Abstract
Pulse wave velocity (PWV) and pulse pressure (PP) are blood pressure (BP)-dependent surrogates for vascular stiffness. Considering that there are no clinically useful markers for arterial stiffness that are BP-independent, our objective was to identify novel indices of arterial stiffness and compare them with previously described markers. PWV and PP were measured in young and old male Fisher rats and in young and old male spontaneously hypertensive rats (SHR) over a wide range of BPs. The BP dependence of these and several other indices of vascular stiffness were evaluated. An index incorporating PWV and PP was also constructed. Both PWV and PP increase in a non-linear manner with rising BP for both strains of animals (Fisher and SHRs). Age markedly changes the relationship between PWV or PP and BP. The previously described Ambulatory Arterial Stiffness Index (AASI) was able to differentiate between young and old vasculature, whereas the Cardio-Ankle Vascular Index (CAVI) did not reliably differentiate between the two. The novel Arterial Stiffness Index (ASI) differentiated stiffer from more compliant vasculature. Considering the limitations of the currently available indices of arterial stiffness, we propose a novel index of intrinsic arterial stiffness, the ASI, which is robust over a range of BPs and allows one to distinguish between compliant and stiff vasculature in both Fisher rats and SHRs. Further studies are necessary to validate this index in other settings.
Similar content being viewed by others
Introduction
Age-associated systolic hypertension, a disproportional increase in systolic blood pressure (BP) while maintaining a relatively normal or even decreased diastolic BP, has consistently been linked with increased cardiovascular morbidity and mortality.1 There is a growing body of evidence that vascular stiffness occurs before isolated systolic hypertension develops.2 Vascular stiffness, which is the reciprocal of compliance, depends mainly on contributions of the stretchable elastin and the stiffer collagen in the extracellular matrix. With aging, elastin is broken down and replaced by collagen, making older arteries less compliant.3, 4 Moreover, vascular compliance depends on wall tension, which is determined by the distending pressure and the geometry (radius) of the vessel. Decreased arterial compliance with aging has direct implications for ventricular-arterial coupling, leading to an increase in myocardial workload, increased oxygen consumption, cardiac hypertrophy and ischemia.5 Moreover, decreased compliance impairs endothelial barrier function, an essential step in the development of atherosclerosis.6 Unfortunately, direct measures of arterial compliance often require complex devices and are not routinely performed in the clinical setting (for example, Young’s elastic modulus, stiffness index (β), magnetic resonance imaging or ultrasound-derived arterial distensibility7, 8). On the basis of the stiffness index, which approximates changes in arterial pressure and diameter ex vivo with a logarithmic transformation, the Cardio-Ankle Vascular Index (CAVI) was established encompassing both smooth muscle tone and matrix components.9 Another marker utilized to assess intrinsic arterial stiffness, the Ambulatory Arterial Stiffness Index (AASI), obtained from systolic and diastolic BP measurements over 24h, was shown to discriminate stiff from compliant vasculature.10, 11, 12 The AASI is defined as one minus the slope of a linear regression of diastolic BP as a function of systolic BP10 and its precision depends on the number of BP measurements.
In contrast, surrogate markers of arterial stiffness such as pulse wave velocity (PWV, the speed at which a pulse wave travels along the arterial tree) or pulse pressure (PP, the difference between systolic and diastolic BP) can be measured non-invasively with relatively simple devices.13 Multiple studies have demonstrated a relationship between increases in PWV or PP and adverse cardiovascular outcomes.10, 14, 15, 16, 17, 18 The major drawback of PWV is that it depends not only on intrinsic arterial wall stiffness, but also on wall tension (and hence on wall thickness, radius, vascular smooth muscle tone and distending BP).19 Thus, for the same patient, different values for PWV or PP will be obtained with changes in BP, even though the intrinsic constituent material of the arterial wall remains unchanged. To utilize PWV or PP as an index of either 'intrinsic arterial stiffness' or 'arterial aging', it needs to be normalized to BP.20
Given that PWV and BP are relatively easy to obtain, we evaluated the indices of vascular stiffness derived from these parameters using a common set of data obtained in older and younger normotensive and hypertensive rats. We then used these data to derive the Arterial Stiffness Index (ASI). Considering that both PP and PWV are BP-dependent measures, we minimized this confounding effect by evaluating the direct relationship between the PP and PWV. The ASI was then defined as the slope of the midline between the data of a parametric plot of PWV vs. PP as diastolic BP is increased. In this manuscript, we describe several parameters of arterial stiffness including PP, PWV, AASI, CAVI and ASI, their relation to BP and their ability to distinguish compliant from stiff arteries.
Materials and methods
For the normotensive group of animals, the invasive BP, PWV and PP data were obtained from a subset of animals that were part of another study in which we demonstrated the aging-associated increases in vascular stiffness as evidenced by changes in nitric oxide signaling, crosslinking of matrix enzymes, collagen and elastin deposition, and tensile properties.21 For the hypertensive animals, BP, PWV and other hemodynamic parameters were measured as described below.
Animals
Male Fisher rats (3–6-months old (n=8) and 19–20-months old (n=7)) and male spontaneously hypertensive rats (SHR, 2-months (n=4), 3-months old (n=1), total of five animals in that group, and 12-months old (n=6)) were used in compliance with federal, state, local and National Research Council guidelines. All the surgical procedures and experimental protocols were approved by the Institutional Animal Care and Use Committee, which is fully accredited by the American Association for Accreditation in Laboratory Animal Care.
