Abstract
There is increasing evidence of an association between residential environments and hypertension. As shown in our previous study, the inconvenience of the locations of residential areas may be one of the factors influencing the blood pressures of inhabitants. Salt intake is one of the likely mediators between inconvenience and hypertension. Therefore, in this study, we evaluated the association between the altitudes of residential areas and salt intake in a rural Japanese region because altitude may be one of the proxies for inconvenience. In this cross-sectional study, 1016 participants living in a mountainous region in Japan were recruited during health examinations. The altitude of each participant’s residence was estimated using a geographic information system. Subjects were divided into quartile groups according to the altitudes of their residences. To evaluate salt intake, we employed the 24-h salt intake estimation of Kawano et al. (e24-h salt intake) and the urinary sodium-to-potassium ratio (uNa/K). Linear regression analyses indicated that altitude was an independent factor influencing both e24-h salt intake and uNa/K after adjustments for age, sex, body mass index, physical activity, alcohol consumption, triglycerides and county of residence. The same result was observed when the subjects who did not take antihypertensive medications were analyzed (N=633). The present study indicated that altitude of residence had a significant positive influence on salt intake in a rural area of Japan.
Similar content being viewed by others
Introduction
There is a growing interest in the association between residential environments and hypertension.1, 2, 3, 4, 5 Residential environments have both physical (for example, climate and geography) and social (for example, socioeconomic conditions and social capital) aspects that may contribute to individual health.6 Inconvenience in daily life may be one such factor. Japan has wide mountainous regions (hilly and mountainous areas make up ~70% of the land) in which people have greatly reduced access to facilities that support their health and daily lives (grocery stores, hospitals and so on).7, 8, 9
In a previous study, we showed that distance from an urban area influenced the average blood pressure (BP) of inhabitants.10 Considering the mechanisms underlying this observation, we hypothesized that inconvenience caused by geographic features may influence salt intake, which may result in increased BPs.11 Evidence from previous studies has revealed the cardiovascular complications and negative effects on BPs caused by high salt intake.12, 13, 14 Furthermore, a recent study in the UK reported that salt intake differed among subjects according to their socioeconomic statuses and the geographical features of the places where they lived.15
Therefore, in this study, we examined the association between altitudes of residence, which is a possible index of inconvenience in Japan, and salt intake in a rural area.
Materials and methods
Participants
This cross-sectional population-based study was conducted as part of the Shimane CoHRE Study, a cohort study designed to determine risk factors of lifestyle-related diseases, including hypertension. Health examinations were performed in six counties (Kakeya, Mitoya, Daito, Kamo, Yoshida and Kisuki) located in Un-nan City in 2012. Un-nan City is located in a rural mountainous area in the eastern part of Shimane Prefecture, Japan. People receiving health examinations were invited to participate in the study and were included when they gave written informed consent. After excluding individuals with missing data, we recruited 1016 individuals who were included in the study. The study was approved by the ethics committee at Shimane University.
Measurements
BP was measured in subjects twice with automatic sphygmomanometers after a 15-min rest period in the sitting position, and the lower value was taken as the representative BP. An interview included questions regarding individuals’ history of hypertension, and their use of antihypertensive drugs was verified by checking the subject’s prescription records. Regular physical activity, alcohol consumption and smoking habits were investigated in the interview as well. Subjects who participated in 1 h or more of physical activity (for example, walking) per day were categorized as having high physical activity. Drinkers were defined as those who consumed alcohol once a week or more.
High-density and low-density lipoprotein cholesterol, triglycerides and fasting blood glucose were measured in serum by standard methods.
Altitudes of residences were estimated with a geographic information system based on the addresses of the participants (ESRI Japan, Tokyo, Japan). In the analysis, subjects were divided into quartile groups according to their altitudes of residence: 29–44 m, N=261; 45–68 m, N=237; 69–195 m, N=245 and 196–485 m, N=250.
We used two different parameters to evaluate salt intake: (1) estimated 24-h salt intake (e24-h salt intake), which was calculated with the formula proposed by Kawano et al.,16 and (2) the urinary sodium-to-potassium ratio (uNa/K). The uNa/K has been reported to be an index of salt intake.17, 18, 19 A significant correlation was observed between the e24-h salt intake and the log-transformed uNa/K in the present study (Pearson’s r=0.72; P<0.0001, see Supplementary Figure 1). Although the ability of these methods to accurately estimate salt intakes in individuals is limited, they are still useful and practical for estimating salt intake in a large population.16, 17, 18, 19, 20 Spot urine samples were collected at the site of the health examination, and the concentrations of sodium and potassium were measured using the electrode method (TBA-c16000, Toshiba Medical System Corporation, Tochigi, Japan).
