Abstract
The most common classifications of hypertensive disorders of pregnancy consist of chronic hypertension, gestational hypertension, preeclampsia (PE) and superimposed PE. A common final pathophysiology of PE is endothelial dysfunction. The most successful translational research model for explaining the cause–effect relationship in the genesis of PE is the angiogenic/angiostatic balance theory, involving soluble fms-like tyrosine kinase 1 (sFlt-1), placental growth factor (PlGF) and soluble endoglin (sEng). In a systematic review of articles on the prediction of early-onset PE using angiogenesis-related factors, we revealed that the prediction of early-onset PE in the first trimester is clinically possible, but the prediction of early-onset PE in the early third trimester might be ideal. In addition, an onset threshold or a serial approach appeared to be clinically useful for predicting the imminent onset of PE, with onset at <4 weeks after blood sampling in the second and early third trimesters, because the positive likelihood ratio was >10 and the positive predictive value was >20%. The National Institute for Health and Care Excellence guidelines state that the Triage PlGF testing and Elecsys immunoassay for the sFlt-1/PlGF ratio could help to exclude PE in women with suspected PE at 20–34 weeks of gestation. Until now, we have not found any effective therapies to prevent PE. However, low-dose aspirin treatment starting at ⩽16 weeks of gestation might be associated with a marked reduction in PE. In addition, early statin treatment might prevent the occurrence of PE. Currently, a clinical trial using pravastatin for the prevention of PE is ongoing.
Similar content being viewed by others
Introduction
Preeclampsia (PE) is a major complication of pregnancy associated with significant morbidity and mortality for both the fetus and mother.1, 2 Hypertensive disorders of pregnancy (HDP) consist of the following four diseases: chronic hypertension, gestational hypertension (GH), PE and superimposed PE; however, PE has been mostly studied for its prediction and prevention. In this review, we focused on the risk factors for PE in antepartum booking, prediction of PE using uterine artery flow velocity waveforms or circulating levels of angiogenesis-related factors and prevention of PE.
Classification of hypertensive disorders of pregnancy
There are several guidelines for the management of hypertensive disorders in pregnancy. Between 2013 and 2014, four major societies, including the American College of Obstetricians and Gynecologists, the Society of Obstetricians and Gynaecologists of Canada, the Society of Obstetric Medicine of Australia and New Zealand, and the International Society for the Study of Hypertension in Pregnancy (ISSHP), revised their guidelines.3, 4, 5, 6 The common points were as follows: (1) the use of the generic term ‘hypertensive disorders of pregnancy’; (2) the inclusion of chronic hypertension in the classification of HDPs; (3) the inclusion of a clinical definition of PE, such as GH and impaired liver function but not new proteinuria; and (4) the inclusion of a clinical definition of superimposed PE, such as chronic hypertension and impaired liver function but not new proteinuria. Although the Japan Society for the Study of Hypertension in Pregnancy (JSSHP) classified pregnancy-induced hypertension in 2004, the four common aforementioned points in the recent guidelines were not considered.7, 8 The JSSHP has established a committee for the revision of the guidelines for the management of pregnancy-induced hypertension; in May 2016, the committee decided to change the name of pregnancy-induced hypertension to HDPs and include chronic hypertension in the classification of HDPs. The details of the guidelines for the management of HDPs are provided chronologically in Supplementary Table S1.
The most common classifications of HDPs consist of the following four diseases: chronic hypertension, GH, PE and superimposed PE;3, 4, 5, 6, 9, 10, 11, 12 however, the Japanese classification of HDP does not include chronic hypertension,7, 8 and the National Institute for Health and Care Excellence (NICE) classification of HDP does not include superimposed PE.13 The definitions of edema, proteinuria and hypertensive disorders in pregnancy, childbirth and the puerperium by the International Statistical Classification of Diseases and Related Health Problems (ICD)-10 have also been used in several clinical research studies,14 and these definitions also include the four common classifications.15 Therefore, in this review, we defined HDPs as chronic hypertension, GH, PE and superimposed PE. Recent classifications of HDPs have commonly defined PE as hypertension with a new onset of at least one of the following: proteinuria, renal insufficiency, impaired liver function, neurological complications or hematological complications (clinical definition of PE),3, 4, 5, 6, 9, 12 although the old ISSHP guidelines, JSSHP classification, NICE guidelines and ICD-10 classification used narrow definitions of PE, de novo hypertension, and de novo proteinuria.7, 8, 11, 13, 15 However, in the current review, we did not distinguish between the clinical definition of PE and the narrower definitions of PE.
The JSSHP defined GH or PE occurring at <32 weeks of gestation as the early-onset type,7, 8 because the distributions of severe early-onset pregnancy-induced hypertension and severe late-onset pregnancy-induced hypertension showed bimodal distributions with peaks at 30–31 and 34–35 weeks of gestation, respectively.16 In a recent statement about the definition of severe and early-onset PE, most investigators considered early-onset PE to occur before 34 weeks of gestation.17 Early-onset PE differs from late-onset PE in terms of maternal mortality, pathophysiology, recurrence in later pregnancies, risk of later cardiovascular disease and death, and the occurrence of fetal growth restrictions.18 In addition, it was disclosed that an abnormal increase in soluble fms-like tyrosine kinase 1 (sFlt-1) and an abnormal decrease in placental growth factor (PlGF) frequently occurred in preeclamptic women with an onset at <34 weeks of gestation.19, 20
Risk factors on antenatal booking
There are many risk factors for the occurrence of PE. The early detection of high-risk factors for PE could allow for improvement of the outcome by increasing patient surveillance or by prescribing drugs to prevent the occurrence of PE. Therefore, it is very important to know whether a pregnant woman has some risk factors for PE at the first visit for an antenatal maternal checkup. In a systematic review of the risk factors for PE on antenatal booking, using 52 cohort and case–control studies from 1966 to 2002, the risk factors (unadjusted relative risk (RR)) were as follows: antiphospholipid antibodies (9.7), preexisting diabetes (3.6), previous PE (7.2), family history of PE (2.9), nulliparity (2.9), twins (2.9), obesity (2.5), high systolic blood pressure ⩾130 mm Hg (vs. <130 mm Hg); (2.4), age ⩾40 (multipara); (2.0) and age ⩾40 (primipara); (1.7).21 Recently, 14 clinical risk factors at ⩽16 weeks of gestation for the development of PE were evaluated involving almost 25 million pregnancies in 92 cohort studies from 2000 to June 2015.14 The risk factors (unadjusted RR) were as follows: prior intrauterine growth restriction (1.4, but not significant), systemic lupus erythematosus (2.5), nulliparity (2.1), age ⩾35 (1.2), age ⩾40 (1.5), prior stillbirth (2.4), chronic kidney disease (1.8), assisted reproductive technology (1.8), prepregnancy body mass index ⩾25 (2.1), prepregnancy body mass index ⩾30 (2.8), multifetal pregnancy (2.9), prior placental abruption (2.0), pregestational diabetes (3.7), prior PE (8.4), chronic hypertension (5.1) and antiphospholipid antibodies (2.8). The results of the recent systematic review mostly confirmed the previous results for nulliparity, age ⩾40, obesity, diabetes, prior PE and antiphospholipid antibodies, and it additionally revealed that systematic lupus erythematosus, prior stillbirth, chronic kidney disease, assisted reproductive technology, prior placental abruption and chronic hypertension were high-risk factors for PE.
Although nulliparity is a well-known risk factor for PE, the multiparous effect disappeared if the time between pregnancies was 10 years or more.22 In addition, several studies have reported that the incidence of PE in a second pregnancy with a new partner is almost the same as that in the first pregnancy with the previous partner.23 However, the incidence rate of PE in the second pregnancy is very different in women with/without PE in the first pregnancy. Then, we systemically reviewed whether pregnant women with a new partner in the second pregnancy developed PE more frequently than those with the same partner in the second pregnancy who did not develop PE in the first pregnancy.24 In the four cohorts with 601 365 pregnant women who did not have PE in the first pregnancy, women with a new partner developed PE at a rate of 2.0%, whereas women with the same partner developed PE at a rate of 1.5% (P<0.001),25, 26, 27, 28 indicating that a change of paternity could increase the occurrence of PE.
