Abstract
Increased arterial stiffness and wave reflections are independently associated with orthostatic hypotension (OH). This study investigated whether heart rate variability (HRV) is also involved in the modulation of orthostatic blood pressure (BP) change. A total of 429 subjects (65.1±16.4 years, 77.4% men) were enrolled in this study. OH was defined as a ⩾20 mm Hg decrease in brachial systolic blood pressure (SBP) or a ⩾10 mm Hg diastolic blood pressure (DBP) decrease upon standing. Measurements of carotid–femoral pulse wave velocity (cf-PWV) and the amplitude of the reflected pressure wave from a decomposed carotid pressure wave (Pb) were obtained by carotid tonometry in the supine position. The power spectrum from a 5-min recording of an electrocardiogram at rest was analyzed to provide components in the high frequency (HF) and low frequency (LF) ranges. Subjects with OH (n=59, 13.8%) had significantly higher cf-PWV and Pb and significantly lower LogHF and LogLF than those without OH (n=370). The cf-PWV, Pb, LogHF and LogLF were significantly associated with postural SBP and DBP changes. Furthermore, cf-PWV but not Pb was significantly associated with LogHF and LogLF. Multivariate analysis showed that Pb (odds ratio (OR) per 1 s.d. 1.65, 95% confidence interval (CI) 1.282–2.137; P=0.003) and LogHF (OR 0.628, 95% CI 0.459–0.860, P=0.004), but not cf-PWV (OR 1.279, 95% CI 0.932–1.755, P=0.128), were significant independent determinants of OH. Increased wave reflections may predispose OH independently of arterial stiffness and HRV. In contrast, increased arterial stiffness may cause OH through the modulation of HRV.
Similar content being viewed by others
Introduction
Maintaining blood pressure (BP) during postural changes is important for vital organ perfusion and becomes more difficult with advancing age, partly because of the age-related decline in baroreflex sensitivity (BRS).1 Excessive decreases in BP during the transition from the supine to the upright posture, or orthostatic hypotension (OH), may indicate a failure in the baroreflex function or its interaction with hemodynamic or humoral factors.1 OH is common in the elderly, is associated with cardiovascular disease2 and is predictive of ischemic stroke and transient ischemic attack.3, 4 In the elderly, OH has been identified as an independent predictor of falls5, 6 and mortality.7 Understanding the underlying mechanisms for OH is crucial for the prevention and management of its adverse consequences.
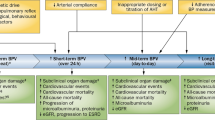
Aging is associated with increased arterial stiffness and arterial wave reflections, both of which are recognized as major determinants of BP and predictors of incident hypertension.8, 9 In the elderly, arterial stiffening enhances BP liability and may cause an excessive decrease in BP associated with the volume shift upon standing.10 Moreover, arterial stiffening may contribute to the age-associated reduction in BRS, as the arterial stretch over segments with the baroreceptors is a key determinant in baroreflex activation.1 In a large elderly study population, arterial stiffness assessed by carotid–femoral pulse wave velocity (cf-PWV) was associated with impaired BRS and orthostatic BP changes.11 In contrast, only a few, small studies have suggested an increase in wave reflections assessed by carotid augmentation index (cAI) as a risk factor for OH12 or syncope.13 Moreover, the link between wave reflections and baroreflex modulation has never been evaluated.
Spectral analysis evaluating heart rate variability (HRV) has widely been used as a noninvasive technique for examining the sympathetic and parasympathetic nervous outflows to the heart.14 Efferent vagal activity is a major contributor to the high-frequency (HF) power components in the HRV in the frequency domain,14 and HF may indicate efferent cardiovagal sensitivity of the baroreflex.1 Recently, the low-frequency (LF) power components in HRV have also been shown to correlate with the baroreflex function.15 Thus, power spectral analysis of HRV may provide a means to evaluate the ability to modulate autonomic outflows via the baroreflex.15, 16 However, the link between arterial stiffness and wave reflections to baroreflex modulation has never been evaluated. Therefore, the main purpose of the present study was to investigate whether the association of arterial stiffness and wave reflections with OH involves the modulation of HRV.
