Abstract
Purpose:
The current curative treatment of Fanconi anemia is hematopoietic stem cell transplantation; this treatment has a higher rate of successful outcome when donors are compatible siblings. Therefore some families opt to have a healthy and compatible baby after selecting an embryo using preimplantation genetic diagnosis with human leukocyte antigen (HLA) typing. This study aims to estimate the success rate of this procedure from the family’s perspective.
Methods:
Genetic and embryology data were collected from genetic reports provided by the families.
Results:
A total of 524 oocytes (14.1 oocytes/cycle) and 299 embryos were generated (8.0 embryos/cycle) after 38 in vitro fertilization cycles. Sixteen embryos were transferred to the uterus because they were non–Fanconi anemia and HLA matched. One baby was born. A younger couple delivered a healthy and HLA-compatible baby after four cycles. Therefore, the success rate per cycle is less than 5% (two babies from 42 trials).
Conclusion:
While Fanconi anemia per se does not worsen the probability of success, a critical factor is advanced maternal age; a late diagnosis leads to few transferrable embryos and high rates of aneuploidy. Families should be informed in advance of the many trials that they will probably need to undergo even if a haploidentical younger relative is available as an oocyte donor.
Genet Med 17 11, 935–938.
Similar content being viewed by others
Introduction
The only curative treatment for many blood disorders is hematopoietic stem cell transplantation, which has a higher rate of successful outcome when the donors are compatible siblings. For this reason, a number of affected families opt to have an human leukocyte antigen (HLA)–compatible baby by selecting an embryo using preimplantation genetic diagnosis (PGD) with HLA typing1 (PGD + HLA) to generate a donor for an affected child. In fact, this procedure was initially developed to provide a donor for a patient with Fanconi anemia (FA) and was later applied to other blood disorders when transplantation is not urgent and parents are of a reproductive age.2,3 FA is a rare genetic syndrome characterized by bone marrow failure, congenital malformations, chromosome fragility, and a predisposition to cancer. Mutations in 16 genes (FANCA, B, C, D1, D2, E, F, G, I, J, L, M, N, O, P, and Q) are known to cause FA, including one recently identified by our team via whole-exome sequencing.4 Early genetic subtyping and mutational analysis of this and related disorders are extremely important, not only for proper diagnosis, genetic counseling, and management, as for any genetic disease, but also for the implementation of curative therapies including hematopoietic stem cell transplantation following embryo selection.
Most of the news and literature available on the topic of PGD and “savior babies” comes from in vitro fertilization (IVF) clinics with a potential bias toward positive outcomes given that unsuccessful trials often are not reported or announced in the mass media. As co-coordinator of the Spanish FA Research Network and reference laboratory in the genetic diagnosis of Spanish patients with FA,5 we are in contact with all Spanish families with FA willing to undergo embryo selection. The aim of this study is to provide families with FA and their clinicians and genetic counselors with an estimate of the success rate of this procedure from the family’s perspective. For this purpose, we systematically collected information about the PGD experience of eight Spanish families with FA willing to have a savior baby.
Methods
In this study we followed eight Spanish families with FA complementation group A (FANCA) over a period of 11 years. To avoid any selection bias, we included all families with FA undergoing PGD + HLA without any selection based on procedure success, maternal age, or gene. Collectively, these eight families carried out 42 PGD + HLA selection trials. To our knowledge, this is the largest series of individual PGD + HLA cycles for FA ever reported. All cycles were performed in specialized reproductive clinics in the United States, Belgium, and Spain. IVF reports with detailed embryology and genetic data per cycle were provided by the families for this study. Data regarding maternal age, number of IVF cycles performed, number of oocytes retrieved per cycle, number of embryos obtained in each cycle, number of non-FA embryos (either carriers or noncarriers of FANCA mutations), number of transferrable embryos (non-FA and HLA-matched), and number of transferred embryos were collected. We followed up with all the families to determine the number of pregnancies and abortions and the number of babies born. Aneuploidy data also were collected from the genetic reports when available. Aneuploidy was tested by fluorescence in situ hybridization, polymerase chain reaction, or array comparative genomic hybridization,depending on the date of the IVF cycle and the reporting IVF clinic.
