Abstract
This study was designed to evaluate the possible renoprotective effects of rosiglitazone (RGT), a peroxisome proliferator-activated subtype γ receptor agonist, in deoxycorticosterone acetate (DOCA)-salt hypertension and its role in endogenous endothelin-1 (ET-1) production and renal fibrosis associated with inflammation. Rats were implanted with DOCA strips (200 mg kg−1) at 1 week after unilateral nephrectomy. DOCA-salt rats received control diet with or without RGT (10 mg kg−1 per day). Systolic blood pressure was measured by the tail-cuff method. Glomerulosclerosis and tubulointerstitial fibrosis were evaluated on kidney sections. The expression of ED-1, cyclooxygenase-2 (COX-2), heat shock protein-25 (HSP25) and transforming growth factor-β1 (TGF-β1) was determined in the kidney by semiquantitative immunoblotting. In DOCA-salt rats, systolic blood pressure was increased, whereas creatinine clearance decreased compared with controls, which were counteracted by RGT treatment. Tubular injury and glomerulosclerois in the histological study were prominent in DOCA-salt rats, which were counteracted by RGT treatment. ET-1 expression was increased in DOCA-salts rats, which was attenuated by RGT treatment. The expression of TGF-β1, ED-1 and COX-2 was increased in DOCA-salt, which was attenuated by RGT treatment. In conclusion, RGT treatment decreases blood pressure and is effective in preventing the progression of renal injury in DOCA-salt hypertension, the mechanisms of which are associated with anti-inflammatory and anti-fibrotic effects through reducing the overexpression of ET-1, ED-1, COX-2 and TGF-β1 in the kidney.
Similar content being viewed by others
Introduction
Thiazolidinediones (TZDs) are used to treat type II diabetes because of their efficacy in controlling blood glucose secondary to enhancing insulin action through a mechanism(s) that is yet to be completely elucidated.1 Interestingly, these compounds are also capable of a rich array of beneficial effects, including reductions of blood pressure in animal models and humans.2, 3, 4 Moreover, TZDs prevent vascular smooth muscle cell growth5 and inflammatory response.6 One of the TZDs, rosiglitazone (RGT) also has diverse actions. It has anti-inflammatory and anti-fibrotic effects in nondiabetic renal disease,7 and an anti-hypertensive effect.8
Deoxycorticosterone acetate (DOCA)-salt hypertensive rat is a well known, established model of mineralocorticoid hypertension with renal dysfunction. Although mineralocorticoid is traditionally known to promote sodium retention, recent evidence indicates that it causes oxidative stress,9 and stimulates inflammation and fibrosis by activating transcription factors such as nuclear factor κ-B (NF-κB) and activating protein-1.10 Glomerular and tubular damage such as focal and segmental glomerular sclerosis, mesangial expansion, inflammatory cell infiltration and tubulointerstitial fibrosis develops in this model of hypertension together with activation of renal endothelin-1 (ET-1) and transforming growth factor (TGF)-β1 expression.11, 12, 13 The PPARγ activators significantly attenuated renal damage in a rat model of diabetic nephropathy associated with reduced oxidative stress and TGF-β1 expression.14 Moreover, it provided far better renal protection compared with suppression of the renin-angiotensin system by ACE inhibitors, and is able to suppress ET-1 secretion from endothelial and vascular smooth muscle cells.15 These findings suggest the ability of protective effects of PPARγ activators against hypertensive renal injury. In the kidney, PPARγ protein is widely expressed along the nephron segment,16 but its role in hypertensive renal injury has not yet been determined.
This study was aimed at characterizing the renal protective effects of RGT in DOCA-salt hypertension and in the progression of inflammation and fibrosis in the kidney. We evaluated the effects of RGT on blood pressure, renal injury and ET-1 production in DOCA-salt hypertensive rats.
