Abstract
Recent studies suggested that home arterial stiffness index (HASI) may be a new measure of arterial stiffness. The aim of this study was to investigate whether HASI is more strongly associated with arterial stiffness than is pulse pressure (PP) and thus a more suitable tool than PP for evaluating arterial stiffness in patients with type 2 diabetes. We evaluated the relationship of HASI or PP with pulse wave velocity (PWV) as well as with major cardiovascular risk factors in 332 patients with type 2 diabetes. Furthermore, we compared the area under the receiver-operator characteristic curve (AUC) of HASI or PP for PWV. Morning PP was positively associated with PWV (r=0.303, P<0.0001), while morning HASI was not (r=−0.006, P=0.9063). Multiple regression analysis demonstrated that morning PP (β=0.179, P=0.0210), but not morning HASI (β=−0.040, P=0.5036), was independently associated with PWV. The AUCs (95% confidence interval (CI)) of morning HASI and morning PP for arterial stiffness were 0.510 (0.448–0.573) (P=0.745) and 0.638 (0.578–0.698) (P<0.0001), respectively. The AUC (95% CI) of morning HASI for arterial stiffness was significantly less than that of morning PP (P=0.0005). In conclusion, morning HASI is less correlated with PWV than is morning PP in patients with type 2 diabetes.
Similar content being viewed by others
Introduction
Recently, the ambulatory arterial stiffness index (AASI), which is derived from the linear relationship between 24-h ambulatory systolic and diastolic blood pressure measurements, has been proposed as an easy measure of arterial stiffness.1 Furthermore, previous studies have demonstrated that AASI is associated with target organ damage, such as stroke and cardiovascular disease.2 Although AASI has been validated, ambulatory blood pressure monitoring is uncommonly used in routine clinical practice. Home blood pressure has been found to have a stronger relationship with target organ damage than clinic blood pressure in several population-based studies and prospective clinical studies.3, 4 As home blood pressure monitoring is less costly, more widely available and better accepted by patients than ambulatory blood pressure monitoring, the application of the home arterial stiffness index (HASI) would have considerable potential for wide use in clinical practice if HASI could be a useful marker for arterial stiffness.
Qureshi et al.5 have demonstrated that HASI is significantly correlated with pulse wave velocity (PWV) and left ventricular mass index. Xu et al.6 reported that the AASI, but not the HASI, is associated with PWV. Thus, HASI has prompted considerable controversy and debate as to whether it is a true measure of arterial stiffness.
Pulse pressure (PP) increases concomitantly with arterial stiffness because the stiffer the aorta is, the faster the reflected pressure wave returns to the heart and superimposes in the forward wave during late systole.7 PP has been reported to be linked to micro- and macrovascular complications and arterial stiffness.8
Arterial stiffness can be assessed simply, noninvasively and reproducibly by measuring PWV along the thoracoabdominal aorta.9 PWV is a marker for both severity of vascular damage and prognosis in atherosclerotic vascular disease.10 However, the classic methods to evaluate arterial stiffness require special expensive equipment and trained observer.
There has been no study investigating the association between HASI and arterial stiffness in patients with type 2 diabetes. We hypothesized that if HASI were a useful marker for arterial stiffness, it would have considerable potential for wide use in clinical practice. The aim of this study was to investigate whether HASI is more strongly associated with arterial stiffness evaluated by PWV and thus would be a more suitable tool than PP for evaluating arterial stiffness in patients with type 2 diabetes.
