Abstract
Purpose: To determine the prevalence and psychosocial correlates of depressive symptoms among adolescents and adults with Klinefelter syndrome.
Methods: Individuals (n = 310) aged 14–75 years with self-reported Klinefelter syndrome were recruited from regional and national support networks to complete a web-based survey. Depressive symptoms were assessed using the Center for Epidemiologic Studies Depression Scale. Perceived consequences (Illness Perceptions Questionnaire), perceived stigma (Perceived Social Stigmatization Scale), and coping (Ways of Coping Checklist-Revised) were also measured and evaluated as correlates of depressive symptoms.
Results: Overall, 68.8% of the study participants reported clinically significant levels of depressive symptoms as indicated by a Center for Epidemiologic Studies Depression Scale score ≥16. The use of emotion-focused coping strategies (P < 0.01), perceptions of stigmatization (P < 0.01), perceived negative consequences of Klinefelter syndrome (P < 0.01), and the importance of having children in the future (P < 0.05) were all significantly associated with depressive symptoms.
Conclusions: Individuals with Klinefelter syndrome may be at increased risk for depression. Routine screening for depressive symptoms and appropriate referral and evaluation may be warranted.
Similar content being viewed by others
Main
Klinefelter syndrome (XXY), or 47, XXY, is the most common chromosomal aberration among men, occurring with an estimated frequency of 1:500 to 1:1000 live male births. The physical and cognitive phenotype associated with XXY is highly variable. Individuals with XXY may have hypogonadism, fertility problems, tall stature, gynecomastia, language-based learning disabilities, and disorders of executive function.
Previous research has raised concerns that individuals with XXY are at increased risk for psychiatric disorders, including depression, anxiety, schizophrenia, and other psychotic disorders.1–6 A survey of hospital admissions and discharge diagnoses among individuals with XXY in Denmark (n = 832) and a randomly selected age-matched control group (n = 4033) found that individuals with XXY had an increased relative risk of being hospitalized for psychiatric disorders (hazard ratio: 3.65), particularly for psychoses (hazard ratio: 4.97).7 A psychiatric screening of 31 adults with XXY showed an increased prevalence of psychosis (6.5%) and depression (19.4%).4 Psychiatric interviews and observations of 51 boys with XXY indicated that nearly half of the study participants (45%) demonstrated psychotic symptoms, predominantly auditory hallucinations and paranoid delusions. Four of the participants (8%) were classified as having a psychotic disorder not otherwise specified according to the Diagnostic and Statistical Manual of Mental Disorders, 4th edition, Text Revision. Another two boys were diagnosed with either schizophrenia or schizoaffective disorder. Twelve boys (24%) in this study had experienced an episode of depression.6
In addition to these studies, several prospective longitudinal studies have assessed the prevalence of psychiatric disorders among individuals with XXY. A follow-up study of individuals (n = 19) with XXY diagnosed at birth indicated an increased rate of psychiatric referrals (26%) compared with matched controls (9%).1 Similarly, a study by Bender et al.5 found that adolescents with XXY were more likely to receive psychiatric diagnoses (54%) in contrast to controls (14%). Specifically, among 13 adolescents with XXY, seven had psychiatric diagnoses based on evaluations by a child psychiatrist, with depression being the most common (n = 3).5
A follow-up study by Bender et al.3 assessed psychopathology among 11 young adults with XXY using a quantitative self-report measure (Symptom Checklist-90-R) and psychiatric interview. The investigators found that individuals with XXY rated themselves as experiencing less depressive symptoms and paranoid ideation than matched controls, but the differences were small and did not clearly reflect psychopathology specific to XXY. In contrast, the degree of psychopathology did help to explain the finding that individuals with XXY self-reported higher levels of social adaptation (Social Adjustment Scale-Self-Report) than that reported by the psychiatrist. Individuals with more psychiatric symptoms tended to underreport pathologic symptoms expected to impact social adaptation.3 The small sample size of this follow-up study precludes generalizing from its findings, but it may suggest that individuals with XXY may experience more psychiatric symptoms than what they self-report.