Methods
Animals
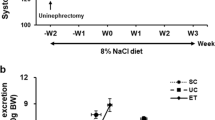
The animal study was approved by the Ethics Committee of Chonnam National University Medical School. Male Sprague-Dawley rats weighing 180–200 g were used. DOCA-salt hypertension was induced by subcutaneous implantation of silicone rubber containing DOCA (200 mg kg−1) at 1 week after unilateral nephrectomy. Physiologic saline was supplied as drinking water to all animals. Two weeks after DOCA implantation, DOCA-salt rats were randomly divided to receive control diet with or without RGT (avandia, 10 mg kg−1 per day) for another 2 weeks. Systolic blood pressure was measured by the tail-cuff method (Power lab, ADInstruments Inc., Colorado Springs, CO, USA) at 2 and 4 weeks after DOCA implantation. The rats were maintained individually in metabolic cages to allow urine collections for the measurement of Na+, K+ and creatinine. They were killed for semiquantitative immunoblotting and immunohistochemical studies at 4 weeks after DOCA implantation. Under anesthesia with isoflurane, blood samples were collected from the inferior vena cava and analyzed for Na+, K+ and creatinine. The kidney was rapidly removed from the dissected cortex and outer stripe of the outer medulla (cortex/OSOM), and processed for immunoblotting as described below.
Another series of experiments was performed for the assay of real-time polymerase chain reaction (PCR). The rats were decapitated in a conscious state, and their kidneys were taken and kept at −70 °C until assayed for the mRNA expression by real-time PCR.
Another set of experiments was made to examine the effects of RGT alone in unilateral nephrectomized rats, with no DOCA implanted. Three weeks later after unilateral nephrectomy, rats received control diet with or without RGT (avandia, 10 mg kg−1 per day) for another 2 weeks. The kidneys were taken for immunoblotting of ED-1, TGF-β1, Na+/H+ exchanger type 3 (NHE3) and Na,K ATPase α1.
Histology
A perfusion needle was inserted into the abdominal aorta and the vena cava was cut to establish an outlet. Blood was flushed from the kidney with cold phosphate-buffered saline (pH 7.4) for 15 s before switching to cold 3% paraformaldehyde in 0.1 M cacodylate buffer (pH 7.4) for 3 min. The kidney was removed and sectioned into 2–3 mm transverse sections and immersion fixed for an additional 1 h, followed by 3 × 10 min washes with 0.1 M cacodylate buffer of pH 7.4. The tissue was dehydrated in graded ethanol and left overnight in xylene. After embedding in paraffin, 2 μm sections were made on a rotary microtome (Leica Microsystems A/S, Herlev, Denmark). The Periodic acid Schiff (PAS) stain and Masson trichrome (M-T) were performed. Microscopy was carried out using a light microscope (Nikon, Tokyo, Japan).
Pathologic examinations
The extent of glomerulosclerosis (GS) was graded from 0 to 4 by a semiquantitative score: 0, normal; 1, mesangial expansion/sclerosis involving <25% of the tuft; 2, moderate GS (25–50%); 3, severe GS (50–75%) and 4, diffuse GS involving >75% of the glomerular tuft. GS index (GSI) for each rat was calculated as a mean value of all glomerular scores obtained.17 Tubulointerstitial lesion indexes were determined using a semiquantitative scoring system.17 Ten fields per kidney were examined, and lesions were graded from 0 to 3 (0, no change; 1, changes affecting <25% of the section; 2, changes affecting 25–50% of the section and 3, changes affecting 50–100% of the section), according to the area with tubulointerstitial lesions (tubular atrophy, casts, interstitial inflammation and fibrosis). The score index in each rat was expressed as a mean value of all scores obtained.
Semiquantitative immunoblotting
The dissected kidneys were homogenized in ice-cold isolation solution containing 0.3 M sucrose, 25 mM imidazole, 1 mM EDTA, 8.5 μM leupeptin and 1 mM phenylmethylsulfonyl fluoride, with pH 7.2. The homogenates were centrifuged at 1000 g for 15 min at 4 °C to remove whole cells, nuclei and mitochondria. The total protein concentration was measured (Pierce BCA protein assay reagent kit, Pierce, Rockford, IL, USA). All samples were adjusted with isolation solution to reach the same final protein concentrations and solubilized at 65 °C for 15 min in SDS-containing sample buffer and then stored at −20 °C. To confirm equal loading of protein, an initial gel was stained with Coomassie blue. Sodium dodecyl sulfate-polyacrylamide gel electrophoresis was performed on 9 or 12% polyacrylamide gels. The proteins were transferred by gel electrophoresis (Bio-Rad Mini Protean II, Bio-Rad, Hercules, CA, USA) onto nitrocellulose membranes (Hybond ECL RPN3032D, Amersham Pharmacia Biotech, Little Chalfont, UK). The blots were subsequently blocked with 5% milk in PBST (80 mM Na2HPO4, 20 mM NaH2PO4, 100 mM NaCl, 0.1% Tween 20, pH 7.5) for 1 h and incubated overnight at 4 °C with primary antibodies followed by incubation with secondary anti-rabbit (P448, DAKO, Glostrup, Denmark) or anti-mouse (P447, DAKO) horseradish peroxidase-conjugated antibodies. The labeling was visualized by an enhanced chemiluminescence system.
