Abstract
Nesfatin/nucleobindin-2 (nesf/NUCB2), a precursor of the anorexigenic protein nesfatin-1, is selectively expressed in the hypothalamic nuclei, which are central to the regulation of the autonomic nervous system. The present study sought to investigate the involvement of nesf/NUCB2 in the regulation of blood pressure and ingestive behavior, by using nesf/NUCB2-transgenic (Tg) mice. Blood pressure and heart rates were measured under conscious and unconscious conditions. Twenty-four-hour water intake and urine volume of male nesf/NUCB2-Tg mice and their littermates in metabolic cages were measured. After killing, kidney weight was measured and the mRNA expression of epithelial sodium channel (ENaC)-α and ENaC-γ was measured in the hypothalamus and kidney with real-time PCR. Systolic, diastolic and mean blood pressure were significantly higher in nesf/NUCB2-Tg mice, but pulse rate was not affected in conscious mice. In contrast, isoflurane anesthesia prevented an increase in blood pressure in the nesf/NUCB2-Tg mice. Twenty-four-hour water intake and urine volume were significantly higher in the nesf/NUCB2-Tg mice than in their non-Tg littermates. Urine sodium concentration was significantly lower in the nesf/NUCB2-Tg mice, although the serum sodium concentration and urine sodium excretion were not different between the genotypes. Kidney weight was significantly higher in the nesf/NUCB2-Tg mice than their non-Tg littermates, although there were no clear differences in the kidney histological findings between genotypes. The mRNA expression of ENaC-γ, but not ENaC-α, was decreased in the hypothalami of nesf/NUCB2-Tg mice. Our data suggested that Nesf/NUCB2 is involved in the regulation of blood pressure in the brain.
Similar content being viewed by others
Introduction
Nesfatin-1 has been found to be involved in the regulation of feeding behavior in the paraventricular nucleus of the hypothalamus.1 Nesfatin/nucleobindin-2 (nesf/NUCB2), a precursor protein of nesfatin-1, is ubiquitously expressed in peripheral tissues and the hypothalamus.2 Although the origin of circulating nesfatin-1 in the blood has not been clarified, nesfatin-1 crosses the blood-brain barrier3, 4 and peripherally administered nesfatin-1 reaches the feeding center in the hypothalamus and decreases short-term food consumption in mice fed ad libitum.5
Nesfatin-1 may be involved in the regulation of blood pressure, because it is expressed in the cardiovascular control center.6 Intracerebroventricular administration of nesfatin-1 increases mean blood pressure (MBP) in conscious, freely moving rats and the α-adrenergic antagonist, phentolamine, abrogates the increase in MBP by nesfatin-1.7 However, peripherally administered nesfatin-1 also increases mouse blood pressure without affecting heart rate and simultaneous administration of a β-adrenergic receptor blocker completely blocks the effect of nesfatin-1 on blood pressure.8 These data indicate that circulating nesfatin-1 may be involved in peripheral regulation of blood pressure via the activation of β-adrenergic receptors in the periphery. In addition, circulating nesfatin-1 levels are correlated with body adiposity,9 a marker of insulin resistance, and systolic and diastolic blood pressure (SBP and DBP, respectively) in patients with polycystic ovary syndrome.10 Nesfatin-1 may have a role in the development of hypertension in obese people. However, the exact mechanism by which nesfatin-1 regulates blood pressure has not yet been thoroughly clarified.
Recently, our immunohistochemical observations have indicated selective expression of nesfatin/NUCB2 in vascular endothelial cells, but not smooth muscular cells, of arteries and in renal collecting ducts of the kidney.11 In addition, nesfatin/NUCB2 is co-expressed with epithelial sodium channels (ENaC) in the renal collecting duct of the kidney.11 Activation of the renal sympathetic nervous system has a role in the development of salt-induced hypertension by increasing sodium retention in the kidney.12 β-Adrenergic receptors are present in renal collecting ductal cells13 and β-adrenergic receptor activation increases net fluid secretion by cultured inner collecting ducts.14 Such findings indicate the possible involvement of nesfatin/NUCB2 in the regulation of blood pressure via water and sodium metabolism in the kidney. We have recently established nesf/NUCB2-transgenic (Tg) mice, which are susceptible to high fat-induced obesity.15 The present studies sought to examine a possible role of nesfatin/NUCB in the regulation of water metabolism and blood pressure by using nesf/NUCB2-Tg mice.