The results of existing studies suggest an increased risk of psychiatric disorders among individuals with XXY, as assessed most often by a psychiatric interview. Although some of the aforementioned studies are limited by sample size, the prevalence of psychiatric disorders found is considerably higher than what has been described in men in the general population. One study reports the lifetime general population prevalence of depression in men as 9.01% and the 12-month general population prevalence in men as 3.56%.8 Studies estimate the lifetime general population prevalence of major depressive disorder as 13.2%8,9 and the 12-month general population prevalence as 5.3–6.7%.8,10 The lifetime prevalence of any psychotic disorder in men is estimated as 3.11%.11 Little is understood about the underlying etiology, manifestations, and consequences of depression in individuals with XXY. However, depression is a leading cause of disability in adolescents and adults in the general population, and there is good evidence that treatment of depression reduces clinical morbidity.12 Thus, it is important to determine the prevalence and impact of depressive symptoms in individuals with XXY to improve recognition and treatment.
The purpose of this study was not only to measure the prevalence of self-reported depressive symptoms among adolescents and adults with XXY but also to examine the psychosocial correlates of depressive symptoms with a sample size sufficiently powered to detect statistically significant effects of key psychosocial variables on depressive symptoms.
MATERIALS AND METHODS
Participants
During an 8-month recruitment period from May 2009 to January 2010, 310 adolescents and adults with self-reported XXY enrolled in the study. Individuals were eligible for participation if they were aged 14 years or older and had self-reported XXY. Participants were recruited through XXY online support networks, including Klinefelter Syndrome and Associates, Klinefelter Syndrome Association, United Kingdom, and Klinefelter Organization, United Kingdom. These organizations advertised the study through website postings, email listservs, and newsletter mailings. In addition, participants were recruited in person at a Klinefelter Syndrome and Associates sponsored conference in California and at a New York City regional support group meeting.
Procedure
Participation involved a one-time self-administered survey. Interested individuals were instructed to either access the electronic version of the survey through SurveyMonkey, a secured Internet site, or to contact the researcher for a paper copy of the survey. Two study websites were developed: one for individuals younger than 18 years and one for individuals aged 18 years and older. The website for individuals younger than 18 years was password protected and required a parent or guardian to contact the researcher to provide permission for participation and to obtain the website password. Participation was anonymous, and compensation was not provided.
This study was approved by the Institutional Review Board at the National Human Genome Research Institute, National Institutes of Health (Protocol no. 09-HG-N142).
Measures
Depressive symptoms were assessed using the Center for Epidemiologic Studies Depression Scale (CES-D),13 one of the most widely used instruments in the field of psychiatric epidemiology. The CES-D was originally designed to screen for depressive symptoms in the general population; however, it has since been used extensively in studies aimed at understanding depressive symptomatology among individuals with a variety of medical conditions. Reliability of the scale (Cronbach's α = 0.85–0.90) and construct validity have been established,13 and normative data for both community and psychiatric populations are available for comparison.14
The CES-D consists of 20 self-report items rated on a 4-point scale of symptom frequency (0 = “Rarely or none of the time, <1 day” to 3 = “Most or all of the time, 5–7 days”). In this study, we decided no missing items were tolerated. Summed scores could range from 0 to 60, with higher scores more likely to be associated with depression. Although the CES-D is not a clinical diagnostic tool, the cutoff score of 16 has been shown to reliably distinguish between clinically depressed and nondepressed persons.13,15–17 The sensitivity, specificity, and positive predictive value found in a community sample of 720 individuals were 64%, 94%, and 33%, respectively, when using a cutoff score of 16.18 Another study using 16 as the cutoff score found high sensitivity (99%) when the CES-D was administered to individuals with acute primary depression, but specificity was reduced (56%) among individuals who were formerly depressed.14 Although 16 is the most widely used cutoff, other studies have recommended using 27 as the cutoff score when screening for depressive symptoms among select medical conditions.19,20 Because this study was interested in comparing the prevalence of depressive symptoms among individuals with an XXY diagnosis to the general population, the widely accepted cutoff score of 16 was used.