We used previously characterized antibodies. Affinity-purified rabbit polyclonal antibodies were used against the renal sodium transporters; NHE3, Na-K-ATPase α1 and the thiazide-sensitive Na+:Cl− cotransporter (NCC).18 Affinity-purified rabbit polyclonal antibodies to TGF-β1 (Santa Cruz Biotechnology, Santa Cruz, CA, USA), ED-1 (Serotec, Raleigh, NC, USA), cyclooxygenase-2 (COX-2, Cayman Chemical, Ann Arbor, MI, USA), heat shock protein 25 (HSP25, Upstate Biotechnology, Lake Placid, NY, USA) and β-actin (Sigma, St Louis, MO, USA) were commercially obtained.
mRNA Expression of endothelin system and inflammatory markers
The mRNA expression of ET-1, type A ET receptor (ETAR), type B ET receptor (ETBR), tumor necrosis factor (TNF)-α, interleukin (IL)-1β, interferon (IFN)-γ, TGF-β1, monocyte chemoattractant protein (MCP)-1 and intercellular adhesion molecule (ICAM)-1 was determined by real-time PCR. cDNA was made by reverse-transcribing 5 μg of total RNA using oligo (dT) priming and superscript reverse transcriptase II (Invitrogen, Carlsbad, CA, USA). cDNA was quantified using the Smart Cycler II System (Cepheid, Sunnyvale, CA, USA) and SYBR Green was used for detection. PCR was performed using the Rotor-Gene 3000 Detector System (Corbette Research, Mortlake, New South Wales, Australia). Sequences of primers are listed in Table 1. The PCR was performed according to the following steps: (1) 95 °C for 5 min; (2) 95 °C for 20 s; (3) 58–62 °C for 20 s (optimized for each primer pair); (4) 72 °C for 30 s and (5) 85 °C for 6 s to detect SYBR Green. Steps 2–5 were repeated for an additional 45 cycles, whereas at the end of the last cycle, the temperature was increased from 60 to 95 °C to produce a melt curve. Data from the reaction were collected and analyzed with the Corbett Research Software. The comparative critical threshold (CT) values from quadruplicate measurements were used to calculate the gene expression, with normalization to GAPDH as an internal control.19 Melting curve analysis was performed to enhance specificity of the amplification reaction.
Enzyme immunoassay for ET-1
Concentrations of ET-1 in plasma, kidney tissue and urine extracts were determined using an ET-1 enzyme-linked immunosorbent assay kit (R&D Systems, Minneapolis, MN, USA). The cross-reactivity of the antibody for the former was 0.1% for all Big ETs, 14% for ET-3 and 45% for ET-2. The assay procedure was carried out according to the manufacturer’s instructions.
Statistical analyses
Results are expressed as mean±s.e.m. Multiple comparisons among the groups were made by one-way ANOVA and post hoc Tukey HSD test. P-values <0.05 were considered significant.
Results
Blood pressure and renal function
Table 2 summarizes the blood pressure and body weight of control, DOCA-salt and RGT-treated DOCA-salt rats. The only DOCA-salt rats showed 20% mortality rate, whereas all of the controls and D+RGT rats survived during the experiments. The systolic blood pressure was markedly increased in DOCA-salt rats compared with control rats, whereas RGT attenuated increased systolic blood pressure in DOCA-salt rats at 4 weeks after DOCA implantation. Kidney weights and left ventricular weights were increased in DOCA-salt rats compared with controls, which were attenuated by RGT treatment.
Table 3 summarizes the renal functions. DOCA-salt rats decreased creatinine clearance and increased plasma creatinine levels compared with controls. In addition, the fractional excretion of sodium increased, suggesting impaired tubular sodium reabsorption in DOCA-salt rats. In addition, the urinary microalbumin excretion ratio (UAE) was increased. RGT treatment lowered plasma creatinine levels, increased creatinine clearance and reduced fractional excretion of sodium and UAE.