Results
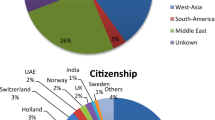
Of the eight families and 42 IVF cycles followed in this study, detailed data on PGD + HLA procedures are available for 38 cycles in seven families, with a maternal age of 39.3 ± 1.8 years (range: 37–41 years) ( Table 1 ). As graphically shown in Figure 1 , from a total of 524 oocytes (14.1 ± 7.9 per cycle), 299 embryos (8.0 ± 6.1 per cycle) were generated by intracytoplasmic sperm injection. Of the embryos for which single blastocytes could be analyzed, 75 were non-FA (including monoallelic carriers or noncarriers), 26 were non-FA and HLA-compatible, and 16 could be transferred to the uterus. Five pregnancies occurred (confirmed by ultrasound and hormonal testing), but only one baby was born. Therefore, the success rate per IVF cycle was 2.6% (one baby born from 38 trials), and the live birth rate per embryo transferred was 6.25% (one baby born from 16 embryos transferred). When considering the eighth family, who had a baby after four cycles, the success rate was still very low: two babies born from 42 trials (4.8%). However, it is important to highlight that this mother was 25 years old, which is much younger than the rest of the mothers included in this study.
The causes of the four documented abortions in this study are unknown. In addition to FA and HLA genetic status, 28 embryos were concurrently tested for chromosomal numerical abnormalities by fluorescence in situ hybridization, polymerase chain reaction, or array comparative genomic hybridization. In most cases, not all 23 chromosomes were assayed; however, 15 of 28 embryos (53.6%) were aneuploidal, including a monosomy 6 that was indirectly detected in one embryo as a result of abnormal HLA markers. Of the four embryos that resulted in spontaneous abortion, none underwent aneuploidy testing. Given the advanced maternal age, however, the probability that these embryos were aneuploidal for any of the 23 chromosomes is extremely high.
Discussion
In addition to the known low Mendelian probability (only 3 of 16 embryos are theoretically expected to be non-FA and HLA-matched), there are a number of other factors that may lead to the low success rate observed here, including a small initial number of embryos; loss of embryos during culture, manipulation, and selection procedures; a low implantation rate; a low rate of live births per embryo transferred; and a high incidence of miscarriages, most probably caused by aneuploidy, especially at advanced maternal ages. In our cohort of families with FA, the mean number of oocytes retrieved (14.1 per cycle), embryos obtained (8 per cycle), and aneuploidal embryos (53.6%) obtained is similar to that reported in larger non-FA PGD cohorts with a similar maternal age (39–40 years old).6 This observation suggests that the FA disease per se does not worsen the success rate of generating a savior baby. The critical point in FA seems to be advanced maternal age. Unfortunately, advanced maternal age is unavoidable in most cases of FA, given that a diagnosis of FA is rare in newborns. In fact, the mean age at onset of hematological disease in FA is 7 years,5,7 and the majority of patients are diagnosed months to years after onset.
Given that advanced maternal age negatively affects the success rate of IVF, one Spanish family with FA that had unsuccessfully performed four IVF cycles (couple 6 in Table 1 ) opted to use a haploidentical maternal cousin as an oocyte donor. The cousin was 10 years younger than the biological mother and was not a carrier of the maternal mutation. In total, three cycles were performed. No pregnancy occurred after the first two PGD + HLA trials. In the first trial two of four embryos were HLA-compatible, but one of these was determined by array comparative genomic hybridization to be aneuploidal. The matched embryo with normal ploidy was transferred to the uterus; however, no pregnancy occurred. In the second trial only two embryos were analyzed for HLA, carrier status, and aneuploidy. Neither of these embryos was HLA-matched with the patient with FA. In the third trial eight embryos were biopsied. Seven were not mutation carriers, of which five were HLA-matched, and three of them were not aneuploidal according to array comparative genomic hybridization. One non-FA, nonaneuploidal, and HLA-matched embryo was initially transferred to the uterus but did not implant. The two remaining non-FA, nonaneuploidal, and HLA-matched embryos were transferred 1 month later, and both implanted. The pregnancy with two fetal sacs currently progresses normally at week 30 (26 January 2015). This family’s experience demonstrates the extreme difficulties that can arise during attempts to generate a savior baby. Three other families in our study underwent 10, 7, and 7 unsuccessful trials. Therefore, clinicians and families with FA considering PGD + HLA must make informed decisions, taking into account that probably more than 95% of the IVF cycles will not result in a birth and that the probability worsens as the age of the mother approaches 40 years. Knowledge of success rates is important for families, not only in psychological terms but also for economic reasons; PGD + HLA in private reproductive clinics can be extremely expensive for families or the public health system. In addition, families should be aware in advance of the many trials that they will probably need to undergo even if a haploidentical female relative is available to act as a younger oocyte donor.