Methods
Patients
Home blood pressure measurements were performed in patients with type 2 diabetes who had regularly attended the diabetes outpatient clinic at the Hospital of Kyoto Prefectural University of Medicine, Kyoto, Japan and the other four general hospitals as previously reported.11 A total of 954 type 2 diabetic patients agreed to participate in the present study. First, 31 patients who conducted home blood pressure measurement for <4 consecutive days12 were excluded. We randomly measured PWV and 567 patients, whose PWV data were not available, were also excluded. In addition, 10 patients who had advanced renal dysfunction (serum creatinine ⩾2.0 mg dl−1) and 14 patients whose ankle-brachial index <0.9513 were excluded from the analyses. Finally, 332 patients comprised the study population (175 male, 157 female). Type 2 diabetes was diagnosed according to the Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus.14 Retinopathy was assessed with a state of mydriasis by ophthalmologists who were unaware of the data, and was graded as follows: no diabetic retinopathy; simple diabetic retinopathy; and proliferative, including preproliferative, diabetic retinopathy. If the finding in the left and right fundi were discordant, the worse side was taken as a representative for the subject. Nephropathy was graded as follows: normoalbuminuria, urinary albumin excretion <30 mg per gram of creatinine (mg g−1 Cr); microalbuminuria, 30–300 mg g−1 Cr; or macroalbuminuria, >300 mg g−1 Cr. Neuropathy was defined by the diagnostic criteria for diabetic neuropathy proposed by the Diagnostic Neuropathy Study Group.15 In brief, in the absence of peripheral neuropathies, diabetic neuropathy is diagnosed by ⩾2 of the following: neuropathic symptoms such as numbness, paresthesia and neuropathic pain, decreased or absent ankle reflex (bilateral), and decreased distal sensation. Cardiovascular disease was defined as a previous myocardial or cerebral infarction based on the clinical history or physical examination. Subjects were classified as nonsmokers, past smokers or current smokers according to a self-administered questionnaire.
Study design
We designed a cross-sectional multicenter study in general hospitals, which are located in Kansai area in Japan. First, we evaluated relationships of HASI or PP to PWV as well as to major cardiovascular risk factors, including age, serum lipid concentration and hemoglobin A1c, using a linear regression analysis. Second, we performed multiple regression analysis to determine the contribution of the variables on PWV. Finally, we compared area under the receiver-operator characteristic curve (AUC) of HASI or PP for arterial stiffness defined as PWV ⩾1800 cm s−1. This study was approved by the local Research Ethics Committee and was conducted in accordance with Declaration of Helsinki, and informed consent was obtained from all the participants.
Data collection
Blood samples for biochemical measurements were taken at the hospital. Serum total cholesterol, triglycerides and high-density lipoprotein cholesterol concentrations were assessed using standard enzymatic methods. HemoglobinA1c was assayed using high-performance liquid chromatography with the standard provided by the National Glycohemoglobin Standardization Program. Urinary albumin excretion was measured with an immunoturbidimetric assay. A mean value for urinary albumin excretion was determined from three urine collections. Home blood pressure measurements were self-measured using an automatic memory-equipped device, (HEM-70801C; Omron Healthcare, Kyoto, Japan), which uses the cuff-oscillometric method to generate a digital display of heart rate and systolic/diastolic blood pressure value. HEM-70801C uses the identical components and blood pressure determining algorithm to those of another device, HEM-705IT, which was previously validated and satisfied the criteria of the British Hypertension Society protocol.16 Patients received written instructions and individual guidance on how to self-measure triplicate morning and evening home blood pressure measurements for 14 consecutive days. Measurements of morning home blood pressure were made within 1 h of waking, before breakfast or taking any drugs, with the patient seated and rested for at least 5 min.17 Measurements of evening home blood pressure were obtained in a homologous way just before going to bed.
Measurement of PVW
Brachial-ankle PWV was measured using a Colin Waveform Analyzer (form PWV/ankle-brachial index/toe brachial index; Colin Medical Technology, Komaki, Japan), which simultaneously measures pulse volumes in the brachial and posterior tibial or toe arteries using an oscillometric method together with bilateral arm and ankle or toe blood pressure. PWV was measured after allowing the patient to rest in the supine position for at least 5 min. Details of the method have been described elsewhere.18 After bilateral determination of brachial-ankle PWV, the higher value was taken as a representative for each subject.
HASI estimation
The regression slope of diastolic on systolic blood pressure was computed for each individual on the basis of home blood pressure readings. HASI was defined as one minus the respective regression slope.1
Statistical analysis
Means and frequencies of potential confounding variables were calculated. The relationships between HASI or PP and PWV, age, glycemic control or other variables were examined by Pearson’s correlation analyses, using Stat View software (version 5.0; SAS Institute, Cary, NC, USA). In multiple regression analysis to assess the effects of variables on PWV, we included the following independent variables: age, gender, duration of diabetes, body mass index, mean arterial pressure, hemoglobin A1c, total cholesterol, triglycerides, smoking, alcohol and HASI or PP. Receiver-operator characteristic analyses were performed to calculate AUC of HASI or PP for arterial stiffness defined as PWV ⩾1800 cm s−1, using the ROCKIT (http://xray.bsd.uchicago.edu/krl/roc_soft.htm). All continuous variables are presented as the mean±s.d. A P value <0.05 was considered statistically significant.