Effect of RGT on pathological changes in DOCA-salt rats
Figure 1 shows morphological change among the three groups. In the PAS stain, tubular cast, obstruction and dilatation were shown in DOCA-salt rats. The GSI attained values almost 10-fold as high as in control rats. Treatment with RGT was associated with a less pronounced increment of GSI. Interstitial expansion was also a prominent component of renal injury in DOCA-salt rats, which was attenuated by RGT treatment
Effect of RGT on endothelin system in DOCA-salt rats
Figure 2a shows the expression of ET-1, ETAR and ETBR in the kidney. The abundance of ET-1 mRNA was significantly increased in kidneys of DOCA-salt rats compared with controls, which was counteracted by RGT treatment. The expression of ETAR was decreased in kidneys of DOCA-salt rats, which was not further affected by RGT treatment. The expression of ETBR was increased in kidneys of DOCA-salt rats, which was attenuated by RGT treatment. ET-1 content in the kidney and its urinary excretion were increased in DOCA-salt HTN rats, which were attenuated by RGT treatment. However, Plasma ET-1 level revealed no difference among the three groups (Figure 2b).
(a) Expression of ET-1, type A ET receptor (ETAR) and type B ET receptor (ETBR) in whole kidney. Columns show densitometric data representing control, and the DOCA-salt and rosiglitazone treatment groups. (b) The ET-1 content in plasma, urine and the kidney. *P<0.05 compared with control. #P<0.05 compared with the DOCA-salt group.
Effect of RGT on inflammatory markers in DOCA-salt rats
The expression of ED-1, COX-2, HSP25 and TGF-β1 were increased in DOCA-salt rats compared with controls, which are reduced by RGT treatment (Figures 3 and 4). Immunohistochemical staining for TGF-β1 was increased in the cortical glomerulus and interstitium in DOCA-salt rats compared with controls, which was attenuated with RGT treatment (Figure 4). The mRNA expression of TNFα, IL-1β, INFγ, TGF-β1, MCP-1 and ICAM-1 was increased in DOCA-salt rats, which was attenuated by RGT treatment (Figure 5).
Semiquantitative immunoblotting of ED-1, COX-2 and HSP25 in the cortex/OSOM in the kidney. Densitometric analysis revealed that the protein expression of ED-1, COX-2 and HSP25 were increased in DOCA-salt rats compared with controls, which was counteracted by rosiglitazone treatment. *P<0.05 compared with control. #P<0.05 compared with DOCA-salt rats.
Semiquantitative immunoblotting of TGF-β1 in the membrane fraction of cortex/OSOM. Densitometric analysis revealed that the protein expression of TGF-β was increased in DOCA-salt rats, which was counteracted by rosiglitazone treatment. Increased immunolabeling of TGF-β1 in the cortex was shown in DOCA-salt rats, which was reversed by rosiglitazone treatment. Magnification: × 200. *P<0.05 compared with control. #P<0.05 compared with the DOCA-salt group.
Effect of RGT on sodium transporters in DOCA-salt rats
The protein expression of NHE3, Na,K-ATPase α1-subunit and NCC was markedly decreased in the cortex/OSOM in DOCA-salt rats, which was attenuated by RGT treatment (Figure 6).
Semiquantitative immunoblotting of NHE3, Na-K-ATPase α1 and NCC in the membrane fraction of cortex/OSOM. Densitometric analysis revealed decreased expression of NHE3, Na-K-ATPase α1 and NCC in DOCA-salt rats. Rosiglitazone treatment partially prevented the downregulation of NHE3, Na-K-ATPase α1 and NCC in DOCA-salt rats. *P<0.05 compared with control. #P<0.05 compared with the DOCA-salt group.
Expression of RGT alone in unilaterally nephrectomized rats
In unilaterally nephrectomized rats, the protein expression of ED-1, TGF-β1, NHE3 and Na,K ATPase α1 was not changed by RGT treatment (Figure 7).
Discussion
This study provides in vivo evidence of the beneficial effects of PPARγ activators against GS and chronic hypertensive renal injury in an ET-1-dependent model of hypertension. As expected, DOCA-salt hypertensive rats showed systemic arterial hypertension and impaired renal function. These functional changes were accompanied by severe GS and interstitial fibrosis. The detection of inflammatory and profibrotic gene induction and macrophage infiltration in the kidneys of DOCA-salt hypertensive rats supports the notion that inflammatory processes contribute to progressive renal injury and fibrosis.
