research on pathogenesis, immunity, vaccine development and identification of other therapeutic agents against the disease.1 Currently, the antimicrobials most widely regarded as optimal for the treatment of enteric fever are antibiotics like chloramphenicol, ampicillin and extended spectrum cephalosporins (β-lactams) as well as various quinolones.4 Nevertheless, the emergence of multidrug-resistant strains of Salmonella species (developed resistance to multiple antibiotics) is more worrisome in the present therapeutic scenario.5, 6 Thus, in light of the changing pattern to antibiotic sensitivity, there is a need to revisit the therapeutic regimen combined with efforts toward the development of effective alternatives.
In this context, bacteriocins appear to be the promising candidates. One such example is nisin, a well-known broad spectrum bacteriocin active against Gram-positive pathogens associated with foods.7 However, it is not active against Gram-negative organisms because the outer membrane (OM) of the Gram-negative cell wall acts as a barrier for the cell, restricting the access of the peptide to the cytoplasmic membrane.8 Nonetheless, certain agents like EDTA, citrate and plant essential oils which can disrupt the OM of Gram-negative bacteria can render them susceptible to nisin, but its use in clinical trials is restricted due to the limitations on in-vivo use of EDTA.9
Earlier, the combinations of bacteriocins and antibiotics have been successfully employed to overcome antibiotic resistance in selected cases10 and recently, we had also demonstrated that nisin has the potential to act in conjunction with conventional antibiotics (β-lactam) against murine salmonellosis.7 However, further evaluation of these nisin–β-lactam combinations against clinical isolates of Salmonella could be the next key step to confirm the value added potential of this peptide. The present study was therefore planned to validate the synergistic effects of nisin, in combination with conventional β-lactams, against clinical isolates of S. enterica serovar Typhi.
Materials and methods
Bacterial strain and growth medium
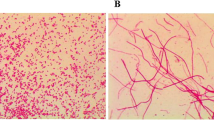
Standard strain of S. enterica serovar Typhi (Ty2), originally procured from Central Research Institute, Kasauli, India, (maintained in our laboratory for the last several years and have also been used in recent studies) along with 12 clinical isolates of serovar Typhi (procured from Government Medical College and Hospital (GMCH), Chandigarh) were used in the present study. All isolates included in this study were recovered from random, sporadic and unrelated cases of typhoid fever. The isolates were revived on nutrient agar plates and were grown overnight with aeration for 18 h at 37 °C in a nutrient broth (5.0 g l−1 peptone, 5.0 g l−1 NaCl, 1.5 g l−1 beef extract, 1.5 g l−1 yeast extract, pH 7.4±0.2; HiMedia, Mumbai, India) and identified as S. enterica serovar Typhi by biochemical tests. All the cultures were maintained on nutrient agar slants and preserved at −80 °C by making 20% glycerol stocks.
For preparation of bacterial cell suspension, bacterial cells grown overnight (at 37 °C, 150 r.p.m.) in nutrient broth were collected by centrifugation (8000 r.p.m., 15 min), washed once with 10 mM sodium phosphate-buffered saline (pH 7.2), and resuspended in phosphate-buffered saline to a final concentration of approximately 107 CFU ml−1.
Agents
Nisin, EDTA, ampicillin, ceftriaxone and cefotaxime powder were obtained from Sigma-Aldrich (St Louis, MO, USA). Ampicillin, ceftriaxone, cefotaxime and EDTA were dissolved in distilled water, whereas nisin was dissolved in 0.2 N HCl. Stock solutions of 500 mM for EDTA and 1 mg ml−1 for other agents were prepared and used within 1 week.
Antimicrobial sensitivity testing
Antibiotic sensitivity profile of the standard strain and all the tested clinical isolates were checked using HiMedia Octadisc-GII Minus, Combi-508, and Combi-513 by the method of Bauer et al.11 The average inhibitory zone diameter was compared with the standards provided by the Clinical and Laboratory Standards Institute (CLSI) guidelines.12 The antibiotic sensitivity pattern against the following antibiotics was determined: Cefotaxime (CTX) 30 μg, Cefalexin (CN) 30 μg, Co-Trimoxazole (COT) 25 μg, Chloramphenicol (C) 30 μg, Nalidixic acid (NA) 30 μg, Furazolidone (FR) 50 μg, Norfloxacin (NX) 10 μg, Oxytetracycline (O) 30 μg, Ceftazidime (CAZ) 30 μg, Gentamicin (GEN) 10 μg, Ceftriaxone (CTR) 30 μg, Ciprofloxacin (CIP) 5 μg, Netillin (NET) 30 μg, Gatifloxacin (GAT) 30 μg, Cefuroxime (CXM) 30 μg, Ampicillin (AMP) 10 μg, Amikacin (AK) 30 μg, Cephalothin (CEP) 30 μg.