Methods
Generation of nesf/NUCB2 Tg mice
Nesf/NUCB2-Tg mice were generated to produce nesf/NUCB2 by insertion of nesf/NUCB2 cDNA into a construct containing the CAG promoter.15 Briefly, a 1.7 kb fragment of the CAG promoter was ligated to a 1263 bp fragment corresponding to position +202 to +1464 of Nucb2 (BC010459) cDNA, including a rabbit β-globin polyadenylation signal. Offspring were screened for genomic integration by PCR analysis of tail DNA. The experimental protocol was approved by the Animal Research Committee of International University of Health and Welfare (number D13002).
Experimental protocol
Nesf/NUCB2-Tg mice and their non-Tg littermates were fed normal laboratory chow and given free access to both food and water. In the first experiment, daily water intake was chronologically measured in individual cages of mice at 7–9 weeks of age. In the second experiment, water intake was measured and urine was simultaneously collected for 24 h for mice 8–9 weeks of age, housed individually in metabolic cages (Buguggiate (VA), Lombardy Region, Italy). Collected urine was frozen at −20 °C for assay after the daily urine volume was measured.
After killing, blood samples were collected and the weights of the kidneys were measured. The obtained serum and kidneys were frozen for assays.
Western blotting and real-time PCR analysis
Overexpression in the hypothalami and kidneys of nesf/NUCB2-Tg mice was confirmed by western blotting and reverse transcriptase-PCR methods. Nesf/NUCB2 Tg mice and their non-Tg littermates were killed and their hypothalami and kidneys were isolated. Western blotting was performed as described previously.15
Total RNA was isolated from the whole hypothalami and kidneys by using a PureLink RNA Mini Kit (Ambion by Life Technologies, Carlsbad, CA, USA), according to the manufacturer’s instructions. Reverse transcription was performed using a High Capacity RNA-to-cDNA Kit (Applied Biosystems, Foster City, CA, USA). Quantitative PCR was performed using TaqMan Fast Advanced Master Mix and a StepOnePlus System with version 2.1 software (Applied Biosystems) according to the manufacturer’s instructions. Primers used for quantitative PCR were also obtained from Applied Biosystems. Gapdh was used as the internal control. All analyses, including settings for threshold and quantification cycle values, were adjusted automatically by using the default settings. Expression of ENaC-α, ENaC-γ and Nucb2 cDNA was normalized to that of Gapdh. All PCR was performed in 96-well plates by using 40 cycles of 95 °C for 20 s and 60 °C for 20 s.
Blood pressure measurement
A non-invasive blood pressure monitor (Model MK-2000ST, Muromachi Kikai, Tokyo, Japan) was used for the measurement of blood pressure and pulse rate (PR).16, 17 Blood pressure and heart rate were measured in conscious mice. Subsequently, the mice were anesthetized to an unconscious condition with a very low concentration of isoflurane inhalation (1.0%). The unconscious condition was defined as a condition in which a mouse stopped voluntary movement but showed a reflex in response to a toe pinch. Blood pressure and heart rate were also measured in an unconscious condition. The measurements were conducted between 1000 and 1200 h, and an average of three to five measurements was used for the individual value.
Assays
Electrolyte concentrations in the urine and serum were measured with an automatic analyzer. Serum aldosterone and arginine vasopressin concentrations were measured with commercially available ELISA kits (Aldosterone ELISA, BioVendor, Brno, Czech Republic, and Arg8-Vasopressin ELISA kit, Abcam, Cambridge, UK, respectively). Serum nesfatin-1 concentration was measured using an ELISA kit for mice (Shibayagi, Shibukawa, Japan).