Earlier studies have shown that ET-1 contributes to the development of high blood pressure and vascular growth in DOCA-salt rats.20 As suggested by earlier in vitro studies, PPARα and PPARγ are potent inhibitors of ET-1 production in vascular cells.15 This study showed that ET-1 mRNA expression was increased in the kidneys in association with increased blood pressure and decreased GFR. These findings suggest that the enhanced renal production of ET-1 has a role in the development of hypertension and renal dysfunction. Physiological and pathophysiological responses to ET-1 in various tissues are mediated by interactions with ETA and ETB receptor subtypes. ETAR is expressed mainly in the vascular tissues, where it mediates vasoconstrictive and growth effects.21 The function of ETBR appears to be more complex, as it is located on a variety of cell types.22 ETBR is particularly abundant in the renal medullary epithelium, where it appears to influence tubular sodium and water reabsorption, accounting for the natriuretic and diuretic actions of ET-1.23 The selective blockade of ETBR resulted in increased blood pressure and increased sodium and water retention in DOCA-salt rats.24 These results suggest that ETAR has an important role in the pathogenesis of DOCA-salt hypertension. On the other hand, it seems likely that an ETBR-mediated pathway protects against vascular and renal injuries in this model of hypertension. Therefore, decreased ETAR and increased ETBR mRNA expression in DOCA-salt hypertensive rats may have compensatory roles in vasoconstriction and renal injury by ET-1.
Our study showed that the ET-1 content in the kidneys and its urinary excretion were increased in DOCA-salt hypertensive rats, but that it could be attenuated by RGT treatment. Although the mechanisms underlying the increased production of ET-1 in the kidneys in DOCA-salt hypertension are unclear, inflammation has been suggested to stimulate renal ET-1 production. ET-1 synthesis and release were increased on exposure to inflammatory cytokines such as TNFα and C-reactive protein in mesangial and vascular endothelial cells.25, 26 Indeed, the blockade of inflammation by a TNFα inhibitor suppressed renal injury in DOCA-salt rats.27 In this study, ET-1 expression was increased in association with the upregulation of inflammatory chemokines (TNFα, IL-1β and IFNγ) and adhesion molecules (MCP-1 and ICAM-1) in DOCA-salt hypertension, and these effects were counteracted by RGT. These findings suggest that RGT decreases ET-1 synthesis by inhibiting tissue inflammation in DOCA-salt hypertension.
In this study, RGT therapy reduced inflammatory marker expression. Such infiltration has been shown to participate in the initiation and progression of GS and tubulointerstitial fibrosis.28 Consistent with this, RGT abrogated the renal expression of a number of inflammatory mediators in chronic cyclosporin nephrotoxicity29 and lipopolysaccharide-induced renal injury.30 It has been shown that macrophage infiltration occurs in DOCA-salt hypertension and contributes to GS.31 In addition, COX-2 expression was increased, and COX-2 inhibitor treatment decreased tubulointerstitial injury in DOCA-salt rats.32 These findings suggest that macrophage infiltration and inflammation contribute to renal injury associated with mineralocorticoid hypertension and that RGT treatment reduces inflammatory reactions and renal injury.
Alterations in HSP expression have been suggested to have a protective role against tissue damage. The molecular adaptation of vascular endothelial cells to oxidative stress is accompanied by HSP induction. Human HSP27 and mouse HSP25 form large oligomers when overexpressed in vitro, acting as molecular chaperones and protecting cells from heat shock and oxidative stress.33 In addition, angiotensin II infusion induces renal HSP25.33, 34 These findings show the beneficial and compensatory roles of HSP25. In this study, HSP25 expression was increased in the kidneys of DOCA-salt rats; thus, it may have a protective role in the pathogenesis of hypertension and renal damage. Interestingly, RGT treatment attenuated HSP expression in the kidneys of DOCA-salt hypertensive rats, in association with the prevention of renal injury.
Levels of the multifunctional cytokine TGF-β1 are elevated in patients with hypertension, and TGF-β1 is likely a prime mediator in the progression of renal disease. One of the mechanisms by which TGF-β1 induces fibrogenesis is the stimulation of extracellular matrix protein production and inhibition of matrix degradation. In this study, TGF-β1 expression was increased and GS was prominent in DOCA-salt rats, and these effects were attenuated by RGT treatment. Thus, histological recovery from GS by RGT treatment may contribute to the restoration of renal function and decrease in blood pressure.