The Illness Perception Questionnaire's consequences subscale21 was used to assess the extent to which an XXY diagnosis impacts an individual's life. This subscale has been shown to have good internal reliability (Cronbach's α = 0.82).21 The seven items were rated on a 5-point scale ranging from “strongly disagree” (1) to “strongly agree” (5). Two missing items were tolerated, as recommended by the authors of this measure.22 Scores were summed, and a mean score ranging from 1 to 5 was calculated. High scores indicated an individual perceived his XXY to have serious, negative consequences on his life. In addition, two questions were included to assess perceived severity. Participants were asked to rate how severe they perceived their XXY to be and how severe they perceived their XXY to be in comparison with others with XXY using a 5-point scale that ranged from “not at all severe” (1) to “very severe” (5).
Perceptions of stigmatization were measured using the Perceived Social Stigma Scale,23 a 22-item measure that consists of 14 items that are negative attributes, such as “unhappy,” “slow,” and “shameful” and eight items that are positive attributes, such as “intelligent,” “attractive,” and “worth knowing.” Participants were instructed to insert each attribute into the statement, “As a person with XXY others see me as …,” and to rate the statement on a 4-point scale (1 = “not at all true” to 4 = “very much true”). This scale has been shown to have good internal reliability (Cronbach's α = 0.91).23 In this study, we decided that no missing items were tolerated. Scores were summed and could range from 22 to 88, with higher scores indicating higher levels of perceived stigma.
Coping was measured using the Ways of Coping Checklist-Revised.24 This instrument includes 42 items to assess five categories of coping: problem focused, social support seeking, self-blame, wishful thinking, and avoidance coping. Reliability of the scale (Cronbach's α = 0.74–0.88 for each subscale) and construct validity have been established.24 Participants were prompted to think about a recent stressful situation related to their XXY and to estimate the frequency with which they use particular coping strategies, based on a 4-point scale ranging from 0 “never use” to 3 “regularly use.” A maximum of 20% of missing data were tolerated, as suggested by the author (Peter Vitaliano, PhD, personal communication, 2009).
We aimed to compare the relative proportion of coping strategies used by participants, rather than the frequency with which a particular coping strategy was used by participants, because previous research has suggested that relative scores may be better suited for empirically evaluating the relationship between depression and coping (see the study by Vitaliano et al.25 for a discussion). To calculate the relative scores, each subscale was first summed and then divided by its respective number of items to obtain a mean score. The mean score for each subscale was then divided by the sum of mean scores for all subscales, giving a relative score.
In addition to calculating relative scores for each subscale, we also grouped the three emotion-focused subscales (wishful thinking, self-blame, and avoidance) to compare the relative proportion of emotion-focused and problem-focused coping strategies used by participants and to reduce the number of variables included in our multivariate linear regression analysis. To calculate the relative emotion-focused score, the mean scores for wishful thinking, self-blame, and avoidance subscales were added and divided by the sum of all mean scores. Grouping the emotion-focused subscales into one relative score was first reported in 1990 by Vitaliano et al.26–28 and has since been used in several studies.
Participants were asked to provide information about their current age, age at diagnosis, and time elapsed since learning of diagnosis. The responses to this last question accounted for individuals who were not informed of their diagnosis at the time that it was made. Information about race, ethnicity, marital status, education level, number of children, and relationship to children was also collected. Finally, participants were asked to rate the importance of having children in the next 10 years using a 5-point scale that ranged from “very unimportant” (1) to “very important” (5).