Pathophysiology of PE
Endothelial dysfunction
A common final pathophysiology of PE is endothelial dysfunction. Many observations have confirmed the presence of endothelial dysfunction in PE.29 Increased sensitivity to angiotensin II precedes the clinical manifestation of PE by weeks to months.30 Glomerular endotheliosis is morphological evidence of endothelial injury.31 The levels of von Willebrand factor and fibronectin were increased in women with later occurrence of PE than in normal pregnant women in the second and third trimesters.32 Actually, serum samples obtained before delivery in women with PE affected the endothelial cell function in human umbilical vein endothelial cells in culture.29 Tsukimori et al.33 investigated endothelial cell injury by the release of radiolabeled chromium from human umbilical vein endothelial cells into culture medium; although the release of chromium 51 in PE was almost twice that in normal pregnancy, the levels in GH and chronic hypertension were not significantly different from those in normal pregnancy. Tsukimori et al.34 also demonstrated that neutrophils from women with PE adhered more markedly to human umbilical vein endothelial cells than those from nonpregnant or normal pregnant women; the increased neutrophil-endothelial adhesion in PE was inhibited by pretreatment with anti-CD11b, the expression of which in neutrophils in PE was significantly increased compared with that in normal pregnancy, indicating an important role of CD11b in the adhesion of neutrophils to endothelial cells. It was demonstrated that neutrophils actually infiltrate resistance-sized vessels in women with PE.35 Vessel reactivity to angiotensin II in endothelium-intact omental arteries obtained from preeclamptic women was significantly increased, compared with that in normal pregnant women; however, the enhanced vessel reactivity to angiotensin II in PE was blocked by pretreatment with superoxide dismutase/catalase or RhoA kinase inhibitor.36 These results suggested a role of activated neutrophils in the genesis of endothelial dysfunction and enhanced vasoconstriction in PE. However, it is not known whether increased sFlt-1 levels in PE are related to the activation of neutrophils.
Animal models of PE
The most successful model of translational research from bench to bed for explaining the cause–effect relationship in the genesis of PE is the angiogenic/angiostatic balance theory involving sFlt-1, PlGF and sEng. In 2003, the role of sFlt-1 in the genesis of PE was discovered in a rat model,37 followed by the discovery of sEng having an additive effect on the genesis of PE in a rat model.38 Soon after these two basic research studies, it was discovered that sFlt-1, PlGF and sEng showed changes 3–4 months before the clinical onset of PE. The circulating levels of sFlt-1 were increased 9–11 weeks before the onset of PE.19 The circulating levels of PlGF were decreased 9–11 weeks before the onset of PE and showed a marked decrease during the 5 weeks before the onset of PE.19 In addition, the circulating levels of sEng were increased 9–11 weeks before the onset of preterm PE and 12–14 weeks before the onset of term PE, although the magnitude of the increase was less marked in term than in preterm PE.39 However, the balance theory has a serious limitation because these markers do not have high positive likelihood ratios (LR+) for predicting late-onset PE, especially at ⩾36 weeks of gestation,40 and because the increased levels of sFlt-1 and sEng were not observed in some cases of PE.20, 41 Therefore, we searched for other animal models of PE and investigated whether there were some new candidates for biomarkers that are possible causes of the animal models of PE.42 We collected 64 articles on animal models of PE, consisting of 25 different methods. Angiotensinogen in the first trimester, prorenin at 8 weeks of gestation in women with Type 1 diabetes and plasma prorenin receptor in early pregnancy might predict the occurrence of PE. Low galectin-1 levels during the second trimester might predict the later occurrence of PE. Interleukin-10 levels did not change before the onset of PE. Maternal plasma asymmetric dimethylarginine in the second and third trimesters was higher in women with PE. However, we could not find any cohort or nested case–control studies of complement component C1q, 2-methoxyoestradiol/catechol-O-methyltransferase or heme oxygenase-1.
Two-stage model
PE occurs mainly during pregnancy and rarely immediately after delivery, and it disappears soon after the cessation of pregnancy, indicating that the placenta is the main cause of the development of PE. In the current understanding of the genesis of PE, there is the two-stage model proposed by Roberts and Hubel43 as follows: the first stage is reduced placental perfusion owing to abnormal implantation or other pathological disorders, and the second stage is the production of endothelial dysfunction, and the appearance of maternal hypertension and proteinuria caused by a maternal response to the reduced placental perfusion. This model almost completely applies to the development of early-onset PE, which was associated with abnormal uterine artery Doppler (UAD) findings in the first and second trimesters,44 and was also associated with an abnormal decrease in PlGF or an abnormal increase in the sFlt-1/PlGF ratio in the second and third trimesters.40 In contrast, late-onset PE often lacks abnormal uterine Doppler findings in the first and second trimesters,44 or sometimes shows normal PlGF or a normal sFlt-1/PlGF ratio at the onset of PE.20 Therefore, regarding late-onset PE, the novel concept of ‘maternal PE’ was proposed by Redman and Sargent.45 Arterial diseases owing to autoimmune disorders, chronic hypertension, obesity or preexisting diabetes involve microvascular lesions accompanied by low-grade systemic inflammation, which could contribute to the development of endothelial dysfunction during pregnancy. However, in most cases of PE, maternal and placental factors are mixed.
Prediction
Prediction of PE in the first, second and early third trimesters
In this review of risk factors in the first, second and early third trimesters, we considered an LR+ of ⩾10 and positive predictive value (PPV) of ⩾20% to be clinically useful predictive markers.
Failure of extra-trophoblast invasion of the uterine spiral arteries has often been observed in PE.46, 47, 48, 49 Shallow invasion of the extra trophoblasts into the spiral arteries has actually been associated with increased resistance by UAD velocity.50 The detection rates of the abnormal uterine artery pulsatility index at 23 weeks of gestation were increased when the weeks at delivery were earlier in women with PE, indicating that screening for early-onset PE using UAD might be more accurate than screening for late-onset PE.51 Thereafter, many studies for predicting early-onset PE using the various findings of UAD in the first and second trimesters have been reported.
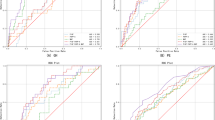
When early-onset PE was not distinguished from other types of PE, it is disappointing that the screening properties for various Doppler indices in the first and second trimesters showed LR+ of <10 as predictive all-PE in the meta-analysis.52 Because abnormal UAD findings are frequently observed in women with a later occurrence of early-onset PE, it is more logical to apply the UAD screening to predict only early-onset PE. We summarized the prediction of early-onset PE using UAD alone in a systematic review.44 In this systematic review, 40 articles with sensitivity and false-positive rate (FPR) data were finally used to calculate LR+, and post-test probability for predicting early-onset PE. In unselected low-risk women, UAD alone could predict early-onset PE in the first and second trimesters with an LR+ of ⩾10 (Supplementary Table S2).53, 54, 55, 56, 57, 58, 59, 60, 61, 62 In particular, UAD alone in the second trimester in high-risk women yielded a post-test probability of >0.20 in one study, and in another study, the post-test probability was close to 0.20 (0.194); (Supplementary Table S2).63, 64 We constructed a regression line between FPR and sensitivity in the first and second trimesters; at a cutoff level of 5% FPR in unselected or low-risk women, the average LR+ in the first and second trimesters was 11.2 and 11.0, respectively (Figure 1).
Scatter plot showing the relationship between the false-positive rate (FPR) and the sensitivity to predict early-onset preeclampsia (PE) by uterine artery Doppler (UAD) alone in the first trimester (a) and UAD alone in the second trimester (b). Closed circles indicate unselected or low-risk women, and closed triangles indicate high-risk women. When the FPR was <10%, the regression line of the sensitivity of FPR, including 0% FPR and 0% sensitivity, was plotted in unselected or low-risk women, and, when the FPR was ⩾10%, the regression line of the sensitivity on FPR, including 100% FPR and 100% sensitivity, was plotted in unselected or low-risk women.