This study suggests that ET-1 and TGF-β1 are key players in preventing glomerular/tubulointerstitial damage and in lowering blood pressure in DOCA-salt rats treated with RGT. However, it is possible that alterations in the renin-angiotensin system (RAS) by RGT treatment are associated with the prevention of renal injury in DOCA-salt rats. The association between PPARγ and angiotensin II is not fully understood, but recent studies have shown that TZDs antagonize the in vivo and in vitro actions of angiotensin II,35 while downregulating the angiotensin II receptor.36 In addition, it has been reported that PPARγ activation inhibits angiotensin II synthesis, apoptosis and proliferation in the mesangial cells of spontaneously hypertensive rats.37 These findings indicate that alterations in renin-angiotensin system by RGT treatment are associated with the prevention of renal injury in DOCA-salt rats.
In this study, the fractional excretion of sodium was increased in DOCA-salt rats, suggesting a decrease in sodium reabsorption in the renal tubules. Accordingly, the expression of NHE3, Na+/K+-ATPase α1 and NCC was decreased in the kidneys of DOCA-salt rats. Thus, it may be that decreased sodium absorptive activity in the renal tubules contributes to the avoidance of the salt-retaining effects of mineralocorticoids. Importantly, the decreased expression of sodium transporters was counteracted by RGT treatment. The molecular mechanisms by which the expression of renal sodium transporters is decreased in the kidneys of DOCA-salt rats are unknown. A recent study showed that LPS-induced inflammation induced the downregulation of renal sodium transporters and that cytokines decreased the expression of renal sodium transporters in cortical collecting duct cells.38 These findings suggest that the downregulation of renal sodium transporters, which may account for the tubular dysfunction in DOCA-salt hypertension, is mediated by inflammation, and that this can be prevented by RGT treatment, leading to the resumption of renal tubular sodium reabsorption.
Unilateral nephrectomy causes a number of changes in the remnant kidneys, including hypertrophy and cellular proliferation.39 Thus, it was assumed that RGT treatment would induce different baseline changes in uninephrectomized contralateral kidneys. This study showed that RGT did not affect the abundance of ED-1, TGF-β1, NHE3 or Na+/K+ ATPase α1 in the remnant kidneys, suggesting that RGT has selective renoprotective effects on hypertensive renal injury in DOCA-salt hypertension.
In conclusion, RGT treatment decreases blood pressure and is effective in preventing the progression of renal injury in DOCA-salt hypertension, the mechanisms of which are associated with anti-inflammatory and anti-fibrotic effects through the reduced overexpression of ET-1, ED-1, COX-2 and TGF-β1.
Conflict of interest
The authors declare no conflict of interest.
References
Day C . Thiazolidinediones: a new class of antidiabetic drugs. Diabet Med 1999; 16: 179–192.
Raji A, Seely EW, Bekins SA, Williams GH, Simonson DC . Rosiglitazone improves insulin sensitivity and lowers blood pressure in hypertensive patients. Diabetes Care 2003; 26: 172–178.
Gerber P, Lubben G, Heusler S, Dodo A . Effects of pioglitazone on metabolic control and blood pressure: a randomised study in patients with type 2 diabetes mellitus. Curr Med Res Opin 2003; 19: 532–539.
Zhang HY, Reddy SR, Kotchen TA . Antihypertensive effect of pioglitazone is not invariably associated with increased insulin sensitivity. Hypertension 1994; 24: 106–110.
Marx N, Schonbeck U, Lazar MA, Libby P, Plutzky J . Peroxisome proliferator-activated receptor gamma activators inhibit gene expression and migration in human vascular smooth muscle cells. Circ Res 1998; 83: 1097–1103.
Liu Y, Shi J, Lu J, Meng G, Zhu H, Hou Y, Yin Y, Zhao S, Ding B . Activation of peroxisome proliferator-activated receptor-gamma potentiates pro-inflammatory cytokine production, and adrenal and somatotropic changes of weaned pigs after Escherichia coli lipopolysaccharide challenge. Innate Immun 2009; 15: 169–178.
Guan Y, Breyer MD . Peroxisome proliferator-activated receptors (PPARs): novel therapeutic targets in renal disease. Kidney Int 2001; 60: 14–30.
Iglarz M, Touyz RM, Amiri F, Lavoie MF, Diep QN, Schiffrin EL . Effect of peroxisome proliferator-activated receptor-alpha and -gamma activators on vascular remodeling in endothelin-dependent hypertension. Arterioscler Thromb Vasc Biol 2003; 23: 45–51.
Iglarz M, Touyz RM, Viel EC, Amiri F, Schiffrin EL . Involvement of oxidative stress in the profibrotic action of aldosterone. Interaction with the renin-angiotensin system. Am J Hypertens 2004; 17: 597–603.