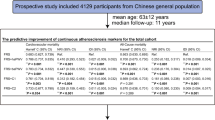
Results
The clinical characteristics of patients with type 2 diabetes are shown in Table 1. The average number of morning and evening home systolic blood pressure measurements per patient during the 14-day study period was 39.3±6.4 and 37.3±8.0, respectively. The relationships between HASI or PP and the characteristics of patients with type 2 diabetes are shown in Table 2. Age was positively associated with morning HASI, and age, duration of diabetes and PWV were positively associated with morning PP. Duration of diabetes and PWV were positively associated with evening HASI, and age, duration of diabetes and PWV were positively associated with evening PP. Age (r=0.141, P=0.0113) and PWV (r=0.113, P=0.0404) were positively associated with HASI in the morning and evening, and age (r=0.351, P<0.0001), duration of diabetes (r=0.216, P<0.0001) and PWV (r=0.319, P<0.0001) were positively associated with PP in the morning and evening. Morning HASI correlated significantly with morning PP (r=0.271, P<0.0001), and evening HASI correlated significantly with evening PP (r=0.289, P<0.0001). HASI in the morning and evening correlated significantly with PP in the morning and evening (r=0.314, P<0.0001). Multiple regression analysis demonstrated that age (β=0.216, P=0.0012), gender (β=-0.169, P=0.0245) and mean arterial pressure (β=0.209, P=0.0012), but not morning HASI (β=−0.040, P=0.5036), were independently associated with PWV, and age (β=0.154, P=0.0273) and morning PP (β=0.179, P=0.0210) were independently associated with PWV (Table 3). Age (β=0.219, P=0.0008), body mass index (β=−0.130, P=0.0382), alcohol (β=0.160, P=0.0137), mean arterial pressure (β=0.208, P=0.0007) and evening HASI (β=0.166, P=0.0058) were independently associated with PWV, and age (β=0.178, P=0.0094), alcohol (β=0.152, P=0.0188) and evening PP (β=0.182, P=0.0114) were independently associated with PWV (Table 3). Age (β=0.213, P=0.0012), alcohol (β=0.132, P=0.0434) and mean arterial pressure (β=0.228, P=0.0002), but not HASI in the morning and evening (β=0.085, P=0.1573), were independently associated with PWV, and age (β=0.165, P=0.0166), alcohol (β=0.131, P=0.0431), mean arterial pressure (β=0.151, P=0.0309) and PP in the morning and evening (β=0.183, P=0.0131) were independently associated with PWV. AUC (95% confidence interval (CI)) of morning HASI and morning PP for arterial stiffness were 0.510 (0.448–0.573) (P=0.745) and 0.638 (0.578–0.698) (P<0.0001), respectively. AUC (95% CI) of morning HASI for arterial stiffness was significantly less than that of morning PP (P=0.0005; Figure 1a). AUC (95% CI) of evening HASI and evening PP for arterial stiffness were 0.600 (0.539–0.661) (P=0.002) and 0.638 (0.578–0.698) (P<0.0001), respectively. AUC (95% CI) of evening HASI for arterial stiffness did not differ from that of evening PP (P=0.0757; Figure 1b). The AUCs (95% CI) of HASI in the morning and evening and of PP in the morning and evening for arterial stiffness were 0.568 (0.506–0.629) (P=0.033) and 0.643 (0.583–0.703) (P<0.0001), respectively. The AUC (95% CI) of HASI in the morning and evening for arterial stiffness was significantly less than that of PP in the morning and evening (P=0.0397).
(a) Area under the receiver-operator characteristic curve (AUC) of morning home arterial stiffness index (HASI) and pulse pressure (PP) for arterial stiffness defined as pulse wave velocity ⩾1800 cm s−1. We compared AUC (95% confidence interval (CI)) between the two groups using the ROCKIT. Value of P was as follows: HASI vs. PP, P=0.0005. (b) AUC of evening HASI and PP for arterial stiffness defined as pulse wave velocity ⩾1800 cm s−1. We compared AUC (95% CI) between the two groups using the ROCKIT. Value of P was as follows: HASI vs. PP, P=0.0757.