Until now, many molecules have been investigated as candidate biomarkers for predicting the onset of PE.65, 66, 67 The conclusions of a recent systematic review were all pessimistic because no single biomarkers could predict the occurrence of HDP or PE with a high LR+.65, 66 However, Forest et al.67 stated that combinations of antenatal risk factors, clinical parameters, and biophysical and biochemical markers were promising. For example, Akolekar et al.68 reported that the sensitivity to predict early, intermediate and late PE under conditions of an FPR of 5% was 91.0%, 79.5% and 60.9%, respectively, when maternal factors, two biophysical markers (uterine artery pulsatility index and mean arterial pressure) and eight biomarkers (pregnancy-associated plasma protein-A, PlGF, placental protein-13, sEng, inhibin-A, activin-A, pentraxin-3 and p-selectin) at 11–13 weeks of gestation were used in a multivariate model. In this model, the LR+ was always >10 for predicting early, intermediate and late PE, indicating that all cases of PE could be detected if we used multiple risk factors simultaneously. However, in light of clinical practice, the fewer the combinations of risk factors that there are, the less expense the cost of screening will be.
As shown in the ‘Animal models of PE’ section, the angiogenic/angiostatic balance theory involving sFlt-1, PlGF and sEng has been the most successful model explaining the genesis of PE. Therefore, many clinical studies to predict PE using sFlt-1, PlGF and sEng have been reported. In a recent review of angiogenesis-related factors for predicting PE, it was concluded that the test accuracy of these biomarkers was too low for the accurate prediction of PE in clinical practice.69 However, the increase in sFlt-1 and sEng, and decrease in PlGF are phenomena mainly related to early-onset PE.20 Therefore, we summarized the predictions of early-onset PE using angiogenesis-related factors alone, or the combined use of angiogenesis-related and other risk factors.40 Twenty-one articles with sensitivity and FPR data were used. For the prediction of early-onset PE with angiogenesis-related factors alone, in unselected or low-risk women, PlGF alone in the first and second trimesters could predict early-onset PE with an LR+ of ⩾10;70, 71, 72, 73, 74 the sFlt-1/PlGF ratio at 19–25 weeks of gestation71 and at 24 week of gestation73 could predict early-onset PE with an LR+ of ⩾10 (Supplementary Table S3). In high-risk women, the sFlt-1/PlGF ratio at 23 weeks of gestation,63 sEng at 19–24 weeks of gestation64 and sFlt-1 at 28–31 weeks of gestation75 could predict early-onset PE with an LR+ of ⩾10 (Supplementary Table S3). We constructed a regression line between FPR and sensitivity in various settings; with a cutoff level of 5% FPR in unselected or low-risk women, PlGF in the first trimester, PlGF in the second trimester, and the sFlt-1/PlGF ratio in the second trimester yielded an average LR+ of 6.8, 14.6 and 12.7, respectively (Figure 2). Regarding the prediction of early-onset PE with the combination of angiogenesis-related and other risk factors, in unselected or low-risk women, PlGF with other risk factors in the first trimester could predict early-onset PE with an LR+ of ⩾10;54, 68, 70, 76, 77, 78, 79, 80 and the sFlt-1/PlGF ratio with other risk factors in the second or early third trimester could predict early-onset PE with an LR+ of ⩾10 (Supplementary Table S4).72, 73 We constructed a regression line between FPR and sensitivity for the combined methods in the first, second and early third trimesters; at the cutoff level of 5% FPR in unselected or low-risk women, the average LR+ in the first, second and early third trimesters was 13.2, 14.6 and 25.4, respectively (Figure 3). These results suggested that the prediction of early-onset PE in the first trimester was clinically possible, but the prediction of early-onset PE in the early third trimester might be the best. We recently reported the effect of the onset threshold, on the basis of the distribution of biomarkers in women with PE but not the distribution of biomarkers in normal pregnant women, on the prediction of imminent onset of PE within 4 weeks after blood sampling.71 The sensitivity, specificity, LR+ (95% confidence interval (CI)), PPV and negative predictive value (NPV) of the sFlt-1/PlGF ratio over the onset threshold for predicting PE with an onset at <4 weeks after blood sampling at 19–25 weeks were 100%, 100%, >1000, 100%, and 100%, respectively; those for predicting PE with an onset at <4 weeks after blood sampling at 26–31 weeks were 83%, 99.4%, 132 (95% CI: 51–339), 50%, and 99.9%, respectively, indicating that the onset threshold, on the basis of distribution of the sFlt-1/PlGF ratio in women with PE, but not the abnormal threshold on the basis of normal reference range of sFlt-1/PlGF ratio in normal pregnant women, was a promising cutoff level for predicting the imminent onset of PE soon after blood sampling in the second and early third trimesters (Figure 4). We also devised a novel prediction model on the basis of a three-step approach by sequential selection using maternal factors, including a past history of PE/GH or blood pressure levels ⩾120/80 mm Hg at 16–23 weeks (first step), followed by plasma levels of PlGF in the <5th percentile (second step) and plasma levels of sFlt-1 in the ⩾95th percentile (third step).81 The sensitivity, specificity, LR+ (95% CI), PPV and NPV of the three-step approach for predicting PE with an onset at <4 weeks after blood sampling at 19–25 weeks were 100%, 99.8%, 599 (150–2390), 50% and 100%, respectively; those at 26–31 weeks were 83%, 99.1%, 94 (42–214), 42% and 99.9%, respectively (Figure 5). These results indicated the following: (1) the three-step approach markedly improved the LR+ from 2.6 (first step) to 94 (third step) and the PPV from 1.9% (first step) to 42% (third step); (2) the three-step approach could exclude almost 98% of women with very high NPV of 99.9–100%; and (3) the three-step approach yielded a cost reduction of 78%, compared with an approach for measuring both sFlt-1 and PlGF in all subjects. Taken together, the onset threshold or three-step approach appeared to be clinically useful for predicting the imminent onset of PE with onset at <4 weeks after blood sampling in the second and early third trimesters because the LR+ was >10, and the PPV was >20%.
Scatter plot showing the relationship between FPR and sensitivity to predict early-onset PE by placental growth factor (PlGF) alone in the first trimester (a), PlGF alone in the second trimester (b) and the soluble fms-like tyrosine kinase 1 (sFlt-1)/PlGF ratio alone in the second trimester (c). Closed circles indicate unselected or low-risk women, and closed triangles indicate high-risk women. When the FPR was <10%, the regression line of the sensitivity of FPR, including 0% FPR and 0% sensitivity, was plotted in unselected or low-risk women, and, when the FPR was ⩾10%, the regression line of the sensitivity on FPR, including 100% FPR and 100% sensitivity, was plotted in unselected or low-risk women. FPR, false-positive rate; PE, preeclampsia.
Scatter plot showing the relationship between FPR and the sensitivity to predict early-onset PE by the combined use of angiogenesis-related factors and other risk factors in the first trimester (a), the second trimester (b) and the early third trimester (c). Closed circles indicate unselected or low-risk women. When the FPR was <10%, the regression line of the sensitivity of FPR, including 0% FPR and 0% sensitivity, was plotted in unselected or low-risk women, and, when the FPR was ⩾10%, the regression line of the sensitivity on FPR, including 100% FPR and 100% sensitivity, was plotted in unselected or low-risk women. FPR, false-positive rate; PE, preeclampsia.