Statistical analyses
Data were analyzed using Statistical Package for Social Sciences (SPSS) version 16.0.2 (SPSS Inc., Chicago, IL). Bivariate associations among all key variables were identified by Pearson correlations. Linear regression analyses were used to assess the influence of each relative coping score (problem focused, social support seeking, self-blame, wishful thinking, and avoidance) on the outcome, depressive symptoms, while controlling for potential confounding. A multivariate linear regression analysis was used to assess associations between the outcome, depressive symptoms, and five key variables (perceived consequences, perceived severity, perceived stigma, emotion-focused coping, and problem-focused coping), controlling for potential confounders (age, race, education level, marital status, whether a participant had children, importance of having children in the future, and time elapsed since learning of the diagnosis). Race was dichotomized as white or nonwhite. Marital status was dichotomized into partnered (individuals who are married or in a partnered relationship) or nonpartnered (individuals who are single, separated/divorced, or widowed). Education level was dichotomized as college graduate or more (postgraduate education) versus some college or technical school or less. An initial model included all potential confounders and key variables. To increase precision on the key variables, while retaining true confounders as control covariates, a backward elimination selection process was used, wherein potential confounders with P values >0.20 were dropped from the model.29,30 The statistical significance of associations between the key variables and depressive symptoms was assessed using the traditional P < 0.05 criterion.
RESULTS
A sample size calculation indicated that 243 participants were needed to have 80% power to detect the effect of a key independent variable explaining a small-to-medium effect size31 of at least 3% of the total variance in depressive symptoms. We exceeded this threshold with a total of 310 participants, although sample sizes for some specific analyses did not include 310 responses due to missing data. Demographic characteristics of the study population are listed in Table 1. The mean age was 40.7 years (SD = 14, range: 14–75 years). Participants were predominantly white (92.2%) and without children (76.4%). Approximately half were married or in a partnered relationship (49.6%) and were diagnosed in adulthood (48%). The average time elapsed since learning of the diagnosis was 15 years (SD = 11.7, range: 0–46 years). The internal reliability values of the measures used in this study ranged from 0.79 to 0.93 (Table 2).
Sixty-nine percent of individuals in this study population scored at, or above, the threshold score of 16, indicating that they had significant levels of depressive symptoms and are at increased risk for depression. As presented in Table 2, the average CES-D score was 24.58 ± 14.7 (range: 0–59), which was significantly higher than that of a standard community sample of 3932 individuals (9.10 ± 8.60)14 (t(4177) = 26.01, P < 0.05), but within the distribution of mean scores reported for individuals with acute depression (38.10 ± 9.01) and individuals who were formerly depressed (14.85 ± 10.06),14 suggesting that these self-reported depressive symptoms may indicate an increased incidence of depression in this population. Bivariate analyses indicated that CES-D scores were significantly positively correlated with perceived negative consequences (Pearson correlation = 0.602, P < 0.01), perceived severity (Pearson correlation = 0.407, P < 0.01), perceived stigma (Pearson correlation = 0.627, P < 0.01), self-blame (Pearson correlation = 0.472, P < 0.01), wishful thinking (Pearson correlation = 0.367, P < 0.01), and avoidance coping (Pearson correlation = 0.345, P < 0.01).
Table 3 summarizes the results of the linear regression analyses conducted to estimate the influence of each relative coping strategy score on depressive symptoms, while controlling for potential confounders. The problem-focused coping relative score accounted for the greatest total variance in depressive symptoms (27%), followed by the self-blame relative score (23%), social support seeking relative score (20%), wishful thinking relative score (9%), and avoidance relative score (9%).
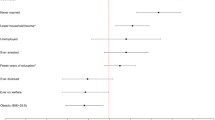
Table 4 summarizes the results of the multivariate linear regression analysis, which showed that emotion-focused coping, perceived stigma, and perceived consequences were significantly positively correlated with depressive symptoms. In addition, greater importance of having children in the future was also associated with greater depressive symptoms. Age, education level, and time elapsed since learning of the diagnosis were included in the model to control for potential confounding. These variables accounted for 61.1% of the variance in depressive symptoms.