Discussion
The present study demonstrated that the AUC of morning HASI for arterial stiffness was significantly less than that of morning PP, suggesting that the recently proposed HASI is a less useful marker for arterial stiffness than is PP in patients with type 2 diabetes. To our knowledge, this is the first report to investigate whether HASI is more strongly associated with PWV and whether it would thus be a more suitable tool than PP for evaluating arterial stiffness in patients with type 2 diabetes.
Schillaci et al.19 suggested that a narrow range of diastolic blood pressure values throughout the 24-h period results in higher AASI values. This is because a narrow range of diastolic blood pressure values flattens the regression line of diastolic on systolic blood pressure. In the same line, for a given range of diastolic blood pressure values, the wider the range of systolic blood pressure values, the flatter the regression line and thereby the higher the AASI value.
PP increases concomitantly with arterial stiffness because the stiffer the aorta is, the faster the reflected pressure wave returns to the heart and superimposes in the forward wave during late systole.7 The exact pathophysiological meaning of AASI in terms of arterial regulation has not been established. Recently, it was suggested that AASI may be a measure of ventriculo-arterial coupling because it depends on arterial factors and on cardiac factors.20 Even though many authors consider both PP and AASI as surrogates of arterial stiffness, these parameters may have different physiological meanings from the arterial stiffness, such as PWV. This study indicates that morning PP is a better marker for arterial stiffness than is morning HASI, which has been proposed as a new marker for arterial stiffness.
Qureshi et al.5 have demonstrated that HASI was significantly correlated with aortic PWV and left ventricular mass index. Matsui et al.21 demonstrated that HASI was significantly correlated with carotid atherosclerosis even after adjusting for confounders. On the other hand, Stergiou et al.22 have reported that HASI did not have strength of association to replace AASI for assessing arterial stiffness because HASI was correlated less with age and PP than AASI was. Xu et al.6 reported that the AASI, but not the HASI, is associated with aortic PWV.
HASI is based on blood pressure measurements taken under stabilized conditions. Therefore, this index provides only limited information about the dynamic relationship between systolic blood pressure and diastolic blood pressure. By contrast, AASI is based on measurements taken in ambulatory conditions while patients undertake their usual daily activities. The reason why the AUC of morning HASI for arterial stiffness was significantly less than that of morning PP while the AUC of evening HASI for arterial stiffness did not differ from that of evening PP has not been clearly determined by this study. The AUC of morning HASI for arterial stiffness was significantly less than that of the AUCs of morning PP, evening HASI and evening PP (data not shown). In addition, the reason why drinking alcohol was independently associated with PWV in multiple regression analysis is not clear. The mean PWV in non-drinkers, social drinkers and everyday drinkers was 1833±330, 1864±374 and 1872±346 cm s−1, respectively (P=0.6710). In general, light-to-moderate alcohol intake has been reported to be vasculoprotective;23 however, in a study by Matsumoto et al.,24 light-to-moderate alcohol intake appeared to have a possible vasculoprotective effect in subjects with optimal or normal blood pressure, but the U-shaped relationship was not observed, and heavy alcohol intake seemed to exert a detrimental effect on the vasculature in subjects with high normal blood pressure or high blood pressure. Most of the patients in the present study had a high normal blood pressure or high blood pressure.
Kikuya et al.25 reported that HASI predicted cerebral infarction independent of PP and other risk factors in normotensive subjects. Therefore, we evaluated the relationship between HASI and PWV in normotensive patients. Morning HASI was not significantly associated with PWV (r=0.083, P=0.5576), and evening HASI was not also significantly associated with PWV (r=0.163, P=0.2442). Unfortunately, however, the number of normotensive patients was too small (n=53) to adequately evaluate the relationship between HASI and PWV in normotensive patients in this study.