Methods
Study population
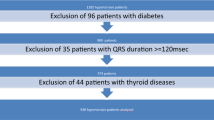
The present cohort was selected from among the previously reported study of 613 participants.17 Among them, 429 subjects had analyzable HRV data and comprised the subjects for this study (Table 1). The investigation conformed to the principles outlined in the Declaration of Helsinki, and an informed consent approved by our institutional review board was obtained from every subject before enrollment.
Study protocol
All participants underwent comprehensive assessments for arterial stiffness, wave reflections and postural BP changes as described in our previous work.18 The medical history, demographics and list of prescribed medications were recorded for each subject. Fasting blood samples were collected for hemoglobin and serum creatinine measurements. The estimated glomerular filtration rate (eGFR) was calculated by using a modified Modification of Diet in Renal Disease equation based on the Chinese population.19
Participants refrained from smoking or drinking beverages containing caffeine or alcohol for 24 h before the study and were studied under supine resting conditions in a quiet, temperature-controlled room. After resting for 10 min, a commercially available device (VP-2000; Colin, Komaki, Japan) incorporating four pressure cuffs and two tonometric probes was used to obtain the supine brachial systolic blood pressure (SBP) and diastolic blood pressure (DBP) from both arms, the heart rate and pressure waveforms from the right common carotid and right femoral arteries simultaneously.20, 21 Pulse pressure was the difference between the SBP and the DBP, and the mean arterial blood pressure (MAP) was computed as the DBP+1/3 pulse pressure. The BP and heart rate measurements were repeated 3 min after standing up. The BP value from the same arm at a higher supine brachial SBP was used for the present study. Orthostatic BP changes were calculated as the BP after standing minus the BP in the supine position. OH was defined as a drop of ⩾20 mm Hg in SBP or a drop of ⩾10 mm Hg in DBP.22
Measures of arterial stiffness and wave reflections
The cf-PWV was calculated from the traveling distance and the foot-to-foot pulse transit time between the right carotid and right femoral arteries.23 The inflection point originating from the wave reflection on the upstroke or downstroke of the carotid pressure waveform was identified by finding the zero-crossing timings of the fourth derivative of the pressure waveform.24 The cAI and carotid augmented pressures (cAP) were calculated accordingly.25 The carotid pressure waveform was also separated into its forward and backward components to calculate the transit time-independent parameter of wave reflection intensity using the validated triangulation method.25, 26 Pf and Pb were the amplitudes of the forward and backward pressure waves, respectively.25
Measures of HRV
After resting for at least 10 min in the supine position, a 5-min segment of ECG signal provided by an oscillometric device (VP-2000; Colin) was transmitted to a personal computer for storage and analysis. The sampling frequency for the ECG signal was 1000 Hz. R-waves were detected and the beat-to-beat RR intervals were determined. Sinus pause and atrial or ventricular arrhythmias were deleted. Short, missing or noisy segments were interpolated by linear splines. If the percentage of deletion was ⩾5%, the patient was excluded from the study. The beat-to-beat RR intervals were resampled at 4 Hz into an evenly spaced time series to generate a power spectrum with the fast Fourier transformation.27 The areas under the spectral peaks ranging 0.04–0.15 Hz, 0.15–0.40 and Hz 0.01–0.40 Hz (including the very LF range 0.01–0.04 Hz) were categorized as LF and HF components and total power (TP), respectively.
Statistical analysis
The mean values, s.d. and percentages were used to describe the characteristics of the participants in the study. Because the frequency domain indices of HRV had a markedly skewed distribution, the log transformation was utilized to permit parametric statistical comparisons that assumed a normal distribution. Student’s t-test and the χ2 test were used for comparisons between subjects with and without OH. Uni- and multivariate logistic regression analyses were performed to examine the associations between arterial stiffness, wave reflections and HRV with OH. Stepwise linear regression analysis was performed to examine the determinants of postural BP changes and HRV. A P-value of <0.05 was considered to be statistically significant, and all statistical analyses were performed using SPSS (Statistical Package for the Social Sciences) 17.0 software (SPSS, Chicago, IL, USA).