Histological analysis
The frozen kidneys were embedded into paraffin blocks and coronal cross-sections were taken for histological analysis of the kidneys. The cross-sections were stained with hematoxylin and eosin or Masson’s trichrome for the evaluation of glomerular sizes or fibrosis, respectively. In the evaluation of glomerular sizes, the average area of 10 randomly selected glomeruli was used for each mouse. A percentage of Masson’s trichrome-positive area (blue area) per field was measured in the cortex and medulla at a magnification of × 200 and an average of three fields was used as the fibrotic area.
Statistical analysis
All data are expressed as the mean±s.d. The statistical analysis was performed by the analysis of variance, followed by Student’s t-test for the individual comparison of the means.
Results
Changes in blood pressure
Changes in blood pressure and heart rate measured in nesf/NUCB2-Tg mice and their non-Tg littermates are presented in Figure 1. SBP, DBP and MBP were significantly higher in nesf/NUCB2-Tg mice than in their non-Tg littermates in a conscious condition (Figures 1a–c). However, PR was not different between the genotypes (Figure 1d).
Changes in systolic blood pressure (SBP; a and e), diastolic blood pressure (DBP; b and f), mean blood pressure (MBP; c and g) and pulse rate (PR; d and h) in nesf/NUCB2-Tg mice and their non-Tg littermates under the conscious condition (a–d) and unconscious condition (e–h). N=12 in each group under the conscious condition (a–d) and N=8 in each group under the unconscious condition (e–h). *P<0.05 versus non-Tg mice.
SBP, DBP and MBP were not different between the conscious and unconscious conditions between nesf/NUCB2-Tg mice and non-Tg mice (Figure 1). The differences of SBP, DBP and MBP between the genotypes disappeared in the unconscious condition (Figures 1e–g). PR was lower in the unconscious condition (Figure 1h) than in the conscious condition (Figure 1d) but was not different between the genotypes (Figure 1h).
Changes in daily water intake, daily urine volume, kidney weight and electrolyte concentration
In the first experiment, chronological changes in water intake and urine volume for 24 h were evaluated in individually caged mice. Water intake significantly increased from the age of 8 weeks (Figure 2a). In the second experiment, 24 h water intake and urine volume were measured in a metabolic cage at the age of 8–9 weeks. An increase in 24 h water intake was found in nesf/NUCB2-Tg mice and 24 h urine volume was significantly higher in nesf/NUCB2-Tg mice than their non-Tg littermates (Figures 2b and c). However, there was no difference in body weight or in 24 h food or sodium intake between the nesf/NUCB2-Tg and non-Tg mice (Table 1).
As shown in Table 2, sodium concentration in the urine was significantly lower in nesf/NUCB2-Tg mice than non-Tg littermates, although 24 h urine sodium, potassium and chloride excretion and sodium, potassium and chloride concentrations in the serum were not significantly different between the genotypes. There were no significant differences between the genotypes in serum aldosterone (Tg mice: 190.0±79.9 pg ml−1 (N=9), non-Tg littermates: 218.5±83.8 pg ml−1 (N=12)) and arginine vasopressin concentrations (Tg mice: 312.7±230.5 pg ml−1 (N=9), non-Tg littermates: 189.7±72.0 pg ml−1 (N=5)).
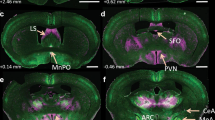
Expression of nesf/NUCB2 in the brains and kidneys of nesf/NUCB2-Tg mice
Overexpression of nesf/NUCB2 in the brains and kidneys of nesf/NUCB2-Tg mice was confirmed by western blotting (Figure 3a) and real-time PCR analysis (Figure 3b). Nesf/NUCB2 mRNA was overexpressed in the hypothalami and kidneys of nesf/NUCB2-Tg mice (1.7 and 2.4 times higher than their non-Tg littermates, respectively, Figure 3b). However, the serum nesfatin-1 concentration was not significantly different between the genotypes (Figure 3c).