Statistical analysis
All of the measures were represented as the mean±the s.d. Parameters influencing salt intake were analyzed by the linear regression analysis. We used a linear regression analysis instead of a multilevel analysis because (1) the number of counties analyzed here was rather small and (2) the subjects in this study were not to be stratified, because they voluntarily participated in the study. In addition, the counties studied covered a wide area, allowing for substantial randomization. Furthermore, regression coefficients provided by the linear regression analysis were a useful parameter for interpreting the results. P<0.05 was considered statistically significant. All of the statistical analyses were performed using JMP 11 (SAS Institute, Cary, NC, USA) and SPSS (v.23, IBM, Armonk, NY, USA).
Results
Characteristics of the studied population are displayed in Table 1. We found significant differences in the e24-h salt intakes as well as in the uNa/K results between the quartiles according to the altitudes of residence. A post-hoc analysis indicated that the e24-h salt intakes and the uNa/K measures were significantly different between quartile (Q) 1 and the other quartiles (Dunnett’s test using Q1 as the reference).
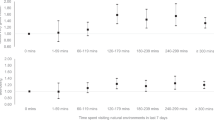
Factors influencing the salt intake are presented in Table 2. In Spearman’s non-parametric correlation analysis, sex, age, body mass index, systolic and diastolic BPs (SBP and DBP, respectively), high-density lipoprotein cholesterol, TG and alcohol consumption were found to have significant correlations with salt intake in addition to the altitude of residence. In addition to the factors included in this univariate analysis, we accounted for effects of the county of residence; as presented in Figure 1, the county of residence appeared to have an effect on the e24-h salt intake independent of the altitude.
Therefore, we performed a linear regression analysis on the e24-h salt intake and included the county of residence as a nominal variance. Because BP was probably the result of salt intake, we excluded SBP and DBP from the model. The results are summarized in Table 3. Even if the county of residence was included in the model, the altitude displayed an independent effect on the salt intake in addition to sex, age, body mass index and physical activity. Collinearity among the parameters was not high when variance inflation factors were calculated (the maximal variance inflation factor for the altitude was 1.96). When the analysis was performed on the uNa/K measurements, the altitude was a significant independent factor influencing it in parallel with sex and the county of residence (see Table 4). The addition of SBP (or DBP) in the model did not affect the results; the altitude was still an independent factor affecting the salt intake (data not shown). Adjusted e24-h salt intakes and uNa/K measurements according to the county of residence and altitude are summarized in Supplementary Table 1.
Out of all of the participants, 383 were receiving treatment with antihypertensive drugs. Therefore, we performed the same analysis on those who were not taking antihypertensive drugs (N=633) to avoid potential perturbation by antihypertensive treatment. The results indicated that the effect of altitude was significant in this population as well (Supplementary Table 2).
Discussion
To the best of our knowledge, this is the first study to examine the association between altitude of residence and salt intake. The major finding of our study was that salt intake was associated with higher altitudes in a rural area of Japan. This association seemed robust even after adjusting for the county of residence (see Table 3). Furthermore, the same significant association was observed after excluding the subjects taking antihypertensive drugs (Supplementary Table 1) and between the altitude and uNa/K measurements, which are another estimate of daily salt intake (see Table 4).
Previous studies noted that climbing at high altitudes acutely increased BP.21, 22 Several factors in addition to lower air pressure have been suggested to be responsible for this, such as hypoxia, low temperatures, wind, stress and dehydration.23, 24 In contrast, chronic effects of living at high altitudes have been controversial.25 However, the subjects in this study lived at altitudes between 29 and 485 m in height. These are much lower than those in previous studies, which usually included altitudes above 2000 m. Accordingly, the effects of altitude observed in this study were probably not consequences of physical effects of the altitudes.
In this context, it is of interest that Tyrovolas et al. reported that people living in mountainous regions (above 400 m in height) on Mediterranean islands had a greater incidence of metabolic syndromes, including hypertension.26 They argued that people living in mountainous regions had fewer opportunities to use health-promoting facilities due to inconvenience or remoteness. To examine whether similar inconveniences were indeed present in our population, we assessed the number of food shops and bus stops in the studied counties according to their altitudes using the geographic information system. As expected, the results indicated that number of these facilities decreased with increasing altitudes, suggesting that living at high altitudes is more inconvenient (Supplementary Figure 2). Based on the above analysis, it is possible to hypothesize that people living at higher altitudes in this area might consume more processed food, which contains more salt because of the reduced access to fresh food. This hypothesis needs to be examined in future studies, and, if it is confirmed, strategies for reducing consumption of processed foods would be required.27
In addition to the altitude, it is of interest that physical activity showed a positive effect on salt intake. Currently, we only have a speculative explanation for this: increased food consumption might be associated with increased physical activity, which might result in increased salt intake. To prove this hypothesis, it will be necessary to examine the food intake in this population. This has not been done yet.