Prediction of the imminent onset of PE using the onset threshold of the sFlt-1/PlGF ratio. The meanings of the symbols are presented in the figure. (a) The thin straight curves represent the 5th and 95th percentiles of the reference range of the sFlt-1/PlGF ratio, and the thick curve represents the mean of the normal reference range of the sFlt-1/PlGF ratio. The dashed and dotted curve represents the onset threshold. The raw values of the sFlt-1/PlGF ratio after the onset of PE are shown. (b, c) Thick straight lines represent the 5th and 95th percentiles of the distribution of log10(sFlt-1/PlGF) in 1155 normal pregnant women at 19–25 weeks of gestation and 769 normal pregnant women at 26–31 weeks of gestation in a prospective cohort study. The dashed and dotted curve represents the onset threshold. In b, the raw values of the sFlt-1/PlGF ratio before the onset of PE are shown; cases with the onset of PE within 4 weeks after blood sampling are indicated by closed circles. In c, the raw values of the sFlt-1/PlGF ratio in normal pregnant women and those with gestational hypertension are shown. PE, preeclampsia; PlGF, placental growth factor; sFlt-1, soluble fms-like tyrosine kinase 1.
Prediction of the imminent onset of PE using the three-step approach. The meanings of the symbols are presented in the figure. (a) True-positive cases for predicting the imminent onset of PE using sFlt-1 levels are shown as closed triangles, whereas false-positive cases are shown as closed circles. Thick straight lines represent the 5th and 95th percentiles of the distribution of log10sFlt-1. (b) True-positive cases for predicting the imminent onset of PE using PlGF levels are shown as closed triangles, whereas false-positive cases are shown as closed circles. Thick straight lines represent the 5th and 95th percentiles of the distribution of log10PlGF. (c) The changes of LR+ by the three-step approach. The lines show the effects of the three-step approach (maternal factors (first step)→PlGF (second step) →sFlt-1 (third step)) on the marked changes in the LR+ for predicting the imminent onset of PE at 19–25 weeks (open triangles) and 26–31 weeks (open circles). (d) The changes in PPV by the three-step approach. The lines show the effects of the three-step approach (first step→second step→third step) on the marked changes in the PPV for predicting the imminent onset of PE at 19–25 weeks (open triangles) and 26–31 weeks (open circles). LR+, positive likelihood ratio; PE, preeclampsia; PlGF, placental growth factor; PPV, positive predictive value; sFlt-1, soluble fms-like tyrosine kinase 1.
Prediction of PE in women with suspected PE
The most important issue for the prediction of PE is whether the method of prediction is clinically useful, in other words, whether there are any effective treatments to prevent the occurrence of PE. However, almost all of the large clinical trials evaluating the prevention of PE with several drugs have failed to identify any clinically significant values.82, 83, 84 In addition, practitioners' interest has shifted to the use of the biomarkers to triage high-risk pregnant women, such as those with gestational proteinuria or GH. Rana et al.85 found that a circulating sFlt-1/PlGF ratio (Elecsys immunoassay, Roche Diagnostics, Penzberg, Germany) of ⩾85 could predict women who will show adverse outcomes within 2 weeks among women with suspected PE. Interestingly, the ability of the sFlt-1/PlGF ratio to stratify the risk of PE was marked in women with suspected PE at <34 weeks of gestation, whereas it was very weak in those with suspected PE at ⩾34 weeks of gestation.85 Álvarez-Fernández et al.86 investigated whether a cutoff point of 85 of the sFlt-1/PlGF ratio was clinically useful to triage women with suspected PE. In women with suspected PE at <34 weeks of gestation, a cutoff point of 23 of the sFlt-1/PlGF ratio could exclude PE within 3 weeks with NPV of 94%, whereas a cutoff point of 85 could predict PE within 3 weeks with PPV of 93%. Recently, the results of the PROGNOSIS study were reported, which is a prospective, multicenter, observational study to derive and validate a serum level of the sFlt-1/PlGF ratio for predicting PE within 1 week and 4 weeks after the onset of suspected PE at 24–36 weeks of gestation.87 A cutoff value of 38 of the sFlt-1/PlGF ratio could exclude PE within 1 week with NPV of 99% and could predict PE within 4 weeks with PPV of 39%. These results indicated that the sFlt-1/PlGF ratio in women with suspected PE at <37 weeks of gestation might be clinically useful to triage very high-risk women with suspected PE.
Alere Triage PlGF is also promising for predicting the imminent onset of PE in women with suspected PE. Duckworth et al.88 investigated whether Alere Triage PlGF could predict the delivery owing to PE within 2 weeks in women with suspected PE. In women with suspected PE at <34 weeks of gestation, the PlGF level of the fifth percentile yielded NPV of 98%, whereas the PlGF level of the fifth percentile in women with suspected PE at 34–36 weeks of gestation yielded NPV of only 69%. Thus, Alere Triage PlGF showed favorable ability to exclude PE in women with suspected PE at <34 weeks of gestation.
In 2016, NICE published ‘PlGF-based testing to help diagnose suspected preeclampsia (Triage PlGF test, Elecsys immunoassay sFlt-1/PlGF ratio, DELFIA Xpress PlGF 1-2-3 test and BRAHMS sFlt-1 Kryptor/BRAHMS PlGF plus Kryptor PE ratio)’.89 The committee’s recommendations were as follows: the Triage PlGF test and Elecsys immunoassay sFlt-1/PlGF ratio were recommended to help exclude PE in women with suspected PE at 20–34 weeks of gestation; however, there is currently insufficient evidence to recommend their routine use for diagnosing PE, and the DELFIA Xpress PlGF 1-2-3 test and BRAHMS sFlt-1 Kryptor/BRAHMS PlGF plus Kryptor PE ratio are not recommended for routine use.
Prediction of GH
In GH, the pulsatility index of the uterine artery did not differ significantly from that of normal pregnant women, but the mean arterial pressure was higher from 12 weeks onward.90 Actually, high blood pressure in the second trimester could predict GH.91 In addition, angiogenesis-related factors in the second or early third trimesters could predict the later occurrence of GH, although all of the LR+ values were <5.72 The characteristics of GH compared with normal pregnancy in a longitudinal study from the first to third trimesters were as follows: slightly decreased PlGF levels after 26 weeks, slightly increased sFlt-1 levels after 34 weeks and almost identical sEng levels during pregnancy; high blood pressure levels during pregnancy; and enhanced maternal flow-mediated dilatation.92
Prevention of PE
No effective measure to prevent PE
Until now, effective therapies to prevent PE have not been found.82, 83, 84 Therefore, it is very important to identify clinically useful biomarkers that could help to triage pregnant women with suspected PE, such as GH or gestational proteinuria. Whenever we diagnose a pregnant woman with PE, we should monitor the mother and her fetus(es) on hospitalization, and we should induce delivery or perform cesarean section when necessary.93, 94 If we could separate low-risk women from those with suspected PE, we could reduce medical costs by reducing bed days.
Early low-dose aspirin treatment for the prevention of PE
After negative reports on the prevention of PE from 1998 to 2010,82, 83, 84 Bujold et al.95, 96 offered a ray of hope for solving the problems in the prevention of PE. Several large, multicenter, randomized and controlled trials had failed to demonstrate the clinical efficacy of low-dose aspirin (LDA) for preventing the occurrence of PE.82, 97, 98 However, the three large randomized controlled trials (RCTs) included participants at ⩾16 weeks of gestation. Bujoid et al.95, 96 found that LDA treatment starting at ⩽16 weeks of gestation was associated with a marked reduction in PE. In the most recent systematic review, an RR of PE by LDA treatment starting at ⩽16 weeks of gestation was 0.47 (CI: 0.34–0.65), whereas the same treatment starting after 16 weeks of gestation did not lead to a significant reduction in PE (RR 0.81, 95% CI 0.63–1.03).96 Recently, an RCT evaluating LDA (100 mg per day) starting at 8–10 weeks of gestation for preventing HDP was reported; a total of 164 women participated in this study, and the very early LDA treatment resulted in a marked reduction in HDP (GH and PE) with an RR of 0.07 (CI: 0.01–0.51).99 Recent animal research using a PE mouse model supported early LDA treatment for preventing PE. Doridot et al.100 created a PE mouse model by crossing transgenic male mice overexpressing human STOX1 with wild-type female mice; the wild-type female mice showed hypertension on days 2.5–18.5 with proteinuria, and hypertension and proteinuria were prevented by adding LDA to drinking water for the entirety of gestation.