This study has some limitations that require consideration. First, the relatively small number of patients may not be sufficient to conclude that morning HASI is a less suitable tool for evaluating arterial stiffness than is morning PP in patients with type 2 diabetes. Second, it might therefore be argued that HASI, as estimated in this study, provides only limited information about the dynamic relationship of systolic with diastolic blood pressure because HASI is exclusively derived from morning and evening blood pressure measurements, each time measured in triplicate but within a short time interval. Third, for comparing the AUC of HASI or PP for arterial stiffness, we defined arterial stiffness as PWV ⩾1800 cm s−1, which is an arbitrary level, because the median value of PWV in this study was 1828 cm s−1. If we had defined arterial stiffness as PWV ⩾1600 or ⩾2000 cm s−1, the main findings would have been almost identical (data not shown). Finally, the reproducibility of HASI has not been clarified.
Conclusions
The AUC of morning HASI for arterial stiffness was significantly less than that of morning PP, suggesting that the recently proposed HASI is a less useful marker for arterial stiffness than is PP in patients with type 2 diabetes. Morning HASI could not be regarded as a reliable substitute for morning PP as a marker for arterial stiffness.
References
Dolan E, Li Y, Thijs L, McCormack P, Staessen JA, O'Brien E, Stanton A . Ambulatory arterial stiffness index: rationale and methodology. Blood Press Monit 2006; 11: 103–105.
Dolan E, Thijs L, Li Y, Atkins N, McCormack P, McClory S, O'Brien E, Staessen JA, Stanton AV . Ambulatory arterial stiffness index as a predictor of cardiovascular mortality in the Dublin Outcome Study. Hypertension 2006; 47: 365–370.
Ohkubo T, Imai Y, Tsuji I, Nagai K, Kato J, Kikuchi N, Nishiyama A, Aihara A, Sekino M, Kikuya M, Ito S, Satoh H, Hisamichi S . Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in Ohasama, Japan. J Hypertens 1998; 16: 971–975.
Sega R, Trocino G, Lanzarotti A, Carugo S, Cesana G, Schiavina R, Valagussa F, Bombelli M, Giannattasio C, Zanchetti A, Mancia G . Alterations of cardiac structure in patients with isolated office, ambulatory, or home hypertension: data from the general population (Pressione Arteriose Monitorate E Loro Associazioni [PAMELA] Study). Circulation 2001; 104: 1385–1392.
Qureshi G, Lazar JM, Javaid H, Weber M, Salciccioli L . Self-measured (blood pressure) arterial stiffness index: a promising new measure of arterial stiffness. J Am Soc Hypertens 2007; 1: 347–352.
Xu TY, Li Y, Fan WX, Li FH, Zou J, Gao PJ, Staessen JA, Wang JG . Ambulatory (AASI), but not home (HASI), arterial stiffness index is associated with aortic pulse wave velocity. Hypertens Res 2011; 34: 402–403.
Safar ME, Levy BI, Struijker-Boudier H . Current perspectives on arterial stiffness and pulse pressure in hypertension and cardiovascular diseases. Circulation 2003; 107: 2864–2869.
Knudsen ST, Poulsen PL, Hansen KW, Ebbehøj E, Bek T, Mogensen CE . Pulse pressure and diurnal blood pressure variation: association with micro- and macrovascular complications in type 2 diabetes. Am J Hypertens 2002; 15: 244–250.
Asmar R, Benetos A, Topouchian J, Laurent P, Pannier B, Brisac AM, Target R, Levy BI . Assessment of arterial distensibility by automatic pulse wave velocity measurement: validation and clinical application studies. Hypertension 1995; 26: 485–490.
Yamashina A, Tomiyama H, Arai T, Hirose K, Koji Y, Hirayama Y, Yamamoto Y, Hori S . Brachial-ankle pulse wave velocity as a marker of atherosclerosis vascular damage and cardiovascular risk. Hypertens Res 2003; 26: 615–622.
Ushigome E, Fukui M, Sakabe K, Tanaka M, Inada S, Omoto A, Tanaka T, Fukuda W, Atsuta H, Ohnishi M, Mogami S, Kitagawa Y, Oda Y, Yamazaki M, Hasegawa G, Nakamura N . Uncontrolled home blood pressure in the morning is associated with nephropathy in Japanese type 2 diabetes. Heart Vessels 2011; 26: 609–615.
Johansson JK, Niiranen TJ, Puukka PJ, Jula AM . Optimal schedule for home blood pressure monitoring based on a clinical approach. J Hypertens 2010; 28: 259–264.