DISCUSSION
Depressive symptoms were strikingly prevalent among study participants. Given the degree of morbidity associated with depression in the general population and the demonstrated efficacy of treatment,12 it seems reasonable that all adolescents and adults with XXY should be routinely screened for depressive symptoms and appropriately referred for evaluation and treatment. According to the US Preventative Services Task Force, the specific screening tool used may be less important than making the effort to screen individuals.12 Even a simple two-question tool assessing for depressed mood and anhedonia had 96% sensitivity and 57% specificity, which was similar to several other tools.32 Such screening could logically be suggested as part of the evaluation during any clinical encounter. Providers who tend to see individuals with XXY on a recurring basis (e.g., Internists, Family Practitioners, and Endocrinologists) are more likely to have established good rapport and, thus, be able to elicit important symptoms. On the other hand, specialists seeing a patient for the first time may be better positioned to notice important signs and symptoms that developed gradually over time and, thus, were missed by clinicians who have an established relationship with the patient. Simple screening tools could even be administered by community-based health outreach providers and/or self-administered, as long as opportunities for formal medical evaluation and management are readily available.
The considerable proportion of study participants indicating a clinically significant level of depressive symptoms makes us question whether depressive symptoms are a primary component of XXY, or secondary due to consequences of living with XXY, or both. A study by van Rijn et al.33 found that men with XXY experience difficulty with social-emotional cues and experience increased emotional arousal in response to emotion-inducing events but have problems identifying and verbalizing these emotions, in comparison with the general population. These can be considered possible risk factors for depressive symptoms or other psychiatric problems and may help to explain the prevalence of depressive symptoms among this study's participants. Research aimed at understanding the causes of social cognitive processing and emotion regulation problems found in individuals with XXY have attributed these problems to structural brain differences2,34 and overexpression of genes on the X chromosome that may be involved in social cognition and susceptibility to psychiatric disorders.4,35,36
Moreover, an association between hypogonadism and depression has been suggested, although study results are inconsistent. One population-based study reported a hazard ratio of 4.2 for depression among hypogonadal men.37 Similarly, another population-based study found that depressed men were 1.55–2.71 times more likely than those without depression to have low testosterone levels.38 However, a follow-up of the Massachusetts Male Aging Study found that serum testosterone levels alone were not significantly associated with depressive symptoms, except among men with shorter CAG repeat lengths in the androgen receptor gene.39 Results of randomized, controlled intervention trials are also mixed, with some studies of testosterone replacement in hypogonadal men showing improved mood,40,41 whereas at least one study found no significant difference in mood after testosterone replacement.42
Although the association between hypogonadism and depression may not be fully understood, it can be challenging to distinguish between depressed mood and hypogonadism in light of their shared symptoms. The CES-D captures symptoms specific to depression, including feelings of guilt, hopelessness, helplessness, and psychomotor agitation, but these symptoms may not be entirely distinct from symptoms of low mood that have been, inconsistently, found in hypogonadal men. This study was not designed to distinguish between hypogonadism and depression. Although we are not able to identify the underlying cause of reported symptoms, our data show a high level of self-reported symptoms that are clinically consistent with one or both diagnoses.
In addition, we were able to identify several psychosocial factors that were significantly associated with higher levels of depressive symptoms. The relationship between emotion-focused coping strategies and depressive symptoms is consistent with the findings of the initial studies of the Ways of Coping Checklist-Revised.24,25 Among the three study populations included in the validation study (medical students, spouses of individuals with Alzheimer disease, and psychiatric outpatients), the investigators found a significant positive correlation between wishful thinking and depression and a significant negative relationship between problem-focused coping and depression. Moreover, wishful thinking accounted for the greatest variance in depression (14–21%).24 In this study, wishful thinking accounted for only 9% of the variance in depressive symptoms. Instead, problem-focused coping, followed by self-blame accounted for 27% and 23% of the variance in depressive symptoms, respectively. Other studies of individuals with chronic illnesses43 and genetic conditions44 have also suggested that greater use of emotion-focused coping strategies, particularly wishful thinking and avoidance, is associated with increased self-reported depressive symptoms.