Despite the low success rate of generating savior babies, the outlook for patients with FA has been improved by several recent advances. The clinical outcome of transplantation in FA using HLA-matched nonsiblings as hematopoietic stem cell donors has greatly improved in the past few years because of optimized hematopoietic stem cell transplantation drugs and protocols.8 In addition, clinical trials of FA gene therapy are currently underway.9 Finally, disease-free blood progenitors from skin fibroblasts of patients with FA were recently generated via induced pluripotent stem cells, setting the path for a future cure through regenerative medicine for patients with FA and other blood disorders.10,11,12 We hope that these therapeutic advances will make the generation of savior babies to cure FA and other genetic blood disorders unnecessary in the years to come.
Disclosure
The authors declare no conflict of interest.
References
Verlinsky Y, Rechitsky S, Schoolcraft W, Strom C, Kuliev A . Preimplantation diagnosis for Fanconi anemia combined with HLA matching. JAMA 2001;285:3130–3133.
Grewal SS, Kahn JP, MacMillan ML, Ramsay NK, Wagner JE . Successful hematopoietic stem cell transplantation for Fanconi anemia from an unaffected HLA-genotype-identical sibling selected using preimplantation genetic diagnosis. Blood 2004;103:1147–1151.
Samuel GN, Strong KA, Kerridge I, Jordens CF, Ankeny RA, Shaw PJ . Establishing the role of pre-implantation genetic diagnosis with human leucocyte antigen typing: what place do “saviour siblings” have in paediatric transplantation? Arch Dis Child 2009;94:317–320.
Bogliolo M, Schuster B, Stoepker C, et al. Mutations in ERCC4, encoding the DNA-repair endonuclease XPF, cause Fanconi anemia. Am J Hum Genet 2013;92:800–806.
Castella M, Pujol R, Callén E, et al. Origin, functional role, and clinical impact of Fanconi anemia FANCA mutations. Blood 2011;117:3759–3769.
Franasiak JM, Forman EJ, Hong KH, et al. The nature of aneuploidy with increasing age of the female partner: a review of 15,169 consecutive trophectoderm biopsies evaluated with comprehensive chromosomal screening. Fertil Steril 2014;101:656–663.e1.
Kutler DI, Singh B, Satagopan J, et al. A 20-year perspective on the International Fanconi Anemia Registry (IFAR). Blood 2003;101:1249–1256.
Peffault de Latour R, Porcher R, Dalle JH, et al.; FA Committee of the Severe Aplastic Anemia Working Party; Pediatric Working Party of the European Group for Blood and Marrow Transplantation. Allogeneic hematopoietic stem cell transplantation in Fanconi anemia: the European Group for Blood and Marrow Transplantation experience. Blood 2013;122:4279–4286.
Tolar J, Becker PS, Clapp DW, et al. Gene therapy for Fanconi anemia: one step closer to the clinic. Hum Gene Ther 2012;23:141–144.
Raya A, Rodríguez-Pizà I, Guenechea G, et al. Disease-corrected haematopoietic progenitors from Fanconi anaemia induced pluripotent stem cells. Nature 2009;460:53–59.
Liu GH, Suzuki K, Li M, et al. Modelling Fanconi anemia pathogenesis and therapeutics using integration-free patient-derived iPSCs. Nat Commun 2014;5:4330.
Rio P, Baños R, Lombardo A, et al. Targeted gene therapy and cell reprogramming in Fanconi anemia. EMBO Mol Med 2014;6:835–848.
Acknowledgements
The authors are grateful to all participating families with Fanconi anemia for sharing their experiences and to Ana Molina for collecting data. Also, the authors thank the clinicians of the Spanish Fanconi Anemia Network. J.S.’s laboratory is currently funded by the Generalitat de Catalunya (SGR0489-2009; SGR317-2014), the ICREA-Academia programme, the Marató de TV3 (project 464/C/2012), the Spanish Ministry of Science and Innovation (projects CB06/07/0023 and SAF2012-31881), the European Commission (EUROFANCOLEN project HEALTH-F5-2012–305421), and the European Regional Development FEDER Funds. CIBERER is an initiative of the Instituto de Salud Carlos III, Spain.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Trujillo, J., Surralles, J. Savior siblings and Fanconi anemia: analysis of success rates from the family’s perspective. Genet Med 17, 935–938 (2015). https://doi.org/10.1038/gim.2014.206
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2014.206
Keywords
This article is cited by
-
Creating human germ cells for unmet reproductive needs
Nature Biotechnology (2016)