Results
A total of 59 subjects with OH were identified among the 429 eligible participants (mean age 65.1±16.4 years, 77.4% men; Table 1). Subjects with OH had more comorbidities (more heart failure, lower eGFR and lower hemoglobin) and a higher number of prescribed medications (more α-blockers and diuretics) than subjects without OH (Table 1).
Subjects with OH had significantly higher supine SBP, DBP and MAP and significantly lower standing SBP, DBP and MAP when compared with subjects without OH (Table 1). The heart rates were similar between subjects with and without OH in both supine and standing positions, although increases in heart rate after standing were more pronounced in subjects without OH (P=0.034).
Subjects with OH had increased arterial stiffness (significantly higher cf-PWV) and wave reflections (significantly higher cAI, cAP and Pb) and decreased logHF and logLF when compared with subjects without OH (Table 1).
Predictors of OH
Higher supine SBP, DBP, MAP, cf-PWV, cAI, cAP and Pb and lower logLF, logHF, logTP, eGFR and hemoglobin levels significantly correlated with the occurrence of OH (Table 2). In a multivariate logistic regression model with cf-PWV, Pb, logHF, eGFR and hemoglobin as independent variables, Pb and logHF, but not cf-PWV, were significant independent predictors of OH (Table 2). Even after adjusting for the use of α-blockers, diuretics and the presence of heart failure, Pb and logHF but not cf-PWV remained as independent predictors of OH. (Table 2) In addition, Pb was still a significant independent predictor when logHF was replaced with logLF in the model (Supplementary Table S1).
Correlates of orthostatic change of brachial SBP
Supine brachial SBP, DBP, MAP, logHF, logLF, logTP, cf-PWV, cAI, cAP and Pb were significantly correlated with the orthostatic change in brachial SBP (Table 3). In a stepwise linear regression model with Pb, logHF and cf-PWV as independent variables, logHF and Pb, but not cf-PWV, were significant independent correlates of postural change of brachial SBP (Table 3). The correlations of logHF and Pb with SBP changes persisted when the use of diuretics and α-blockers and comorbidities were put into the model (Table 3).
Correlates of HRV
Significant correlates for logHF, logLF and logTP included eGFR, hemoglobin, supine and standing heart rates and cf-PWV (Table 4). In addition, age, standing SBP, DBP and MAP were also significant correlates for logLF. In stepwise regression analyses, cf-PWV remained a significant independent correlate for logHF, logLF and logTP. In contrast, none of the wave reflections indices were a significant correlate for logTP, logHF and logLF (Table 5).
Discussion
The major findings of the present study include: (1) subjects with OH were characterized by high supine BP, increased arterial stiffness, increased wave reflections and decreased HF and LF; (2) increased arterial stiffness contributed to postural SBP change and OH via the modulation of HRV; and (3) increased wave reflections contributed to postural SBP change and OH, independent of arterial stiffness and HRV. These results demonstrate the joint roles of vascular aging and decreased HF and LF in the pathogenesis of OH. Furthermore, increased wave reflections predispose OH independently of arterial stiffness and HRV.
Increased supine wave reflections and OH
A previous study has shown that in 155 communities with residents aging 69±7 years, the supine cAI was significantly higher in 9 subjects with OH than in the 146 subjects without OH (44±12% vs. 30±15%, P=0.012).12 In 10 patients with autonomic failure (61±14 years old), the supine cAI (heart rate adjusted) was also significantly higher than in 14 controls (32.4±13.0% vs. 23.1±8.7%, P=0.05).28 Because cAI is dependent on the reflection transit time and the magnitude of the wave reflections, the observed cAI increase in patients with OH or autonomic failure did not necessarily indicate an increase in the magnitude of the wave reflections. In contrast, Pb is a transit time-independent index of the magnitude of wave reflections.29 The present study clearly demonstrated that the magnitude of wave reflections in the supine position was significantly increased in patients with OH, independent of increases in cf-PWV or the reflection transit time.