Despite this noted correlation, emotion-focused coping is not considered to be inferior to problem-focused coping. Rather, coping effectiveness is often based on whether a chosen coping strategy matches an individual's appraisal of the stressor.28 More specifically, when a person appraises the stressor as alterable or controllable, problem-focused coping is most often effective. When a “good fit” between a person's appraisal and chosen coping strategy is achieved, individuals are expected to experience fewer psychological symptoms than when there is lack of a good fit.28,45 Our finding of a positive correlation between emotion-focused coping and depressive symptoms raises concern that these strategies are not associated with effective coping, perhaps because emotion-focused coping strategies are not best aligned with the types of stressors encountered by study participants. This highlights a potential opportunity for healthcare providers to intervene.
Coping effectiveness training is one intervention that teaches individuals how to choose a coping strategy according to the extent to which a stressor can be changed.45 This principle may be extended to the use of social support to enhance coping efforts. For example, individuals are asked to create a list of their support persons according to the type of support provided. By identifying individuals who generally provide problem-focused support, such as advice giving, and individuals who provide emotion-focused support, such as listening, individuals are better equipped to choose a support person according to the type of support sought. Coping effectiveness training has been shown to effectively increase individuals' coping efficacy and to reduce depression and anxiety.45,46
The relationship between perceived negative consequences and depressive symptoms is also supported by other studies that have shown that negative illness appraisals are associated with depressive symptoms.47 Illness appraisals may serve as another potent target for interventions aimed at decreasing depressive symptoms, facilitating adaptation, and enhancing quality of life. Brief interventions aiming to challenge unhelpful beliefs and to enhance feelings of control among individuals with chronic medical conditions have been shown to lower concern and anxiety among study participants when compared with controls who received no intervention.48,49 Challenging perceptions of negative consequences and teaching individuals to distinguish between aspects of their life that are associated with XXY or not associated with XXY are cognitive-behavioral-based strategies that healthcare providers can use to intervene. For example, an individual could be asked to create a list categorizing aspects of his life that are associated with XXY or not associated with XXY. This list can be used to challenge an individual's perceptions about the implications of his condition and to increase awareness of those aspects of his life that are not entirely associated with his diagnosis and, therefore, are within his control and amenable to change. Other interventions aimed at improving control include helping individuals to take more active roles in medical decision making, facilitating disclosure decision making, and helping individuals to develop positive responses to stressful situations, so that they feel better prepared for, and more in control of, future interactions.
The positive relationship between perceived stigma and depressive symptoms found in this study is consistent with what has been reported in other studies of individuals living with genetic conditions.44,50 Common strategies used to cope with stigma include secrecy, avoidance, withdrawal (three emotion-focused coping strategies), and education of others (a problem-focused coping strategy).44,50 Emotion-focused coping strategies may “fit” appraisals of stigma considering that individuals are unable to control the way other people perceive them. However, the use of secrecy and/or withdrawal has been associated with depressive symptoms,44 whereas education of others has been shown to be an effective coping strategy in studies of individuals with achondroplasia,51 Marfan syndrome,44 and craniofacial abnormalities.52 Interventions aimed at facilitating effective coping with stigma for individuals with XXY, such as through problem-focused coping strategies as education of others, may impact self-reported levels of depressive symptoms. That said, language-based learning disabilities may limit the effectiveness of educating others as a potential coping strategy for this population.
Finally, the correlation between greater importance of having children and greater self-reported depressive symptoms was not surprising given that infertility poses a major threat to accomplishing this life goal. Studies of men with infertility have found that these men experience considerable emotional distress.53 Although advances in artificial reproductive techniques are offering hope and options to individuals with XXY, the strong emotional responses that accompany infertility must not be ignored. Healthcare providers should be aware that individuals with XXY who are of reproductive age may be at greater risk for depressive symptoms.