Quantitative determination of the antibacterial activity (MIC determination)
The MICs of these agents against standard strain and clinical isolates of serovar Typhi were determined by macro and micro broth dilution assay methods as described earlier.7, 13 Overnight growth was monitored by measuring the OD at 620 nm. The MIC was defined as the lowest concentration of each antibiotic not producing any visible microbial growth.
Fractional inhibitory concentrations
To evaluate synergy, the fractional inhibitory concentration (FIC) index was determined by checkerboard microtitre test, using an 8-by-8 well configuration at 64 different combinations as described earlier.7 The FIC was calculated after dividing the MIC of the tested agent in combination by the MIC of tested agent alone separately. The FIC index, obtained by adding both the FICs, was interpreted as indicating a synergistic effect when it was ⩽0.5, as additive or indifferent when it was >0.5 and ⩽2.0, and as antagonistic when it was >2.0.
Time-kill assay
The in-vitro synergy as estimated by checkerboard technique was further confirmed by time-kill assay. The antimicrobial action of all the antibacterial agents (nisin, EDTA and antibiotics) was determined at their respective MICs, when the agents were used alone or in combination against S. enterica serovar Typhi (Ty2) and one representative clinical isolate as described earlier.7 For each agent, six flasks of nutrient broth were prepared corresponding to various time intervals; that is, 0, 3, 6, 12, 24 and 48 h. The plates were incubated at 37 °C for 24 h for enumeration of CFUs.
Statistical analysis
Data were expressed as means±standard deviations for three to five independent experiments. Statistical analysis was done by Student’s unpaired t-test and one-way analysis of variance using Jandel Sigma Stat statistical software, version 2.0. In all cases, statistical significance was defined as having a P-value of <0.05.
Results
Antibiogram analysis
Analysis of antibiogram data revealed that serovar Typhi (Ty2) was sensitive to all the tested antibiotics. On the other hand, clinical isolate C3 was observed to be sensitive to all the tested antibiotics and clinical isolates C7 and C11 were observed to be resistant to single antibiotic, that is, nalidixic acid and oxytetracycline, respectively. Remaining nine clinical strains were found to be MDR strains as they were resistant to >1 antibiotic (Table 1).
MIC determination
MIC for various agents was determined and confirmed by both macro and micro broth dilution assay. MICs of ampicillin, ceftriaxone, cefotaxime and EDTA were observed to be 4 μg ml−1, 8 μg ml−1, 20 μg ml−1 and 20 mM, respectively, against serovar Typhi (Ty2). Using nisin, no inhibition of growth was observed till 400 μg ml−1 against all the tested Salmonella strains. The MIC values against all the tested isolates are summarized in Table 2. According to CLSI guidelines,12 all the tested clinical isolates of serovar Typhi were classified as resistant to ceftriaxone and cefotaxime (as per the MIC breakpoints for ceftriaxone and cefotaxime susceptible (⩽1), intermediate (1–4) and resistant (⩾4)). Conversely, except one clinical isolate C12, all the tested isolates were observed to be susceptible to ampicillin (as per the MIC breakpoints for ampicillin susceptible (⩽8), intermediate (8–32) and resistant (⩾32)).
Fractional inhibitory concentrations
Against serovar Typhi (Ty2), all tested combinations (nisin–EDTA, nisin–ampicillin, nisin–ceftriaxone and nisin–cefotaxime) showed synergy as indicated by FIC indices, which were ⩽0.5 for all the combinations. Against clinical isolates C2 and C8, all the tested combinations were observed to illustrate additive effect as indicated by FIC indices, which were between 0.5 and 1. Moreover, clinical isolate C12, the combinations of nisin–ceftriaxone and nisin—cefotaxime were found to be synergistic as indicated by FIC indices, which were ⩽0.5, whereas nisin–ampicillin and nisin–EDTA combinations were found to have additive effects against isolate C12 as indicated by FIC indices. All the remaining nine tested clinical isolates showed synergy for the three tested combinations, which were evident by ⩽0.5 FIC indices (Table 3). In other words, when used in combination with nisin, MICs of EDTA and ampicillin were reduced by 4- to 8-fold, and MICs of ceftriaxone and cefotaxime were reduced by 8- to 16-fold, respectively.