(a) Results of western blot analysis of brains and kidneys of nesf/NUCB2-Tg mice and their non-Tg littermates. (b) Expression of nesf/NUCB2 mRNA in the hypothalami and kidneys of nesf/NUCB2-Tg mice and their non-Tg littermates. N=18 (non-Tg mice), 15 (Tg mice). *P<0.05 and **P<0.01 versus non-Tg mice. (c) Plasma levels of nesfatin-1 in nesf/NUCB2-Tg mice and their non-Tg littermates. N=5 in each group.
Histological analysis of kidney
The weights of the kidneys were significantly higher in nesf/NUCB2-Tg mice than their non-Tg littermates (Figure 4a). Kidney weight per body weight was also significantly higher in nesf/NUCB2-Tg mice. However, no obvious histological differences in the kidneys were found between the genotypes (Figures 4b–e).
(a) The kidney weight and kidney weight per body weight in sacrificed nesf/NUCB2-Tg mice and their non-Tg littermates. N=11 (non-Tg mice), 12 (Tg mice). *P<0.05 and **P<0.01 versus non-Tg mice. (b) Representative images of hematoxylin and eosin -stained kidneys of nesf/NUCB2-Tg mice and their non-Tg littermates. (c) Average glomerular size. (d and e) Cortical and medullar fibrotic area, respectively.
Changes in ENaC expression
Figure 5 shows changes in the expression of ENaC-α mRNA and ENaC-γ mRNA in the hypothalamus and kidney. In the hypothalamus, ENaC-α mRNA expression was not different between nesf/NUCB2-Tg mice and their non-Tg littermates, but ENaC-γ mRNA expression was significantly lower (0.6 times) in nesf/NUCB2-Tg mice than their non-Tg littermates. However, there were no differences between the genotypes in ENaC-α and ENaC-γ mRNA expression in the kidney.
Discussion
The present study provides the first demonstration that nesf/NUCB2 overexpression increases blood pressure without affecting PR in mice. Overexpression of nesf/NUCB2 in the brain and kidney was confirmed at the protein and mRNA levels in the present study, but serum nesfatin-1 concentration was not increased in Tg mice.15 Therefore, circulating nesfatin-1 may not have an important role in the present results and intracellular overexpression of nesf/NUCB2 in the hypothalamus or kidney may be involved in an increase of blood pressure.
First, we demonstrated that SBP, MBP and DBP were significantly higher in nesf/NUCB2-Tg mice than in their non-Tg littermates in a conscious condition, findings in agreement with results of a previous study reporting that hypothalamic nesfatin-1 stimulates sympathetic nerve activity.18 Notably, isoflurane anesthesia canceled an increase in blood pressure in Tg mice, thus suggesting potential involvement of the central nervous system. The main aim of assessing blood pressure in the unconscious condition induced by isoflurane was to exclude effects of sympathetic activation resulting from restriction stress during the blood pressure measurement. One study has reported that a full sympathetic activation occurs in conscious mice undergoing restriction stress, whereas anesthesia is associated with complete sympathetic withdrawal.19 However, effects of isoflurane on hemodynamics must be considered in the interpretation of our findings. A previous study has reported that the effects of isoflurane on systemic hemodynamics are concentration dependent: higher isoflurane concentration results in an elevated heart rate and reduced blood pressure.20 In the present study, to minimize isoflurane-induced changes in hemodynamics, we used a very low concentration of isoflurane. The blood pressure in non-nesf/NUCB2-Tg mice was similar in the conscious and unconscious (anesthetized) conditions, whereas the PR was ~10% lower in the unconscious condition than in the conscious condition. These findings indicated that the hemodynamic effects of isoflurane were minimal. In contrast to increased blood pressure, PR was not comparable between non-nesf/NUCB2-Tg and Tg mice. Given that PR was decreased under isoflurane anesthesia, restriction stress-induced activation of the parasympathetic nervous system may have masked central nesf/NUCB2 effects on PR. Measurement of sympathetic nerve activity under restriction stress may be necessary to finally conclude the possible involvement of sympathetic nerve activity in these mice.