Statins for future treatment to prevent PE
In 2007, Cudmore et al.101 discovered that simvastatin treatment of endothelial cells upregulated heme oxygenase-1, which can exert protective effects against oxidative stress, and simvastatin inhibited the release of sFlt-1. Soon after this discovery, two groups demonstrated early statin-based prevention of PE using two different rodent models of PE. Costantine et al.102 used a mouse model created by an adenovirus carrying sFlt-1 on day 8 of gestation, in which the mice developed hypertension and proteinuria on day 18 of gestation. Free drinking of water containing pravastatin reduced the sFlt-1 serum levels, and treatment with pravastatin decreased the contractile responses of the carotid artery to phenylephrine, which is a sympathomimetic amine that acts predominantly on α- adrenergic receptors.102 Kumasawa et al.103 established a unique experimental model using a lentiviral vector expressing a human sFlt1-mediated placenta-specific expression system; the model mice showed hypertension on day 16.5 of gestation and proteinuria on day 18.5 of gestation, and pravastatin induced PlGF and ameliorated hypertension and proteinuria. However, the protective effect was only observed when started on day 7.5 or day 10.5 of gestation, and it was not observed when the pravastatin was started at day 13.5 or day 16.5 of gestation. Currently, a clinical trial using pravastatin for the prevention of PE is ongoing.104
References
Nagaya K, Fetters MD, Ishikawa M, Kubo T, Koyanagi T, Saito Y, Sameshima H, Sugimoto M, Takagi K, Chiba Y, Honda H, Mukubo M, Kawamura M, Satoh S, Neki R . Causes of maternal mortality in Japan. JAMA 2000; 283: 2661–2667.
Yamauchi A, Minakami H, Ohkuchi A, Usui R, Idei S, Sato I . Causes of stillbirth: an analysis of 77 cases. J Obstet Gynaecol Res 1999; 25: 419–424.
American College of Obstetricians and Gynecologists; Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet Gynecol 2013; 122: 1122–1131.
Magee LA, Pels A, Helewa M, Rey E, von Dadelszen P . Canadian Hypertensive Disorders of Pregnancy (HDP) Working Group. Diagnosis, evaluation, and management of the hypertensive disorders of pregnancy. Pregnancy Hypertens 2014; 4: 105–145.
Lowe SA, Bowyer L, Lust K, McMahon LP, Morton M, North RA, Paech M, Said JM . SOMANZ guidelines for the management of hypertensive disorders of pregnancy 2014. Aust N Z J Obstet Gynaecol 2015; 55: e1–29.
Tranquilli AL, Dekker G, Magee L, Roberts J, Sibai BM, Steyn W, Zeeman GG, Brown MA . The classification, diagnosis and management of the hypertensive disorders of pregnancy: a revised statement from the ISSHP. Pregnancy Hypertens 2014; 4: 97–104.
Sato K . A proposal for a new definition and classification of ‘pregnancy induced hypertension (PIH)’ (2004). In Japan Society for the Study of Toxemia of Pregnancy. Historical Perspective of Study of Pregnancy-Induced Hypertension in Japan. Medical View Co: Tokyo, Japan. 2005, pp. 54–87.
Watanabe K, Naruse N, Tanaka K, Metoki H, Suzuki Y . Outline of definition and classification of ‘Pregnancy induced Hypertension (PIH)’. Hypertens Res Pregnancy 2013; 1: 3–4.
Brown MA, Hague WM, Higgins J, Lowe S, McCowan L, Oats J, Peek MJ, Rowan JA, Walters BN . Austalasian Society of the Study of Hypertension in Pregnancy. The detection, investigation and management of hypertension in pregnancy: full consensus statement. Aust N Z J Obstet Gynaecol 2000; 40: 139–155.
Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy. Am J Obstet Gynecol 2000; 183: S1–S22.
Brown MA, Lindheimer MD, de Swiet M, Van Assche A, Moutquin JM . The classification and diagnosis of the hypertensive disorders of pregnancy: statement from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Hypertens Pregnancy 2001; 20: IX–XIV.
Magee LA, Helewa M, Moutquin JM, von Dadelszen P . Hypertension Guideline Committee, Strategic Training Initiative in Research in the Reproductive Health Sciences (STIRRHS) Scholars. Diagnosis, evaluation, and management of the hypertensive disorders of pregnancy. J Obstet Gynaecol Can 2008; 30: S1–48.
Hypertension in pregnancy: diagnosis and management Clinical guideline. Published: 25 August 2010. Available at: https://www.nice.org.uk/Guidance/CG107. (accessed 15 May 2016).
Bartsch E, Medcalf KE, Park AL, Ray JG . High Risk of Pre-eclampsia Identification Group. Clinical risk factors for pre-eclampsia determined in early pregnancy: systematic review and meta-analysis of large cohort studies. BMJ 2016; 353: i1753.
International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10)-WHO Version for;2016. Chapter XV Pregnancy, childbirth and the puerperium (O00-O99). Oedema, proteinuria and hypertensive disorders in pregnancy, childbirth and the puerperium (O10-O16). Available at: http://apps.who.int/classifications/icd10/browse/2016/en#/O10-O16. (accessed 15 May 2016).
Yamasaki M, Nakamoto O, Suzuki Y, Takagi K, Seki H, Eguchi K, Hidaka A, Satoh K . Validation of the gestational week division border for subclassification of pregnancy induced hypertension. Hypertens Res Pregnancy 2013; 1: 23–30.
Tranquilli AL, Brown MA, Zeeman GG, Dekker G, Sibai BM . The definition of severe and early-onset preeclampsia. Statements from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Pregnancy Hypertens 2013; 3: 44–47.
von Dadelszen P, Magee LA, Roberts JM . Subclassification of preeclampsia. Hypertens Pregnancy 2003; 22: 143–148.
Levine RJ, Maynard SE, Qian C, Lim KH, England LJ, Yu KF, Schisterman EF, Thadhani R, Sachs BP, Epstein FH, Sibai BM, Sukhatme VP, Karumanchi SA . Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med 2004; 350: 672–683.
Ohkuchi A, Hirashima C, Matsubara S, Suzuki H, Takahashi K, Arai F, Watanabe T, Kario K, Suzuki M . Alterations in placental growth factor levels before and after the onset of preeclampsia are more pronounced in women with early onset severe preeclampsia. Hypertens Res 2007; 30: 151–159.
Duckitt K, Harrington D . Risk factors for pre-eclampsia at antenatal booking: systematic review of controlled studies. BMJ 2005; 330: 565.
Skjaerven R, Wilcox AJ, Lie RT . The interval between pregnancies and the risk of preeclampsia. N Engl J Med 2002; 346: 33–38.
Trupin LS, Simon LP, Eskenazi B . Change in paternity: a risk factor for preeclampsia in multiparas. Epidemiology 1996; 7: 240–244.
Nagayama S, Ohkuchi A, Usui R, Matsubara S, Suzuki M . The role of the father in the occurrence of preeclampsia. Med J Obstet Gynecol 2014; 2: 1029.
Lie RT, Rasmussen S, Brunborg H, Gjessing HK, Lie-Nielsen E, Irgens LM . Fetal and maternal contributions to risk of pre-eclampsia: population based study. BMJ 1998; 316: 1343–1347.
Li DK, Wi S . Changing paternity and the risk of preeclampsia/eclampsia in the subsequent pregnancy. Am J Epidemiol 2000; 151: 57–62.
Trogstad LI, Eskild A, Magnus P, Samuelsen SO, Nesheim BI . Changing paternity and time since last pregnancy; the impact on pre-eclampsia risk. A study of 547 238 women with and without previous preeclampsia. Int J Epidemiol 2001; 30: 1317–1322.