Sun Y, Zhang J, Lu L, Chen SS, Quinn MT, Weber KT . Aldosterone-induced inflammation in the rat heart: role of oxidative stress. Am J Pathol 2002; 161: 1773–1781.
Matsumura Y, Hashimoto N, Taira S, Kuro T, Kitano R, Ohkita M, Opgenorth TJ, Takaoka M . Different contributions of endothelin-A and endothelin-B receptors in the pathogenesis of deoxycorticosterone acetate-salt-induced hypertension in rats. Hypertension 1999; 33: 759–765.
Callera GE, Tostes RC, Yogi A, Montezano AC, Touyz RM . Endothelin-1-induced oxidative stress in DOCA-salt hypertension involves NADPH-oxidase-independent mechanisms. Clin Sci 2006; 110: 243–253.
Hartner A, Klanke B, Cordasic N, Amann K, Schmieder RE, Veelken R, Hilgers KF . Statin treatment reduces glomerular inflammation and podocyte damage in rat deoxycorticosterone-acetate-salt hypertension. J Hypertens 2009; 27: 376–385.
Ohtomo S, Izuhara Y, Takizawa S, Yamada N, Kakuta T, van Ypersele de Strihou C, Miyata T . Thiazolidinediones provide better renoprotection than insulin in an obese, hypertensive type II diabetic rat model. Kidney Int 2007; 72: 1512–1519.
Satoh H, Tsukamoto K, Hashimoto Y, Hashimoto N, Togo M, Hara M, Maekawa H, Isoo N, Kimura S, Watanabe T . Thiazolidinediones suppress endothelin-1 secretion from bovine vascular endothelial cells: a new possible role of PPARgamma on vascular endothelial function. Biochem Biophys Res Commun 1999; 254: 757–763.
Sato K, Sugawara A, Kudo M, Uruno A, Ito S, Takeuchi K . Expression of peroxisome proliferator-activated receptor isoform proteins in the rat kidney. Hypertens Res 2004; 27: 417–425.
Gadola L, Noboa O, Marquez MN, Rodriguez MJ, Nin N, Boggia J, Ferreiro A, García S, Ortega V, Musto ML, Ponte P, Sesser P, Pizarrosa C, Ravaglio S, Vallega A . Calcium citrate ameliorates the progression of chronic renal injury. Kidney Int 2004; 65: 1224–1230.
Kim SW, Wang W, Nielsen J, Praetorius J, Kwon TH, Knepper MA, Frøkiaer J, Nielsen S . Increased expression and apical targeting of renal ENaC subunits in puromycin aminonucleoside-induced nephrotic syndrome in rats. Am J Physiol Renal Physiol 2004; 286: F922–F935.
Livak KJ, Schmittgen TD . Analysis of relative gene expression data using real-time quantitative PCR and the 2(−Delta Delta C(T)) Method. Methods 2001; 25: 402–408.
Schiffrin EL . Role of endothelin-1 in hypertension and vascular disease. Am J Hypertens 2001; 14: 83S–89S.
Terada Y, Tomita K, Nonoguchi H, Yang T, Marumo F . Different localization of two types of endothelin receptor mRNA in microdissected rat nephron segments using reverse transcription and polymerase chain reaction assay. J Clin Invest 1992; 90: 107–112.
Pollock DM, Keith TL, Highsmith RF . Endothelin receptors and calcium signaling. FASEB J 1995; 9: 1196–1204.
Garvin J, Sanders K . Endothelin inhibits fluid and bicarbonate transport in part by reducing Na+/K+ ATPase activity in the rat proximal straight tubule. J Am Soc Nephrol 1991; 2: 976–982.
Pollock DM, Allcock GH, Krishnan A, Dayton BD, Pollock JS . Upregulation of endothelin B receptors in kidneys of DOCA-salt hypertensive rats. Am J Physiol Renal Physiol 2000; 278: F279–F286.
Kohan DE . Production of endothelin-1 by rat mesangial cells: regulation by tumor necrosis factor. J Lab Clin Med 1992; 119: 477–484.
Verma S, Li SH, Badiwala MV, Weisel RD, Fedak PW, Li RK, Dhillon B, Mickle DA . Endothelin antagonism and interleukin-6 inhibition attenuate the proatherogenic effects of C-reactive protein. Circulation 2002; 105: 1890–1896.