ENaC is expressed in brain regions implicated as cardiovascular regulatory centers.21 Immuno-reactivity to ENaC-γ has also been demonstrated to be present in many magnocellular neurons in the supraoptic nucleus of the hypothalamus and to co-localize with vasopressin, but not oxytocin.22 We have previously demonstrated the expression of nesf/NUCB2 in the supraoptic nuclei of the hypothalamus.1 The present finding that ENaC-γ mRNA expression was decreased in the hypothalamus may be associated with the observed increase in blood pressure in nesf/NUCB2-Tg mice.
In addition, our recent study has demonstrated a selective expression of nesf/NUCB2 in the vascular endothelial cells of arteries, but not in vascular smooth muscle cells.12 Nesfatin-1 has been shown to modulate blood pressure by acting directly on peripheral arterial resistance.23 Alternatively, overexpressed nesf/NUCB2 in vascular endothelial cells may function in a paracrine manner and accelerate the contraction of vascular smooth muscle cells in the vessels of those animals, although an increase of circulating nesfatin-1 was not found in nesf/NUCB2-Tg mice, and anesthesia by isoflurane, which has fewer systemic hemodynamic effects in mice,24 blocked the increase in blood pressure.
The present study demonstrated that nesf/NUCB2-Tg mice showed a significant increase in water intake and urine volume. Immunohistochemical analysis for nesf/NUCB2 has revealed that nesfatin-1/NucB2 protein levels are increased after 48 h of dehydration and attenuated by 24 h of rehydration,25 thus indicating that an increase in nesf/NUCB2 expression in the hypothalamus may stimulate water intake and that nesf/NUCB2 may be involved in the regulation of water intake by the hypothalamus. An increase in intracellular nesf/NUCB2 expression in the hypothalamus may cause an increase in water intake in nesf/NUCB2-Tg mice. In addition, urine sodium concentration was significantly lower in nesf/NUCB2-Tg mice, thereby indicating an increase in sodium reuptake in renal tubules, although total urinary sodium excretion for 24 h was not significantly changed in nesf/NUCB2-Tg mice. We have recently demonstrated that nesf/NUCB2 is selectively co-expressed with ENaC in renal collecting ductal cells.12 However, overexpression of nesf/NUCB in the kidney did not affect renal ENaC-α and ENaC-γ mRNA expression. Serum aldosterone and arginine vasopressin concentrations were not significantly changed in the Tg mice. Renal sympathetic nerve activity has been reported to be involved in the regulation of renal tubular sodium re-absorption.26 An increase in urine volume due to increased water intake and supposed modulation of renal sympathetic nerve activity may explain the observed reduction in urine sodium concentration in nesf/NUCB2-Tg mice. Furthermore, a recent study has demonstrated that renal sympathetic denervation and β-adrenergic blockade by bisprolol decreases renal weight in Dahl salt-sensitive hypertensive rats,27 thus indicating possible involvement of renal sympathetic nerve activity in the increase in kidney size in nesf/NUCB2-Tg mice.
A limitation of the present study is that we did not assess the specific location in which expressed ENaC and nesf/NUCB2 are upregulated in the hypothalami of nesf/NUCB2-Tg mice and the exact mechanism could not be conclusively clarified in the present experiments. Another limitation is the lack of data about diurnal variation in blood pressure. Non-invasive methods of blood pressure measurement, including the tail cuff method, which we used in the present study, have certain limitations in evaluating diurnal blood pressure variation.28 Although our data that were taken during the conscious and unconscious conditions may represent diurnal blood pressure variation induced by changes in sympathetic and parasympathetic nervous system activation to some extent, further studies using invasive methods of blood pressure measurement, such as radiotelemetry implantation and fluid-filled catheter insertion, are necessary to obtain further insight into the role of central nesf/NUCB2 in the activation of the sympathetic nervous system.
The data obtained herein indicated that nesf/NUCB2 is involved in the regulation of blood pressure in the conscious condition and in regulation of water and sodium metabolism in the kidney. Overexpression of nesf/NUCB2 may increase blood pressure by the activation of the sympathetic nervous system in the brain and by reducing sodium reuptake in the kidney. As overproduction of nesf/NUCB2 has been found in adipose tissue of high-fat diet-fed mice,8 the reduction of nesf/NUCB2 expression may contribute to the improvement of hypertension in obese people.