Mostello D, Kallogjeri D, Tungsiripat R, Leet T . Recurrence of preeclampsia: effects of gestational age at delivery of the first pregnancy, body mass index, paternity, and interval between births. Am J Obstet Gynecol 2008; 199: 55.e1–7.
Roberts JM, Redman CW . Pre-eclampsia: more than pregnancy-induced hypertension. Lancet 1993; 341: 1447–1451.
Gant NF, Daley GL, Chand S, Whalley PJ, MacDonald PC . A study of angiotensin II pressor response throughout primigravid pregnancy. J Clin Invest 1973; 52: 2682–2689.
Strevens H, Wide-Swensson D, Hansen A, Horn T, Ingemarsson I, Larsen S, Willner J, Olsen S . Glomerular endotheliosis in normal pregnancy and pre-eclampsia. BJOG 2003; 110: 831–836.
Deng L, Bremme K, Hansson LO, Blombäck M . Plasma levels of von Willebrand factor and fibronectin as markers of persisting endothelial damage in preeclampsia. Obstet Gynecol 1994; 84: 941–945.
Tsukimori K, Maeda H, Shingu M, Koyanagi T, Nobunaga M, Nakano H . The possible role of endothelial cells in hypertensive disorders during pregnancy. Obstet Gynecol 1992; 80: 229–233.
Tsukimori K, Tsushima A, Fukushima K, Nakano H, Wake N . Neutrophil-derived reactive oxygen species can modulate neutrophil adhesion to endothelial cells in preeclampsia. Am J Hypertens 2008; 21: 587–591.
Leik CE, Walsh SW . Neutrophils infiltrate resistance-sized vessels of subcutaneous fat in women with preeclampsia. Hypertension 2004; 44: 72–77.
Mishra N, Nugent WH, Mahavadi S, Walsh SW . Mechanisms of enhanced vascular reactivity in preeclampsia. Hypertension 2011; 58: 867–873.
Maynard SE, Min JY, Merchan J, Lim KH, Li J, Mondal S, Libermann TA, Morgan JP, Sellke FW, Stillman IE, Epstein FH, Sukhatme VP, Karumanchi SA . Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Invest 2003; 111: 649–658.
Venkatesha S, Toporsian M, Lam C, Hanai J, Mammoto T, Kim YM, Bdolah Y, Lim KH, Yuan HT, Libermann TA, Stillman IE, Roberts D, D'Amore PA, Epstein FH, Sellke FW, Romero R, Sukhatme VP, Letarte M, Karumanchi SA . Soluble endoglin contributes to the pathogenesis of preeclampsia. Nat Med 2006; 12: 642–649.
Levine RJ, Lam C, Qian C, Yu KF, Maynard SE, Sachs BP, Sibai BM, Epstein FH, Romero R, Thadhani R, Karumanchi SA . CPEP Study Group. Soluble endoglin and other circulating antiangiogenic factors in preeclampsia. N Engl J Med 2006; 355: 992–1005.
Hirashima C, Ohkuchi A, Takahashi K, Usui R, Matsubara S, Suzuki M . Prediction of early-onset preeclampsia using angiogenesis-related factors. Med J Obstet Gynecol 2014; 2: 1025.
Hirashima C, Ohkuchi A, Matsubara S, Suzuki H, Takahashi K, Usui R, Suzuki M . Alteration of serum soluble endoglin levels after the onset of preeclampsia is more pronounced in women with early-onset. Hypertens Res 2008; 31: 1541–1548.
Suzuki H, Ohkuchi A, Shirasuna K, Takahashi H, Usui R, Matsubara S, Suzuki M . Animal models of preeclampsia: insight into possible biomarkers candidates for predicting preeclampsia. Med J Obstet Gynecol 2014; 2: 1031.
Roberts JM, Hubel CA . Is oxidative stress the link in the two-stage model of pre-eclampsia? Lancet 1999; 354: 788–789.
Ohkuchi A, Takahashi K, Hirashima C, Usui R, Matsubara S, Suzuki M . Prediction of early-onset preeclampsia using uterine artery Doppler. Med J Obstet Gynecol 2014; 2: 1026.
Redman CW, Sargent IL . Latest advances in understanding preeclampsia. Science 2005; 308: 1592–1594.
Brosens IA, Robertson WB, Dixon HG . The role of the spiral arteries in the pathogenesis of preeclampsia. Obstet Gynecol Annu 1972; 1: 177–1791.
Gerretsen G, Huisjes HJ, Elema JD . Morphological changes of the spiral arteries in the placental bed in relation to pre-eclampsia and fetal growth retardation. Br J Obstet Gynaecol 1981; 88: 876–881.
Khong TY, De Wolf F, Robertson WB, Brosens I . Inadequate maternal vascular response to placentation in pregnancies complicated by pre-eclampsia and by small-for-gestational age infants. Br J Obstet Gynaecol 1986; 93: 1049–1059.
Meekins JW, Pijnenborg R, Hanssens M, McFadyen IR, van Asshe A . A study of placental bed spiral arteries and trophoblast invasion in normal and severe pre-eclamptic pregnancies. Br J Obstet Gynaecol 1994; 101: 669–674.
Lin S, Shimizu I, Suehara N, Nakayama M, Aono T . Uterine artery Doppler velocimetry in relation to trophoblast migration into the myometrium of the placental bed. Obstet Gynecol 1995; 85: 760–765.
Papageorghiou AT, Yu CK, Bindra R, Pandis G, Nicolaides KH . Fetal Medicine Foundation Second Trimester Screening Group. Multicenter screening for pre-eclampsia and fetal growth restriction by transvaginal uterine artery Doppler at 23 weeks of gestation. Ultrasound Obstet Gynecol 2001; 18: 441–449.
Cnossen JS, Morris RK, ter Riet G, Mol BW, van der Post JA, Coomarasamy A, Zwinderman AH, Robson SC, Bindels PJ, Kleijnen J, Khan KS . Use of uterine artery Doppler ultrasonography to predict preeclampsia and intrauterine growth restriction: a systematic review and bivariable meta-analysis. CMAJ 2008; 178: 701–711.
Odibo AO, Zhong Y, Goetzinger KR, Odibo L, Bick JL, Bower CR, Nelson DM . First-trimester placental protein 13, PAPP-A, uterine artery Doppler and maternal characteristics in the prediction of pre-eclampsia. Placenta 2011; 32: 598–602.
Foidart JM, Munaut C, Chantraine F, Akolekar R, Nicolaides KH . Maternal plasma soluble endoglin at 11-13 weeks' gestation in pre-eclampsia. Ultrasound Obstet Gynecol 2010; 35: 680–687.
Akolekar R, Minekawa R, Veduta A, Romero XC, Nicolaides KH . Maternal plasma inhibin A at 11-13 weeks of gestation in hypertensive disorders of pregnancy. Prenat Diagn 2009; 29: 753–760.
Rizzo G, Capponi A, Cavicchioni O, Vendola M, Arduini D . First trimester uterine Doppler and three-dimensional ultrasound placental volume calculation in predicting pre-eclampsia. Eur J Obstet Gynecol Reprod Biol 2008; 138: 147–151.
Martin AM, Bindra R, Curcio P, Cicero S, Nicolaides KH . Screening for pre-eclampsia and fetal growth restriction by uterine artery Doppler at 11-14 weeks of gestation. Ultrasound Obstet Gynecol 2001; 18: 583–586.
Parra M, Rodrigo R, Barja P, Bosco C, Fernández V, Muñoz H, Soto-Chacón E . Screening test for preeclampsia through assessment of uteroplacental blood flow and biochemical markers of oxidative stress and endothelial dysfunction. Am J Obstet Gynecol 2005; 193: 1486–1491.
Harrington K, Cooper D, Lees C, Hecher K, Campbell S . Doppler ultrasound of the uterine arteries: the importance of bilateral notching in the prediction of pre-eclampsia, placental abruption or delivery of a small-for-gestational-age baby. Ultrasound Obstet Gynecol 1996; 7: 182–188.