Invasive BP and PWV measurements
Animals were anesthetized with isoflurane, positioned supine on a temperature-controlled surface (Cole-Parmer, Vernon Hills, IL, USA) with extremities taped, and anesthesia maintained with 1.5% isoflurane (in 100% O2). Body temperature was maintained at 37 °C and a three-electrode electrocardiogram was recorded continuously (AD Instruments, Colorado Springs, CO, USA). After local anesthesia (2% lidocaine), a cervical midline excision was performed and the left carotid artery exposed. A 1.6F dual pressure catheter (Scisence, London, ON, Canada) was inserted into the thoracic aorta with the distal tip located just above the diaphragm and the proximal tip 2 cm proximal to the distal tip, below the aortic arch to continuously measure BP (LabChart 6, AD Instruments). A left jugular venous catheter was placed and a phenylephrine infusion was titrated to a systolic BP of 200 mm Hg. The infusion was then stopped allowing BP to slowly return to baseline. Calculations of both PP and PWV were made after the infusion was discontinued (during the period when BP returned to baseline). We excluded data with extreme values of PWV either below 2.5 m s−1 or above 8 m s−1, which we attributed to artifact or premature ventricular contractions.
Vascular indices
PP was calculated as the difference between the systolic and the corresponding diastolic BP measured at the catheter tip. PWV was calculated as the ratio of the separation distance (2 cm) to the time difference between pulse arrival at the proximal and distal pressure measuring points (LabChart 6, AD Instruments).21, 22 Calculation of the AASI was performed as described previously.10 In brief, multiple values of systolic and diastolic BP were obtained, plotted against each other, and the slope of a linear regression was determined with the AASI defined as one minus this value.10 Stiffer vasculature is characterized by an AASI approaching 1, with more compliant vasculature characterized by lower values. The CAVI was calculated as described previously.23, 24 Briefly, CAVI is calculated using the following formula:

where SBP is systolic BP, DBP is diastolic BP, ρ is blood density, and a and b are conversion constants. We report an adjusted value for this index: (CAVI−b) / (2 ρ a).
Data analysis
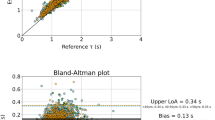
A standard quadratic regression was used to characterize the properties of individual animals. A mixed model regression was used to characterize the entire set of data with random intercepts for each animal. With the exception of the data determining the AASI, which is characterized by the slope of a liner regression, all other data were fit to quadratic equations using the age of the animal (young or old) as a factor. Independent variables also included the pressure, the square of pressure and interactions between both of these and whether the animal was young or old. In the event that the coefficient for any of these independent variables was not significant at the P=0.05 level, the regression was repeated without this independent variable. Any instances of this are noted in the legend accompanying the relevant figure. Use of random effects for other than the intercept was generally not revealing. Therefore, only random intercepts for each animal are used throughout. Confidence intervals (95% CI) were created from the estimates of the standard error of the regression curves. Equations from regression of PWV and PP as a function of diastolic pressure were used to generate a parametric plot indicating the relationship between PWV and PP as diastolic pressure increases. Data manipulation, figure preparation and statistical inference were facilitated by the use of Mathematica 8.0 (Wolfram Research, Champaign, IL, USA) and Stata 12.1 (StataCorp, College Station, TX, USA). The ASI was calculated from the slope of the midline between the data of a parametric plot of PWV vs. PP as diastolic BP is increased. The simplified ASI was created from the relationship between PWV and PP as a ratio of PWV/PP for any single measurement. To compare the proposed measure of arterial stiffness against a more established one, we used the approach suggested by Bland and Altman25 that addresses the concern that these measures differ in scale. Regression was used to predict the established measure from the proposed one. The next step is to determine whether the variability in these predictions falls within an acceptable range. Bland and Altman propose looking at the 95% prediction error bands of the regression and accepting the new measure if this variation was clinically or physiologically insignificant, a determination requiring problem-specific insight. Insofar as vascular stiffness is concerned, there is little to guide this judgement. Therefore, the mean and 95% CI of the predictions were determined for each of the four groups of animals used in this study and differences between younger and older animals qualified with a two-sided T-test. The ability to distinguish younger and older animals using the predicted values was then contrasted with the ability to do so from the original measurements.
Results
Baseline data
Baseline physiological data are presented in Table 1. There was no difference in BP (either systolic, diastolic or mean) between young and old Fisher rats, as well as young SHRs. Old SHRs had significantly higher BP than any of the other groups. The total phenylephrine dose required to render the animals hypertensive was relatively low in SHRs, likely owing to the elevated baseline BP in old SHRs and the accentuated response to phenylephrine in young SHRs. Old Fisher rats required a relatively high dose to achieve adequate BPs for the experiments.
Relationship between PWV and age
For each animal, both in the young and old group, PWV varied greatly during the experiment, with no difference in the mean PWV between young and old Fisher rats, both groups being normotensive (mean PWV (95% CI): young 4.52 (4.20, 4.84) m s−1; old 4.88 (4.53, 5.22) m s−1 (P=0.137); mean BP (s.d.): young 85.7 (11.0) mm Hg; old 90.6 (15.6) mm Hg (P=0.487)). There was a significant difference in PWV between young and old SHRs in old SHRs (mean PWV (95% CI): young SHRs 5.18 (4.85, 5.50) m s−1; old SHRs 6.02 (5.73, 6.32) m s−1 (P<0.001); mean BP (s.d.): young SHRs 95.4 (36.8) mm Hg; old SHRs 145 (16.8) mm Hg (P=0.025)).
Relationship between PWV and BP
PWV monotonically but nonlinearly increases with systolic, diastolic and mean BP in both young and old normotensive Fisher rats (Figure 1). Figure 1a shows scatter plots of PWV for a single young (left) and old Fisher rat (right) as a function of diastolic, mean and systolic BP, along with corresponding quadratic fits for that animal’s data. Figure 1b shows quadratic fits of PWV as a function of diastolic BP for each young (left) and old Fisher rat (right). Fits of PWV to diastolic, mean and systolic BP are drawn in Figure 1c for all young (left) and old (right) Fisher rats. The incremental increase in PWV is more prominent at higher BPs and is especially prominent for diastolic BP compared with systolic BP. Aging is associated with a less curvilinear relationship. The curves for PWV as a function of diastolic BP are distinctly different, differing in all parameters (intercept, linear, quadratic) between young and old (P<0.001). A direct comparison of the relationship between PWV and diastolic BP is illustrated in the left panel of Figure 1d along with 95% CIs. See also Table 2 for a quantitative comparison of the data. Above a diastolic BP of 80 mm Hg, PWV is slightly higher for any given BP in old Fisher rats compared with young animals. The right panel of Figure 1d compares all four animal groups in one graph by adding the information obtained from SHRs (the young and old SHRs differed significantly for all parameters of the quadratic regression (P<0.001)).