The causes for increased wave reflections in subjects with OH remain debatable. An early return of the reflection pressure wave caused by an enhanced arterial stiffness may play a role in causing increased cAI in patients with OH.12 In patients with autonomic failure, relative hypervolemia secondary to daytime renal hypoperfusion, using excessive amounts of salt and the chronic use of fludrocortisone, may be responsible for the increased cAI.28 Alternatively, arterial aging is associated with endothelial dysfunction, and the resulting increased vascular tone in the small arteries may contribute to the increased wave reflection in patients with OH.
The cAI was markedly reduced in subjects with OH (−18±10%) and slightly reduced in subjects without OH (−6±14%, P=0.008) after standing.12 Similarly, cAI was markedly reduced in patients (−100.9±78.1 percentage change) and moderately reduced in the controls (−45.4±55.8 percentage change) after a 60° head-up tilting.28 Both studies demonstrated a strong association between postural changes in cAI and BP.12, 28 Thus, a reduction in cAI after standing appears to be a common observation in subjects with or without OH. Although we did not measure wave reflections after standing, we speculate that substantial decreases in the magnitude of wave reflections must have also occurred concomitantly with a significant decrease in MAP in patients with OH.
Arterial stiffness, wave reflections and BRS
Subjects with OH have a stiffer aorta.17, 30 The cf-PWV was independently associated with OH in a population-based study of 3362 subjects aged ⩾55 years,30 and cf-PWV was shown to be an independent determinant of impaired BRS in a follow-up study.11 Our previous study also demonstrated that both arterial stiffness and wave reflections are independent determinants of orthostatic SBP change.17 Increased arterial stiffness impairs the ‘cushioning’ effects of the arterial tree with subsequently increased volume-sensitive BP variations31 and increased BP variability, both of which may contribute to orthostatic BP fall.32
The present study affirms that arterial stiffness appears to be an independent determinant of decreased HF and LF that may be associated with impaired BRS.1, 15, 16 This outcome is consistent with findings that arterial stiffness correlates with declined sympathetic BRS in elderly men and women.11, 33 This phenomenon is likely because of the fact that the baroreceptors are located in the arterial wall and that their function may become impaired when the mechanical property of the arterial wall changes with age.34
In the present study, we reconfirmed that increased cf-PWV is associated with postural SBP change and the presence of OH. However, the associations were of borderline significance when age, eGFR, hemoglobin, use of diuretics, α-blocker, β-blocker, smoking, diabetes, hypertension and heart failure were accounted for. In our previous study with a larger sample size (total 613 subjects, 100 subjects with OH), cf-PWV and Pb separately were significantly associated with the orthostatic SBP change and were significant predictors of OH in both univariable and multivariable analyses.17
Moreover, we demonstrate for the first time that increased wave reflections may predispose OH independent of arterial stiffness and HRV. The dissociation of arterial stiffness with wave reflections in response to postural change has been recognized.28 In healthy individuals, head-up tilting caused a small decrease in cAI despite an increase in vascular tone and cf-PWV.28 The gravity-related increase in hydrostatic pressure in the lower abdominal aorta with head-up tilting may cause a 20–30% increase in cf-PWV.35 Severe autonomic failure is equivalent to severely reduced BRS. In these patients, head-up tilting caused a 30.4% reduction in systemic vascular resistance, 45.2% fall in aortic SBP, 100.9% reduction in cAI but only a 27.7% reduction in cf-PWV. These data suggest that reduction in systemic vascular resistance due to reduced BRS alone does not fully account for the orthostatic fall in SBP; reduction in wave reflections but not arterial stiffness may independently contribute further to the fall in SBP.