Time-kill assay
To confirm the checkerboard analysis, serovar Typhi (Ty2) and isolate C12 were chosen to perform time-kill assay. Against serovar Typhi (Ty2), nisin–ampicillin and nisin–EDTA exhibited synergy after 12 h, whereas nisin–ceftriaxone and nisin–cefotaxime showed synergy after 6 h, respectively (Figure 1). On the other hand, against clinical isolate C12, both nisin–ceftriaxone and nisin–cefotaxime combination showed synergy after 6 and 12 h respectively, which was evident by a ⩾2 log10 unit reduction as compared to the killing of same magnitude by each agent alone, which seems to occur at 24 h (approximately) indicating that the combinations could kill bacteria more rapidly than each single agent. Though nisin–EDTA, nisin–ampicillin were able to reduce the growth of clinical isolate more significantly as compared to each single agent, it did not show synergy because log10 unit reduction was less than 2 log10 units at every time point as compared to the killing of same magnitude by each agent alone (Figure 2).
Log10 CFU ml−1 of Salmonella enterica serovar Typhi (Ty2) at different time intervals in presence of antibiotic alone (MIC) and in presence of nisin+antibiotic (1 × MIC+1 × MIC). Values are expressed as mean±standard deviation of three individual values. ‡P<0.001 versus log10 CFU of serovar Typhi (Ty2) after 12 h in the absence of any antibacterial agent (control); §P<0.01 versus log10 CFU of serovar Typhi (Ty2) after 12 h in the presence of nisin (400 μg ml−1); αP<0.05 versus log10 CFU of serovar Typhi (Ty2) after 6 h in the presence of ampicillin (4 μg ml−1); βP<0.05 versus log10 CFU of serovar Typhi (Ty2) after 6 h in the presence of EDTA (20 mM); *P<0.001 versus log10 CFU of serovar Typhi (Ty2) after 6 h in the absence of any antibacterial agent (control); #P<0.01 versus log10 CFU of serovar Typhi (Ty2) after 6 h in the presence of nisin (400 μg ml−1); †P<0.05 versus log10 CFU of serovar Typhi (Ty2) after 6 h in the presence of ceftriaxone (8 μg ml−1); ¢P<0.05 versus log10 CFU of serovar Typhi (Ty2) after 12 h in the presence of cefotaxime (20 μg ml−1).
Log10 CFU ml−1 of Salmonella enterica serovar Typhi (clinical insolate, C12) at different time intervals in the presence of antibiotic alone (MIC) and in the presence of nisin+antibiotic (1 × MIC+1 × MIC). Values are expressed as mean±standard deviation of three individual values. *P<0.001 versus log10 CFU of serovar Typhi (C12) after 6 h in the absence of any antibacterial agent (control); #P<0.01 versus log10 CFU of serovar Typhi (C12) after 6 h in the presence of nisin (400 μg ml−1); †P<0.05 versus log10 CFU of serovar Typhi (C12) after 6 h in the presence of ceftriaxone (12 μg ml−1); ‡P<0.001 versus log10 CFU of serovar Typhi (C12) after 12 h in the absence of any antibacterial agent (control); §P<0.01 versus log10 CFU of serovar Typhi (C12) after 12 h in the presence of nisin (400 μg ml−1); ¢P<0.05 versus log10 CFU of serovar Typhi (C12) after 12 h in the presence of cefotaxime (20 μg ml−1).
Discussion
In the past, the high prevalence of MDR strains among Salmonella isolates has prompted fluoroquinolones as the primary antibiotics. However, in the recent past, resistance to this class of antibiotics has been reported among both serovar Typhi14 and serovar Paratyphi.15 Thus, the use of third-generation cephalosporins, such as ceftriaxone, for the management of enteric fever gained acceptance in the last decades.16 However, resistance cassettes against third-generation cephalosporins had already been found in integron-like structures in other enterobacteriaceae, and resistance to third-generation cephalosporins was recently described in Salmonella as well.17, 18 Therefore, there is an urgent need to discover novel antimicrobials and anti-infective agents and to develop innovative strategies to combat them. Use of antimicrobial peptide in conjunction with antibiotics can be perceived as a promising solution to the growing problem of resistance to conventional antibiotics particularly by facilitating the entry of drug into the cells. Combination therapy can therefore be used to increase the antimicrobial activity as well as to broaden the antimicrobial spectrum.