Espinoza J, Kusanovic JP, Bahado-Singh R, Gervasi MT, Romero R, Lee W, Vaisbuch E, Mazaki-Tovi S, Mittal P, Gotsch F, Erez O, Gomez R, Yeo L, Hassan SS . Should bilateral uterine artery notching be used in the risk assessment for preeclampsia, small-for-gestational-age, and gestational hypertension? J Ultrasound Med 2010; 29: 1103–1115.
Yu CK, Smith GC, Papageorghiou AT, Cacho AM, Nicolaides KH . Fetal Medicine Foundation Second Trimester Screening Group. An integrated model for the prediction of preeclampsia using maternal factors and uterine artery Doppler velocimetry in unselected low-risk women. Am J Obstet Gynecol 2005; 193: 429–436.
Albaiges G, Missfelder-Lobos H, Lees C, Parra M, Nicolaides KH . One-stage screening for pregnancy complications by color Doppler assessment of the uterine arteries at 23 weeks' gestation. Obstet Gynecol 2000; 96: 559–564.
Diab AE, El-Behery MM, Ebrahiem MA, Shehata AE . Angiogenic factors for the prediction of pre-eclampsia in women with abnormal midtrimester uterine artery Doppler velocimetry. Int J Gynaecol Obstet 2008; 102: 146–151.
Stepan H, Geipel A, Schwarz F, Krämer T, Wessel N, Faber R . Circulatory soluble endoglin and its predictive value for preeclampsia in second-trimester pregnancies with abnormal uterine perfusion. Am J Obstet Gynecol 2008; 198: 175.e1–6.
Conde-Agudelo A, Villar J, Lindheimer M . World Health Organization systematic review of screening tests for preeclampsia. Obstet Gynecol 2004; 104: 1367–1391.
Cnossen JS, ter Riet G, Mol BW, van der Post JA, Leeflang MM, Meads CA, Hyde C, Khan KS . Are tests for predicting pre-eclampsia good enough to make screening viable? A review of reviews and critical appraisal. Acta Obstet Gynecol Scand 2009; 88: 758–765.
Forest JC, Charland M, Massé J, Bujold E, Rousseau F, Lafond J, Giguère Y . Candidate biochemical markers for screening of pre-eclampsia in early pregnancy. Clin Chem Lab Med 2012; 50: 973–984.
Akolekar R, Syngelaki A, Sarquis R, Zvanca M, Nicolaides KH . Prediction of early, intermediate and late pre-eclampsia from maternal factors, biophysical and biochemical markers at 11-13 weeks. Prenat Diagn 2011; 31: 66–74.
Kleinrouweler CE, Wiegerinck MM, Ris-Stalpers C, Bossuyt PM, van der Post JA, von Dadelszen P, Mol BW, Pajkrt E . EBM CONNECT Collaboration. Accuracy of circulating placental growth factor, vascular endothelial growth factor, soluble fms-like tyrosine kinase 1 and soluble endoglin in the prediction of pre-eclampsia: a systematic review and meta-analysis. BJOG 2012; 119: 778–787.
Akolekar R, Syngelaki A, Poon L, Wright D, Nicolaides KH . Competing risks model in early screening for preeclampsia by biophysical and biochemical markers. Fetal Diagn Ther 2013; 33: 8–15.
Ohkuchi A, Hirashima C, Takahashi K, Suzuki H, Matsubara S, Suzuki M . Onset threshold of the plasma levels of soluble fms-like tyrosine kinase 1/placental growth factor ratio for predicting the imminent onset of preeclampsia within 4 weeks after blood sampling at 19-31 weeks of gestation. Hypertens Res 2013; 36: 1073–1080.
Ohkuchi A, Hirashima C, Matsubara S, Takahashi K, Matsuda Y, Suzuki M . Threshold of soluble fms-like tyrosine kinase 1/placental growth factor ratio for the imminent onset of preeclampsia. Hypertension 2011; 58: 859–866.
Crispi F, Llurba E, Domínguez C, Martín-Gallán P, Cabero L, Gratacós E . Predictive value of angiogenic factors and uterine artery Doppler for early- versus late-onset pre-eclampsia and intrauterine growth restriction. Ultrasound Obstet Gynecol 2008; 31: 303–309.
Kusanovic JP, Romero R, Chaiworapongsa T, Erez O, Mittal P, Vaisbuch E, Mazaki-Tovi S, Gotsch F, Edwin SS, Gomez R, Yeo L, Conde-Agudelo A, Hassan SS . A prospective cohort study of the value of maternal plasma concentrations of angiogenic and anti-angiogenic factors in early pregnancy and midtrimester in the identification of patients destined to develop preeclampsia. J Matern Fetal Neonatal Med 2009; 22: 1021–1038.
Moore Simas TA, Crawford SL, Bathgate S, Yan J, Robidoux L, Moore M, Maynard SE . Angiogenic biomarkers for prediction of early preeclampsia onset in high-risk women. J Matern Fetal Neonatal Med 2014; 27: 1038–1048.
Kuc S, Koster MP, Franx A, Schielen PC, Visser GH . Maternal characteristics, mean arterial pressure and serum markers in early prediction of preeclampsia. PLoS One 2013; 8: e63546.
Di Lorenzo G, Ceccarello M, Cecotti V, Ronfani L, Monasta L, Vecchi Brumatti L, Montico M, D'Ottavio G . First trimester maternal serum PIGF, free β-hCG, PAPP-A, PP-13, uterine artery Doppler and maternal history for the prediction of preeclampsia. Placenta 2012; 33: 495–501.
Poon LC, Stratieva V, Piras S, Piri S, Nicolaides KH . Hypertensive disorders in pregnancy: combined screening by uterine artery Doppler, blood pressure and serum PAPP-A at 11-13 weeks. Prenat Diagn 2010; 30: 216–223.
Poon LC, Kametas NA, Maiz N, Akolekar R, Nicolaides KH . First-trimester prediction of hypertensive disorders in pregnancy. Hypertension 2009; 53: 812–818.
Akolekar R, Zaragoza E, Poon LC, Pepes S, Nicolaides KH . Maternal serum placental growth factor at 11+0 to 13+6 weeks of gestation in the prediction of pre-eclampsia. Ultrasound Obstet Gynecol 2008; 32: 732–739.
Hirashima C, Ohkuchi A, Takahashi K, Suzuki H, Matsubara S, Suzuki M . A novel three-step approach for predicting the imminent onset of preeclampsia within 4 weeks after blood sampling at 19-31 weeks of gestation. Hypertens Res 2014; 37: 519–525.
Caritis S, Sibai B, Hauth J, Lindheimer MD, Klebanoff M, Thom E, VanDorsten P, Landon M, Paul R, Miodovnik M, Meis P, Thurnau G . Low-dose aspirin to prevent preeclampsia in women at high risk. National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med 1998; 338: 701–705.
Levine RJ, Hauth JC, Curet LB, Sibai BM, Catalano PM, Morris CD, DerSimonian R, Esterlitz JR, Raymond EG, Bild DE, Clemens JD, Cutler JA . Trial of calcium to prevent preeclampsia. N Engl J Med 1997; 337: 69–76.
Roberts JM, Myatt L, Spong CY, Thom EA, Hauth JC, Leveno KJ, Pearson GD, Wapner RJ, Varner MW, Thorp JM Jr, Mercer BM, Peaceman AM, Ramin SM, Carpenter MW, Samuels P, Sciscione A, Harper M, Smith WJ, Saade G, Sorokin Y, Anderson GB . Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Vitamins C and E to prevent complications of pregnancy-associated hypertension. N Engl J Med 2010; 362: 1282–1291.
Rana S, Powe CE, Salahuddin S, Verlohren S, Perschel FH, Levine RJ, Lim KH, Wenger JB, Thadhani R, Karumanchi SA . Angiogenic factors and the risk of adverse outcomes in women with suspected preeclampsia. Circulation 2012; 125: 911–919.