It has been recognized that measuring BP in the sitting (standing) or supine position produces different measurements.36 In the sitting or standing position, the right atrium level is the midpoint of the sternum or the fourth intercostal space.36 In the supine position with the arm resting on the bed, the cuff is below the level of the right atrium.36 In the sitting position with the arm hanging down, the cuff position is even lower than the heart level.36 When the arm position is meticulously adjusted so that the cuff is at the level of the right atrium in both positions, the SBP has been reported to be 8 mm Hg higher in the supine than the upright position.36 We have also measured the vertical distance between the center of the cuff and the sternal angle in both positions in 10 subjects (7 male, average age 55.3±18.8 years, height 165.9±9.7 cm and body mass index 25.2±5.2 kg m−2). The average distance was 8.4±2.8 cm in the supine position and 12.8±3.7 cm in the upright position, with a difference of 4.3±3.6 cm that might add 3.2±2.6 mm Hg to standing BP because of the effect of hydrostatic pressure.36 In the present study, we followed the guidelines for BP measurement36 and the definition of OH.22 Even after correcting for the measured standing BP with the estimated hydrostatic pressure, the population with OH remained unchanged.
Study limitations
We did not measure the changes in heart rate associated with the increase and decrease of BP, or the rate of entry of the sympathetic neurotransmitter, noradrenaline, into the cardiac venous drainage (cardiac noradrenaline spillover). Both methods are considered to be the gold standards for the measurement of cardiovagal and sympathovascular outflows of the BRS, respectively. The baroreceptors are located in the carotid sinus and aortic arch13 that are within the range of the cf-PWV. Moreover, of the 429 participants, direct measurement of the common carotid artery distensibility was available in 57 subjects. Carotid artery distensibility was significantly associated with cf-PWV (r=0.380, P=0.004), logHF (r=0.303, P=0.022), logLF (r=0.327, P=0.013) and logTP (r=0.281, P=0.034). These results may support the link between arterial stiffness and modulation of HRV and BRS. Future studies are needed to reconfirm the relationship between arterial wave reflection and the cardiovagal BRS and to investigate whether increased wave reflections will affect the sympathovascular outflow.
Conclusions
Increased wave reflections may predispose OH independently of arterial stiffness and HRV. In contrast, increased arterial stiffness may cause OH through the modulation of HRV.
References
Monahan KD . Effect of aging on baroreflex function in humans. Am J Physiol Regul Integr Comp Physiol 2007; 293: R3–R12.
Rutan GH, Hermanson B, Bild DE, Kittner SJ, LaBaw F, Tell GS . Orthostatic hypotension in older adults. The Cardiovascular Health Study. CHS Collaborative Research Group. Hypertension 1992; 19: 508–519.
Eigenbrodt ML, Rose KM, Couper DJ, Arnett DK, Smith R, Jones D . Orthostatic hypotension as a risk factor for stroke: the atherosclerosis risk in communities (ARIC) study, 1987–1996. Stroke 2000; 31: 2307–2313.
Yatsuya H, Folsom AR, Alonso A, Gottesman RF, Rose KM, Investigators AS . Postural changes in blood pressure and incidence of ischemic stroke subtypes: the ARIC study. Hypertension 2011; 57: 167–173.
Ooi WL, Hossain M, Lipsitz LA . The association between orthostatic hypotension and recurrent falls in nursing home residents. Am J Med 2000; 108: 106–111.
Gangavati A, Hajjar I, Quach L, Jones RN, Kiely DK, Gagnon P, Lipsitz LA . Hypertension, orthostatic hypotension, and the risk of falls in a community-dwelling elderly population: the maintenance of balance, independent living, intellect, and zest in the elderly of Boston study. J Am Geriatr Soc 2011; 59: 383–389.
Luukinen H, Koski K, Laippala P, Kivelä SL . Prognosis of diastolic and systolic orthostatic hypotension in older persons. Arch Intern Med 1999; 159: 273–280.