In contrast to salt intake, altitudes did not influence BP. When factors influencing SBP were evaluated by a linear regression analysis, the e24-h salt intake was a strong independent risk factor for increased SBP (B±s.e.=1.1±0.2, P<0.0001), along with age and body mass index (data not shown). This indicated that although the altitude did indeed affect salt intake in this population, many other factors, especially those related to the individual’s lifestyle, probably had a larger influence on the salt intake and BP of each subject. In the previous study, we showed that distance from an urban area was an independent risk factor for hypertension.10 In that report, we argued that distance from an urban area was a parameter representing inconvenience as well. At the moment, we cannot provide a hypothesis for the reason that altitude and distance from an urban area gave different results for hypertension. Further analyses may be needed to this inconsistency between the two parameters.
It is of interest that the county of residence had an independent effect on the salt intake in addition to the altitude. Several parameters were significantly different among the counties (see Supplementary Table 3). Nevertheless, the effect of the county of residence remained significant after these parameters were adjusted in a linear regression analysis (see Table 3). Potential confounding factors, such as differences in urbanization, might contribute to this observation. Further analyses are warranted on this issue as well.
Our study has several limitations. First, owing to its cross-sectional design, it was, in general, difficult to argue the causal relationship between the independent and dependent parameters. However, in the present case, it seems reasonable to assume that the altitude of residence causally influences salt intake, because the opposite is not likely. Second, our data did not allow for the assessment of other important socioeconomic factors related to hypertension, such as income, education and occupation, which could be confounding factors that explain the effect of the county of residence on salt intake described above. In spite of these limitations, this is a unique study evaluating the altitude of residence as a factor influencing people’s dietary habits. The implementation of geographical factors as a risk factor may be warranted in future studies of lifestyle-related diseases.
References
Hamano T, Fujisawa Y, Yamasaki M, Ito K, Nabika T, Shiwaku K . Contributions of social context to blood pressure: findings from a multilevel analysis of social capital and systolic blood pressure. Am J Hypertens 2011; 24: 643–646.
Chaix B, Bean K, Leal C, Thomas F, Havard S, Evans D, Jego B, Pannier B . Individual/neighborhood social factors and blood pressure in the RECORD Cohort Study: which risk factors explain the associations? Hypertension 2010; 55: 769–775.
Chaix B, Ducimetiere P, Lang T, Haas B, Montaye M, Ruidavets JB, Arveiler D, Amouyel P, Ferrieres J, Bingham A, Chauvin P . Residential environment and blood pressure in the PRIME Study: is the association mediated by body mass index and waist circumference? J Hypertens 2008; 26: 1078–1084.
McGrath JJ, Matthews KA, Brady SS . Individual versus neighborhood socioeconomic status and race as predictors of adolescent ambulatory blood pressure and heart rate. Soc Sci Med 2006; 63: 1442–1453.
Estes MG Jr, Al-Hamdan MZ, Crosson W, Estes SM, Quattrochi D, Kent S, McClure LA . Use of remotely sensed data to evaluate the relationship between living environment and blood pressure. Environ Health Perspect 2009; 117: 1832–1838.
Diez Roux AV, Mair C . Neighborhoods and health. Ann N Y Acad Sci 2010; 1186: 125–145.
Hamano T, Kimura Y, Takeda M, Yamasaki M, Nabika T, Shiwaku K . Is location associated with high risk of hypertension? Shimane COHRE Study. Am J Hypertens 2012; 25: 784–788.
Kawakami N, Li X, Sundquist K . Health-promoting and health-damaging neighbourhood resources and coronary heart disease: a follow-up study of 2165000 people. J Epidemiol Community Health 2011; 65: 866–872.
Baibas N, Trichopoulou A, Voridis E, Trichopoulos D . Residence in mountainous compared with lowland areas in relation to total and coronary mortality. A study in rural Greece. J Epidemiol Community Health 2005; 59: 274–278.
Hamano T, Kimura Y, Takeda M, Yamasaki M, Isomura M, Nabika T, Shiwaku K . Effect of environmental and lifestyle factors on hypertension: Shimane COHRE Study. PLoS One 2012; 7: e49122.