Nisin acts mainly by permeating the cytoplasmic membrane with the formation of transient pores, which allow leakage of intracellular metabolites and dissipation of membrane potential and by the disruption of cell wall biosynthesis through binding to lipid II.19, 20 However, Gram-negative bacteria are covered by an OM composed of a phospholipid bilayer, surrounded by a network of lipids and polysaccharides referred to as lipopolysaccharides. Therefore, due to the barrier provided by the OM, nisin alone is generally not effective against Gram-negative bacteria as evident by broth dilution assay (no inhibition of growth was observed till 400 μg ml−1 against all the tested Salmonella strains). Nevertheless, in our previous study we demonstrated that nisin was able to exert its antimicrobial activity against Salmonella in the presence of conventionally used β-lactams (ampicillin, ceftriaxone and cefotaxime) at much lower concentrations.7 Therefore, in the present study, nisin–β-lactam combination was checked against standard strain of S. enterica serovar Typhi (Ty2) and clinical isolates of S. enterica serovar Typhi for the validation of the above-mentioned combinations.
Checkerboard assay revealed that out of 13 tested Salmonella isolates including the standard strain, 10 isolates showed synergy with all the four tested combination. Remaining three isolates though did not exhibit any synergy, but were observed to illustrate additive effect with nisin–EDTA and nisin–ampicillin combinations, which indicates that there is a need to evaluate the efficacy of other combinations. These results have strengthen our earlier hypothesis that β-lactams and nisin acted cooperatively by increasing the permeabilization of nisin across bacterial OM and by rendering the drug efflux pumps ineffective, thereby increasing cellular drug accumulation by altering cell permeability, leading to collapse of membrane potential and causing rapid efflux of materials present in cytosolic milieu.21, 22 In conclusion, when used in combination, nisin reduced the concentration of the β-lactams which may reduce the chances of developing resistance in the pathogens besides reducing the associated side effects of the former. This careful and limited antibiotic use might help in removal of selective pressure, thereby reducing the chances of developing resistance.
Time-kill assay results also supported the checkerboard assay findings as standard strain exhibited synergy against all the tested combinations and clinical isolate showed synergy against nisin–ceftriaxone and nisin–cefotaxime. β-Lactams have also been reported to trigger hydroxyl radical and superoxide formation, which damage DNA, lipids and proteins.23, 24 This might be attributed to the fact that increased influx of the antibiotics due to pore formation by nisin results in faster inhibition.
Most interesting finding of the study was that addition of nisin amplified the activity of the β-lactams (ampicillin, ceftriaxone and cefotaxime) at much lower MICs, thereby rendering serovar Typhi isolates sensitive to tested β-lactams, which were earlier found to be resistant as per the CLSI guidelines. This increased therapeutic efficacy might be attributed to multitargeted approach of the combinations.
In conclusion, nisin–β-lactam combinations, especially nisin–ceftriaxone and nisin—cefotaxime combinations, demonstrated excellent synergistic activity against clinical isolates of S. enterica serovar Typhi. In view of the encouraging results obtained from the previous and present study, validation of the efficacy of the tested combinations further needs to be done having large number of isolates because of the clinical variability of Salmonella strains in different geographical areas.
References
Tsolis, R. M ., Xavier, M. N ., Santos, R. L . & Bäumler, A. J . How to become a top model: impact of animal experimentation on human Salmonella disease research. Infect. Immun. 79, 1806–1814 (2011).
Siddiqui, F. J ., Rabbani, F ., Hasan, R ., Nizami, S. Q . & Bhutta, Z. A . Typhoid fever in children: some epidemiological considerations from Karachi, Pakistan. Int. J. Infect Dis. 10, 215–222 (2006).
Ochiai, R. L ., Acosta, C. J . & Danovaro-Holliday, M . A study of typhoid fever in five Asian countries: disease burden and implications for controls. Bull. World Health Organ. 86, 260–268 (2008).
Threlfall, E. J ., Skinner, J. A . & Ward, L. R . Detection of decreased in vitro susceptibility to ciprofloxacin in Salmonella enterica serotypes typhi and paratyphi A. J. Antimicrob. Chemother. 48, 740–741 (2001).
Joerger, R. D . Alternatives to antibiotics: bacteriocins, antimicrobial peptides and bacteriophages. Poult. Sci. 82, 640–647 (2003).
Birosova, L . & Mikulasova, M . Development of triclosan and antibiotic resistance in Salmonella enterica serovar Typhimurium. J. Med. Microbiol. 58, 436–441 (2009).
Singh, A. P ., Prabha, V . & Rishi, P . Value addition in the efficacy of conventional antibiotics by nisin against Salmonella. PLoS ONE 8, e76844 (2013).
Field, D . et al. Bioengineered nisin A derivatives with enhanced activity against both Gram positive and Gram negative pathogens. PLoS ONE 7, e46884 (2012).