References
Oh-I S, Shimizu H, Satoh T, Okada S, Adachi S, Inoue K, Eguchi H, Yamamoto M, Imaki T, Hashimoto K, Tsuchiya T, Monden T, Horiguchi K, Yamada M, Mori M . Identification of nesfatin-1 as a satiety molecule in the hypothalamus. Nature 2006; 443: 709–712.
Osaki A, Shimizu H, Ishizuka N, Suzuki Y, Mori M, Inoue S . Enhanced expression of nesfatin/nucleobindin-2 (NUCB2) in white adipose tissue of ventromedial hypothalamus (VMH)-lesioned rats. Neurosci Lett 2012; 521: 46–51.
Price TO, Samson WK, Niehoff ML, Banks WA . Permeability of the blood-brain barrier to a novel satiety molecule nesfatin-1. Peptides 2007; 28: 2372–2381.
Pan W, Hsuchou H, Kastin AJ . Nesfatin-1 crosses the blood-brain barrier without saturation. Peptides 2007; 28: 2223–2228.
Shimizu H, Oh-I S, Hashimoto K, Nakata M, Yamamoto S, Yoshida N, Eguchi H, Kato I, Inoue K, Satoh T, Okada K, Yamada M, Yada T, Mori M . Peripheral administration of nesfatin-1 reduces food intake in mice: the leptin-independent mechanism. Endocrinology 2009; 150: 662–671.
Yosten GL, Samson WK . The anorexigenic and hypertensive effects of nesfatin-1 are reversed by pretreatment with an oxytocin receptor antagonist. Am J Physiol Integr Comp Physiol 2010; 298: R1642–R1647.
Yosten GL, Samson WK . Nesfatin-1 exerts cardiovascular actions in brain: possible interaction with the central melanocortin system. Am J Physiol Integr Comp Physiol 2009; 297: R330–R336.
Osaki A, Shimizu H . Peripheral administration of nesfatin-1 increases blood pressure in mice. Hypertens Res 2013; 37: 185–186.
Ramanjaneya M, Chen J, Brown JE, Tripathi G, Hallschmid M, Patel S, Kern W, Hillhouse EW, Lehnert H, Tan BK, Randdeva HS . Identification of nesfatin-1 in human and murine adipose tissue: a novel depot-specific adipokine with increased levels in obesity. Endocrinology 2010; 151: 3169–3180.
Kir SF, Baydur SS, Mete UU, Cumhur CM, Senturk S, Bayoglu TY, Balik G, Cure E, Yuce S, Kirbas A . Nesfatin-1 and Vitamin D levels may be associated with systolic and diastolic blood pressure values and heart rate in polycystic ovary syndrome. Bosn J Basic Med Sci 2015; 15: 57–63.
Shimizu H, Osaki A . Possible involvement of anorexigenic protein, nesfatin/nucleobindin-2 (NUCB2) in blood pressure regulation by regulating water reabsorption in renal collecting duct. J Cytol Histol 2014; 5: 290.
Boivin V, Jahns R, Gambaryan S, Ness W, Boege F, Lohse MJ . Immunofluorescent imaging of beta 1- and beta 2-adrenergic receptors in rat kidney. Kidney Int 2001; 59: 515–531.
DiBona GF . Physiology in perspective: the wisdom of the body. Neural control of the kidney. Am J Physiol Regul Integr Comp Physiol 2005; 289: R633–R641.
Wallace DP, Reif G, Hedge A-M, Thrasher JB, Pietroe P . Adrenergic regulation of salt and fluid secretion in human medullary collecting duct cells. Am J Physiol Renal Physiol 2004; 287: F639–F648.
Shimizu H, Tanaka M, Osaki A . Transgenic mice overexpressing nesfatin/nucleobindin-2 are susceptible to high-fat diet-induced obesity. Nutr Diabetes 2016; 6: e201.