Pulse wave velocity (PWV) as a function of blood pressure (BP). (a) For a single representative young (left) or old Fisher rat (right), scatter plots of PWV as a function of diastolic, mean and systolic BP are given along with corresponding quadratic fits to that individual animal’s data. (b) Quadratic fits of PWV as a function of diastolic BP for each young (left) and old Fisher rat (right). (c) Quadratic relationships between PWV and diastolic, mean and systolic BP as determined from the data from all young (left) or old Fisher rats (right). (d, left) Quadratic fits of PWV as a function of diastolic BP for all young (solid line, light gray) and old (dashed line, dark gray) Fisher rats, with 95% prediction error bands. (d, right) Quadratic fits of PWV as a function of diastolic BP for all young (solid thin line) and old (dashed thin line) Fisher rats, as well as for all young (solid thick line) and old (dashed thick line) SHRs.
Relationship between PP and BP
PP also exhibits a non-linear monotonically increasing relationship with BP with this rate of increase more pronounced at higher BP (Figure 2). Figure 2a shows scatter plots of PP for a representative young (left) and old Fisher rat (right) as a function of diastolic, mean and systolic BP, along with corresponding quadratic fits to that animal’s data. Figure 2b shows quadratic fits of PP as a function of diastolic BP for each young (left) and old Fisher rat (right). Fits of PP to diastolic, mean and systolic BP are given in Figure 2c for all young (left) and old (right) animals. Differences between young and old animals appear most pronounced for diastolic BP. Overall, the relationship of PP and diastolic BP are distinct in all parameters of the curves for young and old animals (P<0.001) with less overlap of the respective curves than for similar data for PWV (Figure 1). The left panel of Figure 2d depicts quadratic fits of PP as a function of diastolic BP for all young and all old Fisher rats with corresponding 95% CIs. The incremental increase in PP is more prominent at higher BPs, and in young animals, while old animals show a marked flattening of the non-linear PP BP relationship. The right panel of Figure 2d compares all four animal groups in one graph by adding the information obtained from SHRs (the young and old SHRs differed significantly for the quadratic term of the quadratic fits (P<0.001)). See Table 2 for a quantitative comparison of the data.
Pulse pressure (PP) as a function of blood pressure (BP). (a) For the same representative young (left) or old (right) Fisher rat as in Figure 1, scatter plots of PP as a function of diastolic, mean and systolic BP are given along with corresponding quadratic fits to that individual animal’s data. (b) Quadratic fits of PP as a function of diastolic BP for each young (left) and old (right) Fisher rat. (c) Quadratic relationships between PP and diastolic, mean and systolic BP as determined from the data from all young (left) or old (right) Fisher rats. (d, left) Quadratic fits of PP as a function of diastolic pressure for all young (solid line, light gray) and old (dashed line, dark gray) Fisher rats with 95% prediction error bands. (d, right) Quadratic fits of PP as a function of diastolic BP for all young (solid thin line) and old (dashed thin line) Fisher rats, as well as for all young (solid thick line) and old (dashed thick line) SHRs.
Evaluation of the AASI and the CAVI
Our data demonstrate a very close relationship between diastolic and systolic BP in both young and old Fisher rats. Figure 3a shows scatter plots of diastolic BP vs. systolic BP for a representative young (left) and old Fisher rat (right), which is the same animal used as an example in all figures where examples are given. A summary for all Fisher rats is given in Figure 3b. Calculating the AASI for old vs. young animals showed that the difference between the two age groups is 15%. The left panel in Figure 3c shows the combined data for young and old Fisher rats, while the rat panel adds the information obtained from SHR animals (Fisher rats: slopes differ 15%: young Fisher rats: 0.617 95% CI (0.615, 0.620); old Fisher rats: 0.715 95% CI (0.715, 0.718), P<0.001; SHRs: slopes differ 2%, young SHRs: 0.690 (0.688, 0.691); old SHRs: 0.703 (0.701, 0.706), P<0.001). See Table 2 for a quantitative comparison of the data.
Ambulatory Arterial Stiffness Index (AASI). (a) For the single young (left) or old (right) Fisher rat used in Figure 1, scatter plots of diastolic blood pressure (BP) as a function of systolic BP are given along with corresponding linear fits to that individual animal’s data. (b) Linear fits of diastolic BP as a function of systolic BP for each young (left) and old (right) Fisher rat. (c, left) Linear fits of diastolic BP as a function of systolic BP for all young (solid line, light gray) and old (dashed line, dark gray) animals, with 95% prediction error bands. The intercept at 0 mm Hg (95% confidence interval (CI)) and slope (95% CI) are, respectively, 1.3 (−0.4, 3.0) mm Hg and 0.617 (0.615, 0.620) for the young Fisher rats, and −11.8 (−13.6, −10.1) mm Hg and 0.715 (0.712, 0.718) for the old Fisher rats. (c, right) Linear fits of diastolic BP as a function of systolic BP for all young (solid thin line) and old (dashed thin line) Fisher rats, as well as for all young (solid thick line) and old (dashed thick line) spontaneously hypertensive rats (SHRs). Although the slopes are distinct between the young and old animals for each type of animal, these differences are barely perceptible in the figure (15% for Fisher rats and 2% for SHRs).
In contrast to PWV (Figure 1) and PP (Figure 2), the relationship between CAVI and BP is not necessarily monotonic, though it does vary with BP in a non-linear manner both in young and old Fisher rats (Figure 4). Figure 4a shows scatter plots of CAVI for a single young (left) and old Fisher rat (right) as a function of diastolic, mean and systolic BP, along with corresponding quadratic fits. Figure 4b shows quadratic fits of CAVI as a function of diastolic BP for each young (left) and old Fisher rat (right). Fits of CAVI to diastolic, mean and systolic BP are given in Figure 4c for all young (left) and old (right) animals. Although the curves in old and young animals are significantly different (P<0.001), there is considerable overlap (Figure 4d, left). Importantly, considerable variation and BP dependence is apparent from the significantly non-zero (P<0.001) linear and quadratic terms of the curves illustrated. The right panel in Figure 4d also includes the data from the SHRs and compares the CAVI with the Fisher rats (the young and old SHRs differed significantly for all parameters of the quadratic fits (P<0.001)).