Kaess BM, Rong J, Larson MG, Hamburg NM, Vita JA, Levy D, Benjamin EJ, Vasan RS, Mitchell GF . Aortic stiffness, blood pressure progression, and incident hypertension. JAMA 2012; 308: 875–881.
Cheng HM, Wang KL, Chen YH, Lin SJ, Chen LC, Sung SH, Ding PY, Yu WC, Chen JW, Chen CH . Estimation of central systolic blood pressure using an oscillometric blood pressure monitor. Hypertens Res 2010; 33: 592–599.
Chen CH, Nakayama M, Nevo E, Fetics BJ, Maughan WL, Kass DA . Coupled systolic-ventricular and vascular stiffening with age: implications for pressure regulation and cardiac reserve in the elderly. J Am Coll Cardiol 1998; 32: 1221–1227.
Mattace-Raso FU, van den Meiracker AH, Bos WJ, van der Cammen TJ, Westerhof BE, Elias-Smale S, Reneman RS, Hoeks AP, Hofman A, Witteman JC . Arterial stiffness, cardiovagal baroreflex sensitivity and postural blood pressure changes in older adults: the Rotterdam Study. J Hypertens 2007; 25: 1421–1426.
Tabara Y, Nakura J, Kondo I, Miki T, Kohara K . Orthostatic systolic hypotension and the reflection pressure wave. Hypertens Res 2005; 28: 537–543.
Chen CH, Hu HH, Lin YP, Chern CM, Hsu TL, Ding PY . Increased arterial wave reflection may predispose syncopal attacks. Clin Cardiol 2000; 23: 825–830.
Task Force of the European Society of Cardiology and North American Society. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation 1996; 93: 1043–1065.
Goldstein DS, Bentho O, Park MY, Sharabi Y . Low-frequency power of heart rate variability is not a measure of cardiac sympathetic tone but may be a measure of modulation of cardiac autonomic outflows by baroreflexes. Exp Physiol 2011; 96: 1255–1261.
Rahman F, Pechnik S, Gross D, Sewell L, Goldstein DS . Low frequency power of heart rate variability reflects baroreflex function, not cardiac sympathetic innervation. Clin Auton Res 2011; 21: 133–141.
Sung SH, Chen ZY, Tseng TW, Lu DY, Yu WC, Cheng HM, Chen CH . Wave reflections, arterial stiffness, and orthostatic hypotension. Am J Hypertens, (e-pub ahead of print 9 May 2014; doi:10.1093/ajh/hpu063).
Sung SH, Yu WC, Cheng HM, Chuang SY, Wang KL, Huang CM, Chen CH . Pulsatile hemodynamics and clinical outcomes in acute heart failure. Am J Hypertens 2011; 24: 775–782.
Ma YC, Zuo L, Chen JH, Luo Q, Yu XQ, Li Y, Xu JS, Huang SM, Wang LN, Huang W, Wang M, Xu GV, Wang HY . Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol 2006; 17: 2937–2944.
Sung SH, Chuang SY, Sheu WH, Lee WJ, Chou P, Chen CH . Relation of adiponectin and high-sensitivity C-reactive protein to pulse-wave velocity and N-terminal pro-B-type natriuretic peptide in the general population. Am J Cardiol 2009; 103: 1411–1416.
Cortez-Cooper MY, Supak JA, Tanaka H . A new device for automatic measurements of arterial stiffness and ankle-brachial index. Am J Cardiol 2003; 91: 1519–1522.
The Consensus Committee of the American Autonomic Society and the American Academy of Neurology. Consensus statement on the definition of orthostatic hypotension, pure autonomic failure, and multiple system atrophy. J Neurol Sci 1996; 144: 218–219.
Yu WC, Chuang SY, Lin YP, Chen CH . Brachial-ankle vs. carotid-femoral pulse wave velocity as a determinant of cardiovascular structure and function. J Hum Hypertens 2008; 22: 24–31.
Takazawa K, Tanaka N, Takeda K, Kurosu F, Ibukiyama C . Underestimation of vasodilator effects of nitroglycerin by upper limb blood pressure. Hypertension 1995; 26: 520–523.