Motobe K, Tomiyama H, Koji Y, Yambe M, Gulinisa Z, Arai T, Ichihashi H, Nagae T, Ishimaru S, Yamashina A . Cut-off value of the ankle-brachial pressure index at which the accuracy of brachial-ankle pulse wave velocity measurement is diminished. Circ J 2005; 69: 55–60.
The Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 2002; 25: S5–20.
Yasuda H, Sanada M, Kitada K, Terashima T, Kim H, Sakaue Y, Fujitani M, Kawai H, Maeda K, kashiwagi A . Rationale and usefulness of newly devised abbreviated diagnostic criteria and staging for diabetic polyneuropathy. Diabetes Res Clin Pract 2007; 77S: S178–S183.
Coleman A, Freeman P, Steel S, Shennan A . Validation of the Omron 705IT (HEM-759-E) oscillometric blood pressure monitoring device according to the British Hypertension Society protocol. Blood Press Monit 2006; 11: 27–32.
Imai Y, Otsuka K, Kawano Y, Shimada K, Hayashi H, Tochikubo O, Miyakawa M, Fukiyama K . Japanese Society of Hypertension. Japanese Society of Hypertension (JSH) guidelines for self-monitoring of blood pressure at home. Hypertens Res 2003; 26: 771–782.
Yamashina A, Tomiyama H, Takeda K, Tsuda H, Arai T, Hirose K, Koji Y, Hori S, Yamamoto Y . Validity, reproducibility, and clinical significance of noninvasive brachial-ankle pulse wave velocity measurement. Hypertens Res 2002; 25: 359–364.
Schillaci G, Parati G, Pirro M, Pucci G, Mannarino MR, Sperandini L, Mannarino E . Ambulatory arterial stiffness index is not a specific marker of reduced arterial compliance. Hypertension 2007; 49: 986–991.
Westerhof N, Lankhaar JW, Westerhof BE . Ambulatory arterial stiffness index is not a stiffness parameter but a ventriculo-arterial coupling factor. Hypertension 2007; 49: e7.
Matsui Y, Ishikawa J, Shibasaki S, Shimada K, Kario K . Association between home arterial stiffness index and target organ damage in hypertension: comparison with pulse wave velocity and augmentation index. Atherosclerosis 2011; 219: 637–642.
Stergiou GS, Kollias A, Rarra VC, Nasothimiou EG, Roussias LG . Arterial stiffness index based on home (HASI) vs. ambulatory (AASI) blood pressure measurements. Hypertens Res 2010; 33: 731–736.
Wakabayashi I, Kobaba-Wakabayashi R, Masuda H . Relation of drinking alcohol to atherosclerotic risk in type 2 diabetes. Diabetes Care 2002; 25: 1223–1228.
Matsumoto C, Tomiyama H, Yamada J, Yoshida M, Shiina K, Nagata M, Yamashina A . Association of blood pressure levels with the effects of alcohol intake on the vasculature in Japanese men. Hypertens Res 2009; 32: 127–132.
Kikuya M, Ohkubo T, Satoh M, Hashimoto T, Hirose T, Metoki H, Obara T, Inoue R, Asayama K, Hoshi H, Totsune K, Satoh H, Staessen JA, Imai Y . Prognostic significance of home arterial stiffness index derived from self-measurement of blood pressure: the Ohasama Study. Am J Hypertens 2012; 25: 67–73.
Acknowledgements
We thank Naoko Higo, Machiko Hasegawa and Terumi Kaneko in Kyoto Prefectural University of Medicine, Kyoto, Japan for teaching patients how to measure their blood pressure; Sayoko Horibe, Hiroko Kawamura and Sanae Utena in Kyoto Prefectural University of Medicine, Kyoto, Japan for their secretarial assistance.
Author contributions
MF researched date and wrote the manuscript; EU, MT and GH researched date and contributed to discussion; MH contributed to discussion, TT, HA, MO and YO researched date; and NN researched date and reviewed/edited the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Fukui, M., Ushigome, E., Tanaka, M. et al. Could home arterial stiffness index be a novel marker for arterial stiffness in patients with type 2 diabetes?. Hypertens Res 36, 645–649 (2013). https://doi.org/10.1038/hr.2013.4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2013.4