Cardio-Ankle Vascular Index (CAVI). (a) For the same single young (left) or old (right) Fisher rat used in Figure 1, scatter plots of adjusted CAVI as a function of diastolic, mean and systolic blood pressure (BP) are given along with corresponding quadratic fits to that individual animal’s data. (b) Quadratic fits of adjusted CAVI as a function of diastolic BP for each the young (left) and old (right) Fisher rat. (c) Quadratic relationships between adjusted CAVI and diastolic, mean or systolic BP as determined from the data from all young (left) or old (right) Fisher rats. (d, left) Quadratic fits of adjusted CAVI as a function of diastolic BP for all young (solid line, light gray) and old (dashed line, dark gray) animals, with 95% prediction error bands. (d, right) Quadratic fits of adjusted CAVI as a function of diastolic BP for all young (solid thin line) and old (dashed thin line) Fisher rats, as well as for all young (solid thick line) and old (dashed thick line) spontaneously hypertensive rats (SHRs).
Relationship between PWV and PP: Arterial Stiffness Index (ASI)
PWV and PP show a similar pattern of BP dependency in young and old animals. Therefore, we evaluated the relationship between PWV and PP directly and observed that it varies nonlinearly, but monotonically in both young and old animals (Figure 5). It is not possible to compare the ASI directly with the AASI because they differ in scale, though some comparison is desirable. Therefore, as described in Methods, the ASI measurements for each animal from all four groups were used to predict the AASI. The mean and 95% CIs were then generated for each of the four animal groups. For the younger and older Fischer rats, the predicted AASI are, respectively, 0.610 (0.604, 0.616) and 0.667 (0.621, 0.712) with P=0.024 indicating that these groups remain distinguishable, though the predicted values of the AASI lie outside of the CIs of the original determinations summarized in Table 2. For the young and old SHR animals, the predicted AASI are, respectively, 0.635 (0.587, 0.659) and 0.663 (0.647, 0.672) with P=0.26, indicating that the predicted AASI do not readily distinguish between the older and younger animals. However, this is consistent with the determinations of the ASI, which clearly separates the young and old Fisher rats, being more similar, but distinguishable, for the SHR animals.
Arterial Stiffness Index (ASI). (a) Relationship between pulse wave velocity (PWV) and pulse pressure (PP) for the same single young (left) or old (right) Fisher rat as in Figure 1, are given along with corresponding quadratic fits to that individual animal’s data. (b) Quadratic fits of PWV as a function of PP for each young (left) and old (right) Fisher rat. (c) Quadratic fits of PWV as a function of PP for all young (solid line, light gray) and old (dashed line, dark gray) Fisher rats (left) with 95% prediction error bands. The relationship between PWV and PP as diastolic blood pressure (BP) increases is also given in c (right) for all young (solid) and old (dashed) Fisher rats. These curves were constructed from the relationships between PWV and diastolic BP of Figure 1, and those between PP and diastolic BP of Figure 2. For each value of diastolic BP, the corresponding values of PWV and PP are plotted to obtain the parametric curves as diastolic BP increases shown to the right of c. Each point corresponds to a specific value of diastolic BP. The slope of the midpoint between the data was defined as the ASI. (d) Quadratic fits of PWV as a function of PP for all young (solid thin line) and old (dashed thin line) Fisher rats, as well as all young (solid thick line) and old (dashed thick line) spontaneously hypertensive rats (SHRs) (left). The relationship between PWV and PP as diastolic BP increases is also given in c (right) for all young (solid thin line) and old (dashed thin line) Fisher rats, as well as all young (solid thick line) and old (dashed thick line) SHRs.
Figure 5a shows scatter plots of PWV for a single young (left) and old Fisher rat (right) as a function of PP, along with corresponding quadratic fits. Figure 5b shows quadratic fits of PWV as a function of PP for each young (left) and old Fisher rat (right). Quadratic fits of PWV as a function of PP for all young and old animals with 95% prediction error bands are in given in Figure 5c (left) and differ in each coefficient of the fit (P<0.001). Above the intersection point, PWV is significantly greater for PPs in old animals compared with young ones. The slope of the midpoint between the data of a parametric plot of PWV vs. PP as diastolic pressure is increased (Figure 5c, right), yields the ASI. The numerical value of the ASI is more than twice as high for old animals vs. young animals (young normotensive Fisher rats: 0.0352 m s−1 mm Hg−1, 95% CI (0.0345, 0.0359), old normotensive Fisher rats: 0.0769 m s−1mm Hg−1, 95% CI (0.0734,0.0805). Both curves intersect at PWV=4.3 m s−1, PP=51 mm Hg and a diastolic BP of 90 mm Hg. Paralleling the results in Fisher rats, PWV and PP in SHR animals show a similar pattern of BP and age dependency in young and old animals (Data not shown). Figure 5d compares all four groups adding young normotensive and old hypertensive SHRs, and Table 2 demonstrates a quantitative comparison of the data. The slope of the curve at the midpoint of the SHR data (and therefore the ASI) is virtually identical for old hypertensive SHR and old normotensive animals, but the curve is shifted upwards, (old hypertensive SHR 0.076 m s−1 mm Hg−1, 95% CI (0.069,0.086); young normotensive SHR: 0.095 m s−1 mm Hg−1, 95% CI (0.087, 0.103); P<0.001 in all parameters of the quadratic fits). The fact that the slope for the young normotensive SHRs is steeper than that for the young normotensive Fischer rates suggests that vascular stiffness is already higher in these animals even before they become markedly hypertensive.