Álvarez-Fernández I, Prieto B, Rodríguez V, Ruano Y, Escudero AI, Álvarez FV . New biomarkers in diagnosis of early onset preeclampsia and imminent delivery prognosis. Clin Chem Lab Med 2014; 52: 1159–1168.
Zeisler H, Llurba E, Chantraine F, Vatish M, Staff AC, Sennström M, Olovsson M, Brennecke SP, Stepan H, Allegranza D, Dilba P, Schoedl M, Hund M, Verlohren S . Predictive value of the sFlt-1: PlGF ratio in women with suspected preeclampsia. N Engl J Med 2016; 374: 13–22.
Hunter R, Duckworth S, Seed P, Shennan A, Chappell L . PP051. Budget impact analysis of maternal plasma PIGF concentrations in women with suspected pre-eclampsia: the potential for improved health service usage. Pregnancy Hypertens 2013; 3: 85.
PlGF-based testing to help diagnose suspected pre-eclampsia (Triage PlGF test, Elecsys immunoassay sFlt-1/PlGF ratio, DELFIA Xpress PlGF 1-2-3 test, and BRAHMS sFlt-1 Kryptor/BRAHMS PlGF plus Kryptor PE ratio). NICE diagnostics guidance [DG23]. Available at: https://www.nice.org.uk/guidance/dg23. (accessed 24 May 2016).
Khalil A, Garcia-Mandujano R, Maiz N, Elkhouli M, Nicolaides KH . Longitudinal changes in uterine artery Doppler and blood pressure and risk of pre-eclampsia. Ultrasound Obstet Gynecol 2014; 43: 541–547.
Ohkuchi A, Iwasaki R, Suzuki H, Hirashima C, Takahashi K, Usui R, Matsubara S, Minakami H, Suzuki M . Normal and high-normal blood pressures, but not body mass index, are risk factors for the subsequent occurrence of both preeclampsia and gestational hypertension: a retrospective cohort study. Hypertens Res 2006; 29: 161–167.
Noori M, Donald AE, Angelakopoulou A, Hingorani AD, Williams DJ . Prospective study of placental angiogenic factors and maternal vascular function before and after preeclampsia and gestational hypertension. Circulation 2010; 122: 478–487.
Minakami H, Hiramatsu Y, Koresawa M, Fujii T, Hamada H, Iitsuka Y, Ikeda T, Ishikawa H, Ishimoto H, Itoh H, Kanayama N, Kasuga Y, Kawabata M, Konishi I, Matsubara S, Matsuda H, Murakoshi T, Ohkuchi A, Okai T, Saito S, Sakai M, Satoh S, Sekizawa A, Suzuki M, Takahashi T, Tokunaga A, Tsukahara Y, Yoshikawa H . Japan Society of Obstetrics and Gynecology; Japan Association of Obstetricians and Gynecologists. Guidelines for obstetrical practice in Japan: Japan Society of Obstetrics and Gynecology (JSOG) and Japan Association of Obstetricians and Gynecologists (JAOG) 2011 edition. J Obstet Gynaecol Res 2011; 37: 1174–1197.
Minakami H, Maeda T, Fujii T, Hamada H, Iitsuka Y, Itakura A, Itoh H, Iwashita M, Kanagawa T, Kanai M, Kasuga Y, Kawabata M, Kobayashi K, Kotani T, Kudo Y, Makino Y, Matsubara S, Matsuda H, Miura K, Murakoshi T, Murotsuki J, Ohkuchi A, Ohno Y, Ohshiba Y, Satoh S, Sekizawa A, Sugiura M, Suzuki S, Takahashi T, Tsukahara Y, Unno N, Yoshikawa H . Guidelines for obstetrical practice in Japan: Japan Society of Obstetrics and Gynecology (JSOG) and Japan Association of Obstetricians and Gynecologists (JAOG) 2014 edition. J Obstet Gynaecol Res 2014; 40: 1469–1499.
Bujold E, Morency AM, Roberge S, Lacasse Y, Forest JC, Giguère Y . Acetylsalicylic acid for the prevention of preeclampsia and intra-uterine growth restriction in women with abnormal uterine artery Doppler: a systematic review and meta-analysis. J Obstet Gynaecol Can 2009; 31: 818–826.
Bujold E, Roberge S, Lacasse Y, Bureau M, Audibert F, Marcoux S, Forest JC, Giguère Y . Prevention of preeclampsia and intrauterine growth restriction with aspirin started in early pregnancy: a meta-analysis. Obstet Gynecol 2010; 116: 402–414.
CLASP: a randomised trial of low-dose aspirin for the prevention and treatment of pre-eclampsia among 9364 pregnant women. CLASP (Collaborative Low-dose Aspirin Study in Pregnancy) Collaborative Group. Lancet 1994; 343: 619–629.
Golding J . A randomised trial of low dose aspirin for primiparae in pregnancy. The Jamaica Low Dose Aspirin Study Group. Br J Obstet Gynaecol 1998; 105: 293–299.
Bakhti A, Vaiman D . Prevention of gravidic endothelial hypertension by aspirin treatment administered from the 8th week of gestation. Hypertens Res 2011; 34: 1116–1120.
Doridot L, Passet B, Méhats C, Rigourd V, Barbaux S, Ducat A, Mondon F, Vilotte M, Castille J, Breuiller-Fouché M, Daniel N, le Provost F, Bauchet AL, Baudrie V, Hertig A, Buffat C, Simeoni U, Germain G, Vilotte JL, Vaiman D . Preeclampsia-like symptoms induced in mice by fetoplacental expression of STOX1 are reversed by aspirin treatment. Hypertension 2013; 61: 662–668.
Cudmore M, Ahmad S, Al-Ani B, Fujisawa T, Coxall H, Chudasama K, Devey LR, Wigmore SJ, Abbas A, Hewett PW, Ahmed A . Negative regulation of soluble Flt-1 and soluble endoglin release by heme oxygenase-1. Circulation 2007; 115: 1789–1797.
Costantine MM, Tamayo E, Lu F, Bytautiene E, Longo M, Hankins GD, Saade GR . Using pravastatin to improve the vascular reactivity in a mouse model of soluble fms-like tyrosine kinase-1-induced preeclampsia. Obstet Gynecol 2010; 116: 114–120.
Kumasawa K, Ikawa M, Kidoya H, Hasuwa H, Saito-Fujita T, Morioka Y, Takakura N, Kimura T, Okabe M . Pravastatin induces placental growth factor (PGF) and ameliorates preeclampsia in a mouse model. Proc Natl Acad Sci USA 2011; 108: 1451–1455.
Pravastatin for Prevention of Preeclampsia ClinicalTrials.gov Identifier: NCT0171758. Available at: https://clinicaltrials.gov/ct2/show/NCT01717586. Accessed 24 May 2016.
Acknowledgements
This work was supported by Grants-in-Aid (18591809, 24390383 and 24592482 to AO) from the Ministry of Education, Culture, Sports, Science and Technology, Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Rights and permissions
About this article
Cite this article
Ohkuchi, A., Hirashima, C., Takahashi, K. et al. Prediction and prevention of hypertensive disorders of pregnancy. Hypertens Res 40, 5–14 (2017). https://doi.org/10.1038/hr.2016.107
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.107
Keywords
This article is cited by
-
Mid-Trimester Spot Urinary Albumin/Creatinine Ratio as a Screening Tool in Prediction of Pre-eclampsia
The Journal of Obstetrics and Gynecology of India (2023)
-
A nationwide, prospective, cohort study on exogenous oxytocin and delays in early child development: the Japan environment and children’s study
European Journal of Pediatrics (2023)
-
Influence of Swimming Program on the Blood Pressure of Pregnant Hypertensive Rats and Their Fetuses
Reproductive Sciences (2021)
-
Novel biomarker profiles in experimental aged maternal mice with hypertensive disorders of pregnancy
Hypertension Research (2019)
-
Increased plasma fatty acid binding protein 4 concentration at the first prenatal visit and its relevance to preeclampsia
Hypertension Research (2018)