Satoh E . Accessibility in the community healthcare system. J Natl Inst Public Health 2010; 59: 43–50.
He FJ, MacGregor GA . How far should salt intake be reduced? Hypertension 2003; 42: 1093–1099.
Ando K, Kawarazaki H, Miura K, Matsuura H, Watanabe Y, Yoshita K, Kawamura M, Kusaka M, Kai H, Tsuchihashi T, Kawano Y . Report of the Salt Reduction Committee of the Japanese Society of Hypertension (1): Role of salt in hypertension and cardiovascular diseases. Hypertens Res 2013; 36: 1009–1019.
Ohta Y, Tsuchihashi T, Kiyohara K, Oniki H . High salt intake promotes a decline in renal function in hypertensive patients: a 10-year observantional study. Hypertens Res 2013; 36: 172–176.
Ji C, Kandala NB, Cappuccio FP . Spatial variation of salt intake in Britain and association with socioeconomic status. Br Med J 2013; 3: e002246.
Kawano Y, Tsuchihashi T, Matsuura H, Ando K, Fujita T, Ueshima H . Report of the Working Group for Dietary Salt Reduction of the Japanese Society of Hypertension: (2) Assessment of Salt Intake in the Management of Hypertension. Hypertens Res 2007; 30: 887–893.
Huggins CE, O’Reilly S, Brinkman M, Hodge A, Giles GG, English DR, Nowson CA . Relationship of urinary sodium and sodium-to-potassium ratio to blood pressure in older adults in Australia. Med J 2011; 195: 128–132.
Jan RA, Shah S, Saleem SM, Waheed A, Mufti S, Lone MA, Ashraf M . Sodium and potassium excretion in normotensive and hypertensive population in Kashmir. J Assoc Physicians India 2006; 54: 22–26.
Zhao X, Yin X, Li X, Yan LL, Lam CT, Li S, He F, Xie W, Ba S, Luobu G, Ke L, Wu Y . Using a low-sodium, high-potassium salt substitute to reduce blood pressure among tibetans with high blood pressure: A Patient-Blinded Randomized Controlled Trial. PLoS One 2014; 9: e110131.
Sasaki M, Tsuchihashi T, Arakawa K, Fukui H, Kameda W, Tominaga M . Long-term variability of urinary salt excretion and blood pressure in hypertensive patients. Hypertens Res 2014; 37: 939–943.
Khalid ME, Ali ME, Ahmed EK, Elkarib AO . Pattern of blood pressures among high and low altitude residents of southern Saudi Arabia. J Hum Hypertens 1994; 8: 765–769.
Fiori G, Facchini F, Pettener D, Rimondi A, Battistini N, Bedogni G . Relationships between blood pressure, anthropometric characteristics and blood lipids in high- and low-altitude populations from Central Asia. Ann Hum Biol 2000; 27: 19–28.
Handler J . Altitude-Related Hypertension. J Clin Hypertens 2009; 11: 161–165.
Brook RD, Weder AB, Rajagopalan S . ‘‘Environmental hypertensionology’’ the effects of environmental factors on blood pressure in clinical practice and research. J Clin Hypertens 2011; 13: 836–842.
Khouzam RM, Aziz RK . A case report: can altitude change blood pressure that much? J Clin Hypertens 2009; 11: 498–499.
Tyrovolas S, Chalkias C, MorenaM, Tsiligianni I, Zeimbekis A, Gotsis E, Metallinos G, Bountziouka V, Polychronopoulos E, Lionis C, Panagiotakos D . Health care access and prevalence of the metabolic syndrome among elders living in high-altitude areas of the mediterranean islands: the MEDIS Study. Rev Diabet Stud 2011; 8: 468–476.
Okuda N, Nishi N, Ishikawa-Takata K, Yoshimura E, Horie S, Nakanishi T, Sato Y, Takimoto H . Understanding of sodium content labeled on food packages by Japanese people. Hypertens Res 2014; 37: 467–471.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Ferdaus, S., Kohno, K., Hamano, T. et al. Altitudes of residential areas affect salt intake in a rural area in Japan: a Shimane CoHRE Study. Hypertens Res 38, 895–898 (2015). https://doi.org/10.1038/hr.2015.91
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2015.91
Keywords
This article is cited by
-
Twenty-four-hour urinary sodium and potassium excretion and associated factors in Japanese secondary school students
Hypertension Research (2016)
-
A modified DASH diet is one possible solution for overcoming the unfavorable link between vegetable and salt intake in the Japanese diet
Hypertension Research (2016)