Wang KL, Cheng HM, Sung SH, Chuang SY, Li CH, Spurgeon HA, Ting CT, Najjar SS, Lakatta EG, Yin FC, Chou P, Chen CH . Wave reflection and arterial stiffness in the prediction of 15-year all-cause and cardiovascular mortalities: a community-based study. Hypertension 2010; 55: 799–805.
Westerhof BE, Guelen I, Westerhof N, Karemaker JM, Avolio A . Quantification of wave reflection in the human aorta from pressure alone: a proof of principle. Hypertension 2006; 48: 595–601.
Berger RD, Akselrod S, Gordon D, Cohen RJ . An efficient algorithm for spectral analysis of heart rate variability. IEEE Trans Biomed Eng 1986; 33: 900–904.
Huijben AM, Mattace-Raso FU, Deinum J, Lenders J, van den Meiracker AH . Aortic augmentation index and pulse wave velocity in response to head-up tilting: effect of autonomic failure. J Hypertens 2012; 30: 307–314.
Liao CF, Cheng HM, Sung SH, Yu WC, Chen CH . Determinants of pressure wave reflection: characterization by the transit-time independent reflected wave amplitude. J Hum Hypertens 2011; 25: 665–671.
Mattace-Raso FU, van der Cammen TJ, Knetsch AM, van den Meiracker AH, Schalekamp MA, Hofman A, Witteman JC . Arterial stiffness as the candidate underlying mechanism for postural blood pressure changes and orthostatic hypotension in older adults: the Rotterdam Study. J Hypertens 2006; 24: 339–344.
Chen CH, Nakayama M, Nevo E, Fetics BJ, Kass DA . Age-related ventricular-vascular stiffening: effects on preload sensitivity. Circulation 1997; 96: I–199.
Schillaci G, Bilo G, Pucci G, Laurent S, Macquin-Mavier I, Boutouyrie P, Battista F, Settimi L, Desamericq G, Dolbequ G, Faini A, Salvi P, Mannarino E, Parati G . Relationship between short-term blood pressure variability and large-artery stiffness in human hypertension: findings from 2 large databases. Hypertension 2012; 60: 369–377.
Okada Y, Galbreath MM, Shibata S, Jarvis SS, VanGundy TB, Meier RL, Vongpatanasin W, Levine BD, Fu Q . Relationship between sympathetic baroreflex sensitivity and arterial stiffness in elderly men and women. Hypertension 2012; 59: 98–104.
Shimada K, Kitazumi T, Sadakane N, Ogura H, Ozawa T . Age-related changes of baroreflex function, plasma norepinephrine, and blood pressure. standards of measurement. Hypertension 1985; 7: 113–117.
Avolio A, Butlin M, Xu K . Reflections on determinants of augmentation index. J Hypertens 2012; 30: 267–268.
Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ . Recommendations for blood pressure measurement in humans and experimental animals: Part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension 2005; 45: 142–161.
Acknowledgements
This work was supported by National Science Council (NSC 102-2314-B-010 -052 -), and an intramural grant from the Taipei Veterans General Hospital (Grant No. 2013-09-011AC).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Lu, DY., Sung, SH., Yu, WC. et al. Wave reflections, arterial stiffness, heart rate variability and orthostatic hypotension. Hypertens Res 37, 1056–1061 (2014). https://doi.org/10.1038/hr.2014.127
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2014.127
Keywords
This article is cited by
-
Effect of Different Classes of Antihypertensive Drugs on Arterial Stiffness
Current Hypertension Reports (2023)
-
Diagnostic criteria for initial orthostatic hypotension: a narrative review
Clinical Autonomic Research (2021)
-
Serum long-chain omega-3 polyunsaturated fatty acids and risk of orthostatic hypotension
Hypertension Research (2016)
-
The measurement of orthostatic blood pressure as a screening tool for masked hypertension with abnormal circadian blood pressure rhythm
Hypertension Research (2016)