Elmarakby AA, Quigley JE, Imig JD, Pollock JS, Pollock DM . TNF-alpha inhibition reduces renal injury in DOCA-salt hypertensive rats. Am J Physiol Regul Integr Comp Physiol 2008; 294: R76–R83.
Blasi ER, Rocha R, Rudolph AE, Blomme EA, Polly ML, McMahon EG . Aldosterone/salt induces renal inflammation and fibrosis in hypertensive rats. Kidney Int 2003; 63: 1791–1800.
Ahn KO, Lim SW, Yang HJ, Li C, Sugawara A, Ito S, Choi BS, Kim YS, Kim J, Yang CW . Induction of PPAR gamma mRNA and protein expression by rosiglitazone in chronic cyclosporine nephropathy in the rat. Yonsei Med J 2007; 48: 308–316.
Lee S, Kim W, Kang KP, Moon SO, Sung MJ, Kim DH, Kim HJ, Park SK . Agonist of peroxisome proliferator-activated receptor-gamma, rosiglitazone, reduces renal injury and dysfunction in a murine sepsis model. Nephrol Dial Transplant 2005; 20: 1057–1065.
Artner A, Porst M, Gauer S, Prols F, Veelken R, Hilgers KF . Glomerular osteopontin expression and macrophage infiltration in glomerulosclerosis of DOCA-salt rats. Am J Kidney Dis 2001; 38: 153–164.
Adeagbo AS, Zhang X, Patel D, Joshua IG, Wang Y, Sun X, Iqbu IN, Oriowo MA . Cyclo-oxygenase-2, endothelium and aortic reactivity during deoxycorticosterone acetate salt-induced hypertension. J Hypertens 2005; 23: 1025–1036.
Rogalla T, Ehrnsperger M, Preville X, Kotlyarov A, Lutsch G, Ducasse C, Paul C, Wieske M, Arrigo AP, Buchner J, Gaestel M . Regulation of Hsp27 oligomerization, chaperone function, and protective activity against oxidative stress/tumor necrosis factor alpha by phosphorylation. J Biol Chem 1999; 274: 18947–18956.
Ishizaka N, Aizawa T, Ohno M, Usui Si S, Mori I, Tang SS, Ingelfinger JR, Kimura S, Nagai R . Regulation and localization of HSP70 and HSP25 in the kidney of rats undergoing long-term administration of angiotensin II. Hypertension 2002; 39: 122–128.
Schiffrin EL . Peroxisome proliferator-activated receptors and cardiovascular remodeling. Am J Physiol Heart Circ Physiol 2005; 288: H1037–H1043.
Sugawara A, Takeuchi K, Uruno A, Kudo M, Sato K, Ito S . Effects of mitogen-activated protein kinase pathway and co-activator CREP-binding protein on peroxisome proliferator-activated receptor-gamma-mediated transcription suppression of angiotensin II type 1 receptor gene. Hypertens Res 2003; 26: 623–628.
Efrati S, Berman S, Ilgiyeav E, Averbukh Z, Weissgarten J . PPAR-gamma activation inhibits angiotensin II synthesis, apoptosis, and proliferation of mesangial cells from spontaneously hypertensive rats. Nephron Exp Nephrol 2007; 106: e107–e112.
Schmidt C, Hocherl K, Schweda F, Kurtz A, Bucher M . Regulation of renal sodium transporters during severe inflammation. J Am Soc Nephrol 2007; 18: 1072–1083.
Valentin JP, Sechi LA, Griffin CA, Humphreys MH, Schambelan M . Gene expression of the renin-angiotensin system in compensatory renal hypertrophy secondary to contralateral nephrectomy. Arch Mal Coeur Vaiss 1994; 87: 1115–1117.
Acknowledgements
This research was supported by the Korean Society of Nephrology (2008) and the Special Research Program of Chonnam National University (2009).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bae, E., Kim, I., Ma, S. et al. Rosiglitazone prevents the progression of renal injury in DOCA-salt hypertensive rats. Hypertens Res 33, 255–262 (2010). https://doi.org/10.1038/hr.2009.217
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2009.217
Keywords
This article is cited by
-
Morphological Evaluation of the Influence of the Peptide Complex from Tissue of Porcine Kidneys on the Experimental Urolithiasis
Bulletin of Experimental Biology and Medicine (2017)
-
Additive effect of PPAR-γ agonist and ARB in treatment of experimental IgA nephropathy
Pediatric Nephrology (2011)