A limitation of this study was that clinical data were not collected. Karyotype, medications, and symptoms were not confirmed by medical record review. Participants were not asked and did not report any history of psychiatric diagnosis or use of psychiatric medications or testosterone replacement therapy. In addition, the cross-sectional study design allows conclusions to be drawn regarding correlations between variables, rather than to temporal relationships and causal pathways. We were unable to calculate a response rate because we do not know how many potential participants saw the study advertisements. It is possible that individuals who participate in support groups differ from those who do not. Self-selection introduces a potential bias to our findings, but there is conflicting thought about whether those who respond are more likely in need of support or doing sufficiently well to have the interest to participate in a study. The results of this study are not generalizable to the entire population of adolescents and adults with XXY. Although the study population was largely non-Hispanic white, our large sample size, range of ages, and international participation increase the external validity of our findings.
CONCLUSIONS
The prevalence of depressive symptoms among this study's participants supports the findings of other studies that suggest individuals with XXY are at increased risk for depression. The proportion of study participants with clinically significant levels of depressive symptoms was considerable, which raises concern that depression may be an insufficiently addressed complication of XXY. Research shows that depression has a significant negative effect on quality of life,54 is a leading cause of disability,12 and is a major risk factor for suicide.12 Thus, the results of this study emphasize the need for healthcare providers to routinely screen individuals with XXY for depressive symptoms. Simply asking two questions about mood and anhedonia has been found to effectively identify individuals who warrant further evaluation and treatment.12,32 Additional research is needed to understand the clinical correlates of depression among individuals with XXY and to determine whether the manifestations or consequences of depressive symptoms are specific to XXY. Further, intervention trials to determine whether individuals with XXY respond to depression treatment differently than individuals of the general population are warranted. This study identifies important relationships between psychosocial factors and depressive symptoms and highlights opportunities for counseling-based interventions. Developing and testing the feasibility and effectiveness of interventions aimed to facilitate effective coping and adaptation to XXY is an important avenue for future research.
REFERENCES
Ratcliffe S . Long-term outcome in children of sex chromosome abnormalities. Arch Dis Child 1999; 80: 192–195.
DeLisi LE, Maurizio AM, Svetina C, et al. Klinefelter's syndrome (XXY) as a genetic model for psychotic disorders. Am J Med Genet B Neuropsychiatr Genet 2005; 135B: 15–23.
Bender BG, Harmon RJ, Linden MG, Bucher-Bartelson B, Robinson A . Psychosocial competence of unselected young adults with sex chromosome abnormalities. Am J Med Genet 1999; 88: 200–206.
Boks MP, de Vette MH, Sommer IE, et al. Psychiatric morbidity and X-chromosomal origin in a Klinefelter sample. Schizophr Res 2007; 93: 399–402.
Bender BG, Harmon RJ, Linden MG, Robinson A . Psychosocial adaptation of 39 adolescents with sex chromosome abnormalities. Pediatrics 1995; 96: 302–308.
Bruining H, Swaab H, Kas M, van Engeland H . Psychiatric Characteristics in a Self-Selected Sample of Boys With Klinefelter Syndrome. Pediatrics 2009; 123: e865–e870.
Bojesen A, Juul S, Birkebaek NH, Gravholt CH . Morbidity in Klinefelter syndrome: a Danish Register Study based on hospital discharge diagnoses. J Clin Endocrinol Metab 2006; 91: 1254–1260.
Hasin DS, Goodwin RD, Stinson FS, Grant BF . Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on alcoholism and related conditions. Arch Gen Psychiatry 2005; 62: 1097–1106.
Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder. JAMA 2003; 289: 3095–3105.
Kessler RC, Chiu WT, Demler O, Walters EE . Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005; 62: 617–627.
Perala J, Suvisaari J, Saarni SI, et al. Lifetime prevalence of psychotic and bipolar I disorders in a general population. Arch Gen Psychiatry 2007; 64: 19–28.
Force USPST. Screening for depression in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2009; 151: 784–792.
Radloff LS . The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977; 1: 385–401.
Weissman MM, Sholomskas D, Pottenger M . Assessing depressive symptoms in five psychiatric populations: a validation study. Am J Epidemiol 1977; 106: 203–214.
Craig TJ, Vannatta PA . Current medication use and symptoms of depression in a general population. Am J Psychiatry 1978; 135: 1036–1039.