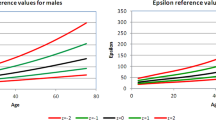
Relationship of PWV/PP to BP
The relationship between the ratio of PWV and PP as a function of diastolic, mean and systolic BP decreases non-linearly and monotonically in young normotensive Fisher rats (Figures 6a and b, left panels). In contrast, the PWV/PP in relation to BP either monotonically increases or remains unchanged for most old normotensive Fisher rats (Figures 6a and b, right panels). Figure 6a depicts scatter plots of the ratio of PWV and PP for a single young (left) and old Fisher rat (right) as a function of diastolic, mean and systolic BP, along with corresponding fits to that animal’s data. Figure 6b shows the ratio of PWV and PP as a function of diastolic BP for each young (left) and old Fisher rat (right). Figure 6c demonstrates that clear differences between young and old normotensive Fisher rats and between young normotensive SHR and old hypertensive SHR can be detected (P<0.001). Similar to the ASI, young normotensive SHRs exhibit a pattern closely resembling old normotensive Fisher rats. However, the PWV/PP to diastolic BP profile of old hypertensive Fisher rats is shifted upwards (Figure 6c, right). Furthermore, despite the proximity in the right panel of Figure 6c, differences in regression parameters between young normotensive Fisher rats and young normotensive SHRs are present (P <0.001, in all terms), with differences between old normotensive Fisher rats and old hypertensive SHRs being visibly and statistically distinct (P<0.001, in all terms). See Table 2 for a quantitative comparison of the data.
The relation of pulse wave velocity (PWV)/pulse pressure (PP) to blood pressure (BP). (a) The ratio of PWV and PP as a function of diastolic, mean and systolic BP for the same single young (left) or old (right) Fisher rat as in Figure 1, are given along with corresponding quadratic fits to that individual animal’s data. (b) Quadratic fits of PWV/PP as a function of diastolic BP for each young (left) and old (right) normotensive Fisher rat. (c, left) Quadratic fits of PWV/PP as a function of diastolic BP for all young (solid line, light gray) and old (dashed line, dark gray) Fisher rats, with 95% prediction error bands. (c, right) Quadratic fits of PWV/PP as a function of diastolic BP for all young (solid thin line) and old (dashed thin line) Fisher rats, as well as for all young (solid thick line) and old (dashed thick line) spontaneously hypertensive rats (SHRs).
Discussion
We have previously demonstrated that compared with young animals, old Fisher rats display markedly elevated vascular stiffness as evidenced by tensile testing, PWV-MAP relationship and endothelial dysfunction.21 In these studies, we demonstrate that both PWV and PP increase in a non-linear but monotonic manner with rising BPs, with the increase being more pronounced for diastolic BP than for mean or systolic BP. Aging markedly changes the relationship between PWV or PP and BP to a less curvilinear shape. The previously described AASI significantly distinguishes the vasculature of young and old animals, while the CAVI is BP-dependent (Figures 3 and 4). In our model, the novel marker for arterial stiffness (ASI) differentiates the vasculature of old normotensive animals from young normotensive animals, which vary in arterial stiffness, with a markedly higher value for old animals (Figure 5). Similarly, both normotensive and hypertensive SHRs have a markedly increased ASI compared with young normotensive Fisher rats.
It has been demonstrated previously that PWV changes with BP,26, 27 and those results are confirmed by our study (Figure 1). Therefore, PWV by itself is a poor indicator in its ability to differentiate intrinsic arterial stiffness given the high variability of PWV and its BP dependency. The BP dependency of PWV has spurred the search for an array of 'normal values', to predict clinical outcomes and to use PWV as an index of intrinsic vascular stiffness.20, 28 This makes PWV more cumbersome to use in the clinical setting, given that for an individual patient, different measurements of PWV should be obtained when his/her BP changes, even though intrinsic arterial stiffness remains unchanged. Nevertheless, arterial stiffness and PWV are closely linked by their shared risk factors and the associated increase in cardiovascular morbidity and mortality, which makes PWV an independent predictor of cardiovascular events in the general population and in patients with hypertension, diabetes, renal insufficiency or coronary artery disease.15, 29, 30, 31, 32 It is, however, not a specific marker for arterial stiffness.15, 17, 33 Moreover, PWV exhibits a correlation with other established cardiovascular risk factors, such as age, male gender, smoking, obesity, diabetes mellitus and BP, all of which have been reported to be a predictor of arterial stiffness.34, 35 The same is true for PP. It is easy to obtain (difference between systolic and diastolic BP) and is predictive of cardiovascular morbidity36, 37—but it also varies greatly with BP (Figure 2). Given that PP and PWV are both similarly BP-dependent, we investigated the direct relationship between PWV and PP to minimize the influence of BP and to unmask intrinsic vascular stiffness (Figure 5). We hypothesize that relating PWV and PP directly will minimize the effects of BP on PWV and PP. Our data demonstrate that above the range for PP values in normotensive rats, there is a progressive increase in PWV that is more pronounced in older and stiffer vessels of old rats (Figure 5c, left panel). This intersection presumably represents the starting point at which the stiffer components of the vascular matrix (for example, collagen) predominate over elastic and pulsatile matrix components. Therefore, the contribution of the 'passive' mechanical properties of the arterial wall tension and hence PWV become predominant. This is most likely due to a greater percentage of stiffer components in the vascular matrix (for example, collagen) from old animals compared with young.38
During isovolumic contraction, the left ventricle generates pressure until it reaches the aortic diastolic BP, at which point ejection begins. This marks the first hemodynamic reference point (diastolic pressure), which we have used for the non-parametric plots. Ejection of blood that follows aortic valve opening generates both PP and the speed at which the pulse wave travels along the vasculature (PWV). Both PP and PWV depend on BP, which in turn depends on cardiovascular coupling. Consequently, increases in stroke volume, vascular impedance or contractility result in increases in PP and PWV. As PP and PWV also depend on wall tension and compliance, decreased vascular compliance or increased wall tension lead to higher PP and PWV and vice versa. Furthermore, our results demonstrate that increases in PP are smaller when compared with increases in PWV with stiffening of the aorta in old animals. This could be explained by the fact that the ejected stroke volume stretches the proximal segment of the aorta (generating PP) to a point at which the vessel cannot stretch any further. The stroke volume is forced forward to the next un-stretched segment of aorta until the complete stroke volume is accommodated by the central vasculature. Stiff old vessels are much less compliant and hence favor the forward spread of the pulse wave (increased PWV for the same increase in PP). To better delineate this difference, we investigated the relationship between PP and PWV, generated by each individual stroke volume ejected. This should minimize or eliminate the effects of BP on the direct comparison of PWV and PP, as BP has similar effect on both parameters, thereby canceling out its effect on the PWV/PP relationship. Parametric plots of quadratic fits for PWV vs. PP as diastolic BP increases provided the best separation between animals. We defined the slope of the midpoint between the data of this relationship between PP and PWV as the Arterial Stiffness Index (ASI, Figure 5c, right panel). Therefore, by definition and similar to the AASI, calculation of the ASI requires multiple measurements and different diastolic BPs. In our model, the slope more than doubles for old vs. young animals making the ASI a marker for subtle changes in vascular stiffness associated with aging, with high values indicating high vascular stiffness. Ultimately, these calculations can be performed by software on commercially available equipment that already measures PWV. This would provide the clinician with supplemental prognostic information for all patients, would be easy to obtain and does not necessarily require 24-h BP measurements.