Boziaris, I. S . & Adams, M. R . Effect of chelators and nisin produced in situ on inhibition and inactivation of Gram negatives. Int. J. Food Microbiol. 53, 105–113 (1999).
Cassone, M . & Otvos, L. Jr . Synergy among antibacterial peptides and between peptides and small-molecule antibiotics. Expert Rev. Anti Infect. Ther. 8, 703–716 (2010).
Bauer, A. W ., Kirby, W. M ., Sherris, J. C . & Turck, M . Antimicrobial susceptibility testing by a standardized single disc method. Am. J. Clin. Pathol. 45, 493–496 (1966).
Clinical and Laboratory Standards Institute M100-S20. Performance Standards for Antimicrobial Susceptibility Testing: 20th Informational Supplement, CLSI, Wayne, PA, USA (2010).
Rishi, P ., Preet, S ., Bharrhan, S . & Verma, I . In-vitro and in-vivo synergistic effects of cryptdin 2 and ampicillin against Salmonella. Antimicrob. Agents Chemother. 55, 4176–4182 (2011).
Chuang, C . et al. Surveillance of antimicrobial resistance of Salmonella enterica serotype Typhi in seven Asian countries. Epidemiol. Infect. 137, 266–269 (2009).
Maskey, A. P . et al. Emerging trends in enteric fever in Nepal: 9124 cases confirmed by blood culture 1993–2003. Trans. R. Soc. Trop. Med. Hyg. 102, 91–95 (2008).
Chalon, M. C ., Acuña, L ., Morero, R. D ., Minahk, C. J . & Bellomio, A . Membrane-active bacteriocins to control Salmonella in foods: are they the definite hurdle? Food Res. Int. 45, 735–744 (2012).
Majtan, J ., Majtanova, L . & Majtan, V . Increasing trend of resistance to nalidixic acid and emerging ceftriaxone and ciprofloxacin resistance in Salmonella enterica serovar Typhimurium in Slovakia, 2005 to 2009. Diagn. Microbiol. Infect. Dis. 68, 86–88 (2010).
Ye, J . et al. Analysis of pSC138, the multidrug resistance plasmid of Salmonella enterica serotype Choleraesuis SC-B67. Plasmid 65, 132–140 (2011).
Cotter, P. D ., Ross, R. P . & Hill, C . Bacteriocins-a viable alternative to antibiotics? Nat. Rev. Microbiol. 11, 95–105 (2013).
Freeman, M. F . et al. Metagenome mining reveals polytheonamides as posttranslationally modified ribosomal peptides. Science 338, 387–390 (2012).
Ruhr, E . & Sahl, H. G . Mode of action of the peptide antibiotic nisin and influence on the membrane potential of whole cells and on cytoplasmic and artificial membrane vesicles. Antimicrob. Agents Chemother. 27, 841–845 (1985).
Gut, I. M ., Blanke, S. R . & van der Donk, W. A . Mechanism of inhibition of Bacillus anthracis spore outgrowth by the lantibiotic nisin. ACS Chem. Biol. 6, 744–752 (2011).
Kohanski, M. A ., Dwyer, D. J . & Collins, J. J . How antibiotics kill bacteria: from targets to networks. Nat. Rev. Microbiol. 8, 423–435 (2010).
Kohanski, M. A ., Dwyer, D. J ., Hayete, B ., Lawrence, C. A . & Collins, J. J . A common mechanism of cellular death induced by bactericidal antibiotics. Cell 130, 797–810 (2007).
Acknowledgements
We acknowledge Dr Jagadish Chander and Dr Varsha Gupta, Government Medical College and Hospital (GMCH), Chandigarh, for providing clinical isolates to carry out this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rishi, P., Preet Singh, A., Garg, N. et al. Evaluation of nisin–β-lactam antibiotics against clinical strains of Salmonella enterica serovar Typhi. J Antibiot 67, 807–811 (2014). https://doi.org/10.1038/ja.2014.75
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ja.2014.75
This article is cited by
-
Combination antimicrobial therapy: in vitro synergistic effect of anti-staphylococcal drug oxacillin with antimicrobial peptide nisin against Staphylococcus epidermidis clinical isolates and Staphylococcus aureus biofilms
Annals of Clinical Microbiology and Antimicrobials (2024)
-
Antimicrobial Peptides: the Achilles’ Heel of Antibiotic Resistance?
Probiotics and Antimicrobial Proteins (2019)
-
Lanthipeptides: chemical synthesis versus in vivo biosynthesis as tools for pharmaceutical production
Microbial Cell Factories (2016)