Kubota Y, Umegaki K, Kagota S, Tanaka N, Nakamura K, Kunitomo M, Shinozuka K . Evaluation of blood pressure measured by tail-cuff (without heating) in spontaneously hypertensive rats. Biol Pharm Bull 2006; 29: 1756–1758.
Shimada T, Takeshita Y, Murohara T, Sasaki K, Egami K, Shintani S, Katsuda Y, Ikeda H . Angiogenesis and vasculogenesis are impaired in the precocious-aging klotho mouse. Circulation 2004; 110: 1148–1155.
Tanida M, Gotoh H, Yamamoto N, Wang M, Kuda Y, Kurata Y, Mori M, Shibamoto T . Hypothalamic nesfatin-1 stimulates sympathetic nerve activity via hypothalamic ERK signaling. Diabetes 2015; 64: 3725–3736.
Tan TP, Gao XM, Krawczyszyn M, Feng X, Kiriazis H, Dart AM, Du XJ . Assessment of cardiac function by echocardiography in conscious and anesthetized mice: importance of the autonomic nervous system and disease state. J Cardiovasc Pharmacol 2003; 42: 182–190.
Constantinides C, Mean R, Janssen BJ . Effects of isoflurane anesthesia on the cardiovascular function of the C57BL/6 mouse. ILAR J 2011; 52: e21–e31.
Amin MS, Wang HW, Reza E, Whitman SC, Tuana BS, Leenen FH . Distribution of epithelial sodium channels and mineralocorticoid receptors in cardiovascular regulatory centers in rat brain. Am J PhysiolRegul Integr Comp Physiol 2005; 289: R1787–R1797.
Teruyama R, Sakuraba M, Wilson LL, Wandrey EJ, Armstrong WE . Epithelial Na+ sodium channels in magnocellular cells of the rat supraoptic and paraventricular nuclei. Am J Physiol Endocrinol Metab 2012; 302: E273–E285.
Yamawaki H, Takahashi M, Mukohda M, Pkada M, Hara Y . A novel adipocytokine, nesfatin-1 modulates peripheral arterial contractility and blood pressure in rats. Biochem Biophys Res Commun 2012; 418: 676–681.
Janssen BJA, De Celle T, Debets JJM, Brouns AE, Callahan MF, Smith TL . Effects of anesthesia on systemic hemodynamics in mice. Am J Physiol Heart Circ Physiol 2003; 287: H1618–H1624.
Yoshimura M, Matsuura T, Ohkubo J, Maruyama T, Ishikura T, Hashimoto H, Kakuma T, Mori M, Ueta Y . A role of nesfatin-1/NucB2 in dehydration-induced anorexia. Am J Physiol Regul Integr Comp Physiol 2014; 307: R225–R236.
Li J, He Q, Wu W, Li Q, Huang R, Pan X, Lai W . Role of the renal sympathetic nerves in renal sodium/potassium handling and renal damage in spontaneously hypertensive rats. Exp Ther Med 2016; 12: 2547–2553.
Watanabe H, Iwanaga Y, Miyaji Y, Yamamoto H, Miyazaki S . Renal denervation mitigates cardiac remodeling and renal damage in Dahl rats: a comparison with β-blockade. Hypertens Res 2016; 39: 217–226.
Kurtz TW, Griffin KA, Bidani AK, Davisson RL, Hall JE Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Recommendations for blood pressure measurement in humans and experimental animals: part 2: blood pressure measurement in experimental animals: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Arterioscler Thromb Vasc Biol 2005; 25: e22–e33.
Acknowledgements
This work was supported in part by the Japanese Ministry of Education, Culture, Sports, Science and Technology, Grant-in-Aid for Scientific Research on Innovative Areas (Research in a proposed research area) ‘Molecular Basis and Disorders of Control of Appetite and Fat accumulation’ to HS.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Mori, Y., Shimizu, H., Kushima, H. et al. Increased blood pressure in nesfatin/nuclebindin-2-transgenic mice. Hypertens Res 40, 861–867 (2017). https://doi.org/10.1038/hr.2017.61
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2017.61