We tested the ASI in a model of hypertension and aging by repeating the invasive measurements in young normotensive and old hypertensive SHRs, which are very similar to Fisher rats, but do have a different genetic background. The slope of the curve and therefore the ASI is virtually identical for old hypertensive SHRs and old normotensive Fisher rats but is shifted upwards (0.076 m s−1mm Hg−1 for old hypertensive SHRs, 0.077 m s−1mm Hg−1 for old normotensive Fisher rats, Figure 5d). The quadratic fits of PWV as a function of PP for young normotensive SHRs is steeper than that for young normotensive Fisher rats (young normotensive SHR: 0.095 m s−1mm Hg−1, young normotensive Fisher rats: 0.035 m s−1mm Hg−1), indicating that both young normotensive and old hypertensive SHRs have a stiff vasculature. This suggests that, in our animals, increased vascular stiffness precedes the development of marked hypertension during the aging of SHRs, which is contrary to some prior studies in the literature.39, 40 Nevertheless, our young SHRs while still being normotensive at baseline, showed dramatic increases in PP and PWV when BP was elevated pharmacologically during the experiment.
Lastly, we describe the relationship between PWV and PP as a ratio of PWV/PP for any single measurement point instead of the slope from multiple measurements. This PWV/PP index is also able to differentiate stiff vasculature in hypertensive SHRs from normotensive Fisher rats and normotensive SHRs (Figure 6c). This simplified ASI demonstrates that hypertensive old SHRs have a higher PWV for identical BPs than normotensive SHRs and Fisher rats. The benefit of the simplified ASI is that it could potentially be used clinically to differentiate stiff from compliant vasculature at any given BP without the need for multiple measurements. The issue of PWV dependence on BP may be resolved with the simplified ASI, because in stiff vasculature, the simplified ASI will stay the same, but in compliant vasculature, if anything, it will decrease with increases in BP. This potentially allows one to compare vascular stiffness between patients given that their PWV may have been measured at a different BP. Our data show that young normotensive Fisher rats exhibit a decreasing PWV/PP ratio over the spectrum of diastolic BPs, while old normotensive Fisher rats and young normotensive SHRs demonstrate a constant ratio of PWV/PP over the measured diastolic BP spectrum. This relationship is shifted upwards in old hypertensive SHRs (Figure 6). These results, possibly indicate that vascular stiffness is already higher in young SHRs before they develop hypertension while the addition of hypertension in the old SHRs results in an upward shift of the PWV/PP relationship.2 This would indicate that, in our model, vascular stiffness could be the initial pathological change in the vasculature before the animals become markedly hypertensive, which is consistent with some studies41, 42, 43 but contrary to some others.39, 40 Furthermore, the development of hypertension and therefore changes in BP does not negatively affect the ASI but rather leads to a shift in the relationship of PWV and PP without significantly changing the slope (defined as ASI).
To compare the ASI with the AASI, we invasively measured thousands of data points per animal, which enabled us to perform precise calculations with very little variation. Both were able to differentiate old from young vasculature, however, the difference in the slope, though statistically significant, was 15% for the AASI and 2% for the SHRs in this very homogeneous data set, with the ASI demonstrating a more than 100% difference between the two groups (Figure 5). This might be partially owing to the fact that the AASI distinguishes between stiffer vessels from compliant vessels based on the assumption that stiffer vessels have a disproportionate increase in systolic BP compared with diastolic BP, which is not as pronounced in our data except at the extremes of BP, where PP increases disproportionally in young animals (Figure 2). Furthermore, the AASI and ASI assay different features of arterial stiffness. The AASI uses the entire BP range, whereas the ASI is determines where the slope of the underlying curve becomes asymptotically linear reflecting vascular features of higher BPs.
Next, we compared the ASI with the CAVI, which has been shown to have a good correlation with cardiovascular risk factors being predictive of clinical outcomes.44 However, the CAVI was also shown to be strongly affected by different antihypertensive regimens and as not being BP-independent as initially thought, as confirmed by our data (Figure 4),45, 46 but it differentiated the different vascular beds. The reason for that is that the CAVI might not only reflect intrinsic vascular wall matrix composition but also the contractile state of the vessel wall. In this context, it is not surprising that in our experiment, where we achieved BP variation by pharmacologic manipulation, CAVI was strongly dependent on BP probably reflecting different states of vascular contraction (Figure 4).
Here, we propose a novel index of vascular stiffness that can be used to non-invasively compare different vascular beds. It is inherently difficult to isolate one or two parameters in an in vivo experiment while controlling all other variables. In our experimental setting, we strived to control for confounding hemodynamic parameters by maintaining a constant volume status and an identical depth of anesthesia in all animals. To manipulate BP, we used an alpha agonist without directly changing inotropy or heart rate. We therefore assumed that the observed changes in BP and PWV are predominantly due to changes in vascular tone and SVR and not due to increases in contractility, heart rate or stroke volume—which could bias our results. Furthermore, to establish either the ASI or the simplified ASI as a surrogate end point for identifying cardiovascular risk, there is a need to demonstrate that a low ASI is predictive of cardiovascular risk. Also, similar experiments need to be carried out in patients to validate this index in the clinical setting. Lastly, multiple measurements at different BPs need to be taken to reliably calculate the ASI, whereas the simplified ASI may be obtained by only a single measurement. We believe that these indices might potentially be useful in assessing the effectiveness of new drugs targeting intrinsic vascular stiffness and to distinguish the effects of BP modulation from vascular wall remodeling elicited by currently available drugs.
References
Franklin SS . Hypertension in older people: part 1. J Clin Hypertens (Greenwich) 2006; 8: 444–449.
Mitchell GF . Arterial stiffness and hypertension: chicken or egg? Hypertension 2014; 64: 210–214.
Cattell MA, Anderson JC, Hasleton PS . Age-related changes in amounts and concentrations of collagen and elastin in normotensive human thoracic aorta. Clin Chim Acta 1996; 245: 73–84.
O'Rourke MF, Hashimoto J . Mechanical factors in arterial aging: a clinical perspective. J Am Coll Cardiol 2007; 50: 1–13.
Kass DA . Age-related changes in venticular-arterial coupling: pathophysiologic implications. Heart Fail Rev 2002; 7: 51–62.
Huynh J, Nishimura N, Rana K, Peloquin JM, Califano JP, Montague CR, King MR, Schaffer CB, Reinhart-King CA . Age-related intimal stiffening enhances endothelial permeability and leukocyte transmigration. Sci Transl Med 2011; 3: 112ra122.
Pannier BM, Avolio AP, Hoeks A, Mancia G, Takazawa K . Methods and devices for measuring arterial compliance in humans. Am J Hypertens 2002; 15: 743–753.
Mackenzie IS, Wilkinson IB, Cockcroft JR . Assessment of arterial stiffness in clinical practice. QJM 2002; 95: 67–74.
Otsuka K, Fukuda S, Shimada K, Suzuki K, Nakanishi K, Yoshiyama M, Yoshikawa J . Serial assessment of arterial stiffness by cardio-ankle vascular index for prediction of future cardiovascular events in patients with coronary artery disease. Hypertens Res 2014; 37: 1014–1020.
Dolan E, Thijs L, Li Y, Atkins N, McCormack P, McClory S, O'Brien E, Staessen JA, Stanton AV . Ambulatory arterial stiffness index as a predictor of cardiovascular mortality in the Dublin Outcome Study. Hypertension 2006; 47: 365–370.
Xu TY, Li Y, Fan WX, Li FH, Zou J, Gao PJ, Staessen JA, Wang JG . Ambulatory (AASI), but not home (HASI), arterial stiffness index is associated with aortic pulse wave velocity. Hypertens Res 2011; 34: 402–403.
Xu TY, Li Y, Wang YQ, Li YX, Zhang Y, Zhu DL, Gao PJ . Association of stroke with ambulatory arterial stiffness index (AASI) in hypertensive patients. Clin Exp Hypertens 2011; 33: 304–308.
Mitchell GF, Izzo JL Jr, Lacourciere Y, Ouellet JP, Neutel J, Qian C, Kerwin LJ, Block AJ, Pfeffer MA . Omapatrilat reduces pulse pressure and proximal aortic stiffness in patients with systolic hypertension: results of the conduit hemodynamics of omapatrilat international research study. Circulation 2002; 105: 2955–2961.
Mitchell GF, Hwang SJ, Vasan RS, Larson MG, Pencina MJ, Hamburg NM, Vita JA, Levy D, Benjamin EJ . Arterial stiffness and cardiovascular events: the Framingham Heart Study. Circulation 2010; 121: 505–511.
Laurent S, Boutouyrie P, Asmar R, Gautier I, Laloux B, Guize L, Ducimetiere P, Benetos A . Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension 2001; 37: 1236–1241.
Sutton-Tyrrell K, Najjar SS, Boudreau RM, Venkitachalam L, Kupelian V, Simonsick EM, Havlik R, Lakatta EG, Spurgeon H, Kritchevsky S, Pahor M, Bauer D, Newman A . Elevated aortic pulse wave velocity, a marker of arterial stiffness, predicts cardiovascular events in well-functioning older adults. Circulation 2005; 111: 3384–3390.
Mattace-Raso FU, van der Cammen TJ, Hofman A, van Popele NM, Bos ML, Schalekamp MA, Asmar R, Reneman RS, Hoeks AP, Breteler MM, Witteman JC . Arterial stiffness and risk of coronary heart disease and stroke: the Rotterdam Study. Circulation 2006; 113: 657–663.
Seidlerova J, Filipovsky J, Mayer O, Wohlfahrt P, Cifkova R . Positive effects of antihypertensive treatment on aortic stiffness in the general population. Hypertens Res 2014; 37: 64–68.
Steppan J, Barodka V, Berkowitz DE, Nyhan D . Vascular stiffness and increased pulse pressure in the aging cardiovascular system. Cardiol Res Pract 2011; 2011: 263585.
Reference Values for Arterial Stiffness' Collaboration. Determinants of pulse wave velocity in healthy people and in the presence of cardiovascular risk factors: 'establishing normal and reference values'. Eur Heart J 2010; 31: 2338–2350.
Steppan J, Sikka G, Jandu S, Barodka V, Halushka MK, Flavahan NA, Belkin AM, Nyhan D, Butlin M, Avolio A, Berkowitz DE, Santhanam L . Exercise, vascular stiffness, and tissue transglutaminase. J Am Heart Assoc 2014; 3: e000599.
Ng K, Hildreth CM, Phillips JK, Avolio AP . Aortic stiffness is associated with vascular calcification and remodeling in a chronic kidney disease rat model. Am J Physiol Renal Physiol 2011; 300: F1431–F1436.
Ibata J, Sasaki H, Kakimoto T, Matsuno S, Nakatani M, Kobayashi M, Tatsumi K, Nakano Y, Wakasaki H, Furuta H, Nishi M, Nanjo K . Cardio-ankle vascular index measures arterial wall stiffness independent of blood pressure. Diabetes Res Clin Pract 2008; 80: 265–270.
Shirai K, Utino J, Otsuka K, Takata M . A novel blood pressure-independent arterial wall stiffness parameter; cardio-ankle vascular index (CAVI). J Atheroscler Thromb 2006; 13: 101–107.
Bland JM, Altman DG . Applying the right statistics: analyses of measurement studies. Ultrasound Obstet Gynecol 2003; 22: 85–93.
Nye ER . The effect of blood pressure alteration on the pulse wave velocity. Br Heart J 1964; 26: 261–265.
Hickson SK, McSwiney BA . The effect of variations in blood-pressure on pulse wave velocity in the brachial artery in man. J Physiol 1924; 59: 217–220.
Cecelja M, Chowienczyk P . Dissociation of aortic pulse wave velocity with risk factors for cardiovascular disease other than hypertension: a systematic review. Hypertension 2009; 54: 1328–1336.
Meaume S, Rudnichi A, Lynch A, Bussy C, Sebban C, Benetos A, Safar ME . Aortic pulse wave velocity as a marker of cardiovascular disease in subjects over 70 years old. J Hypertens 2001; 19: 871–877.
Pannier B, Guerin AP, Marchais SJ, Safar ME, London GM . Stiffness of capacitive and conduit arteries: prognostic significance for end-stage renal disease patients. Hypertension 2005; 45: 592–596.
Smith A, Karalliedde J, De Angelis L, Goldsmith D, Viberti G . Aortic pulse wave velocity and albuminuria in patients with type 2 diabetes. J Am Soc Nephrol 2005; 16: 1069–1075.
Katsuda S, Takazawa K, Miyake M, Kobayashi D, Kusanagi M, Hazama A . Local pulse wave velocity directly reflects increased arterial stiffness in a restricted aortic region with progression of atherosclerotic lesions. Hypertens Res 2014; 37: 892–900.
Vlachopoulos C, Aznaouridis K, Stefanadis C . Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol 2010; 55: 1318–1327.
Alecu C, Gueguen R, Aubry C, Salvi P, Perret-Guillaume C, Ducrocq X, Vespignani H, Benetos A . Determinants of arterial stiffness in an apparently healthy population over 60 years. J Hum Hypertens 2006; 20: 749–756.
Najjar SS, Scuteri A, Shetty V, Wright JG, Muller DC, Fleg JL, Spurgeon HP, Ferrucci L, Lakatta EG . Pulse wave velocity is an independent predictor of the longitudinal increase in systolic blood pressure and of incident hypertension in the Baltimore Longitudinal Study of Aging. J Am Coll Cardiol 2008; 51: 1377–1383.
Roman MJ, Devereux RB, Kizer JR, Lee ET, Galloway JM, Ali T, Umans JG, Howard BV . Central pressure more strongly relates to vascular disease and outcome than does brachial pressure: the Strong Heart Study. Hypertension 2007; 50: 197–203.
Benetos A, Okuda K, Lajemi M, Kimura M, Thomas F, Skurnick J, Labat C, Bean K, Aviv A . Telomere length as an indicator of biological aging: The gender effect and relation with pulse pressure and pulse wave velocity. Hypertension 2001; 37: 381–385.
Shadwick RE . Mechanical design in arteries. J Exp Biol 1999; 202: 3305–3313.
Morgan EE, Casabianca AB, Khouri SJ, Kalinoski AL . In vivo assessment of arterial stiffness in the isoflurane anesthetized spontaneously hypertensive rat. Cardiovasc Ultrasound 2014; 12: 37.
Safar M, Chamiot-Clerc P, Dagher G, Renaud JF . Pulse pressure, endothelium function, and arterial stiffness in spontaneously hypertensive rats. Hypertension 2001; 38: 1416–1421.
Franklin SS . Arterial stiffness and hypertension: a two-way street? Hypertension 2005; 45: 349–351.
Kaess BM, Rong J, Larson MG, Hamburg NM, Vita JA, Levy D, Benjamin EJ, Vasan RS, Mitchell GF . Aortic stiffness, blood pressure progression, and incident hypertension. JAMA 2012; 308: 875–881.
Mukherjee D . Atherogenic vascular stiffness and hypertension: cause or effect? JAMA 2012; 308: 919–920.
Nakamura K, Tomaru T, Yamamura S, Miyashita Y, Shirai K, Noike H . Cardio-ankle vascular index is a candidate predictor of coronary atherosclerosis. Circ J 2008; 72: 598–604.
Shirai K . Analysis of vascular function using the cardio-ankle vascular index (CAVI). Hypertens Res 2011; 34: 684–685.
Shirai K, Song M, Suzuki J, Kurosu T, Oyama T, Nagayama D, Miyashita Y, Yamamura S, Takahashi M . Contradictory effects of beta1- and alpha1- aderenergic receptor blockers on cardio-ankle vascular stiffness index (CAVI)—CAVI independent of blood pressure. J Atheroscler Thromb 2011; 18: 49–55.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Steppan, J., Sikka, G., Hori, D. et al. Seeking a blood pressure-independent measure of vascular properties. Hypertens Res 39, 27–38 (2016). https://doi.org/10.1038/hr.2015.109
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2015.109
Keywords
This article is cited by
-
What is important for aging-induced arterial stiffening, autonomic dysfunction, vascular characteristics or both?
Hypertension Research (2017)
-
Patient-specific blood pressure correction technique for arterial stiffness: evaluation in a cohort on anti-angiogenic medication
Hypertension Research (2017)
-
Ejection time: influence of hemodynamics and site of measurement in the arterial tree
Hypertension Research (2017)
-
New approach to arterial stiffness: BP-independent local carotid stiffness
Hypertension Research (2017)