Chwastiak L, Ehde DM, Gibbons LE, Sullivan M, Bowen JD, Kraft GH . Depressive symptoms and severity of illness in multiple sclerosis: epidemiologic study of a large community sample. Am J Psychiatry 2002; 159: 1862–1868.
Pandya R, Metz L, Patten SB . Predictive value of the CES-D in detecting depression among candidates for disease-modifying multiple sclerosis treatment. Psychosomatics 2005; 46: 131–134.
Boyd JH, Weissman MM, Thompson WD, Myers JK . Screening for depression in a community sample: understanding the discrepancies between depression symptom and diagnostic scales. Arch Gen Psychiatry 1982; 39: 1195–1200.
Zich JM, Attkisson CC, Greenfield TK . Screening for depression in primary care clinics: the CES-D and the BDI. Int J Psychiatry Med 1990; 20: 259–277.
Wilson Schaeffer JJ, Gil KM, Burchinal M, et al. Depression, disease severity, and sickle cell disease. J Behav Med 1999; 22: 115–126.
Weinman J, Petrie KJ, MossMorris R, Horne R . The illness perception questionnaire: a new method for assessing the cognitive representation of illness. Psychol Health 1996; 11: 431–445.
Weinman J, Petrie KJ, Moss-Morris R, Horne R . Using and scoring the IPQ-R Subscales. [Website]. Available at: http://www.uib.no/ipq/. Accessed March 3, 2011.
Rybarczyk B, Nyenhuis DL, Nicholas JJ, Cash SM, Kaiser J . Body image, perceived social stigma, and the prediction of psychosocial adjustment to leg amputation. Rehabil Psychol 1995; 40: 95–110.
Vitaliano PP, Russo J, Carr JE, Maiuro RD, Becker J . The ways of coping checklist—revision and psychometric properties. Multivariate Behav Res 1985; 20: 3–26.
Vitaliano PP, Maiuro RD, Russo J, Becker J . Raw versus relative scores in the assessment of coping strategies. J Behav Med 1987; 10: 1–18.
Vitaliano PP, DeWolfe DJ, Maiuro RD, Russo J, Katon W . Appraised changeability of a stressor as a modifier of the relationship between coping and depression: a test of the hypothesis of fit. J Pers Soc Psychol 1990; 59: 582–592.
Hooker K, Frazier LD, Monahan DJ . Personality and coping among caregivers of spouses with dementia. Gerontologist 1994; 34: 386–392.
Zakowski SG, Hall MH, Klein LC, Baum A . Appraised control, coping, and stress in a community sample: a test of the goodness-of-fit hypothesis. Ann Behav Med 2001; 23: 158–165.
Maldonado G, Greenland S . Simulation study of confounder-selection strategies. Am J Epidemiol 1993; 138: 923–936.
Budtz-Jorgensen E, Keiding N, Grandjean P, Weihe P . Confounder selection in environmental epidemiology: assessment of health effects of prenatal mercury exposure. Ann Epidemiol 2007; 17: 27–35.
Cohen J . Statistical power analysis for the behavioral sciences, 3rd ed. Mahwah, New Jersey: Lawrence Erlbaum Associates, Publishers, 2003.
Whooley M, Avins A, Miranda J, Browner W . Case-finding instruments for depression. J Gen Intern Med 1997; 12: 439–445.
van Rijn S, Swaab H, Aleman A, Kahn RS . X Chromosomal effects on social cognitive processing and emotion regulation: a study with Klinefelter men (47,XXY). Schizophr Res 2006; 84: 194–203.
Shen D, Liu D, Liu H, Clasen L, Giedd J, Davatzikos C . Automated morphometric study of brain variation in XXY males. Neuroimage 2004; 23: 648–653.
Vawter MP, Harvey PD, DeLisi LE . Dysregulation of X-linked gene expression in Klinefelter's syndrome and association with verbal cognition. Am J Med Genet B Neuropsychiatr Genet 2007; 144B: 728–734.
van Rijn S, Aleman A, Swaab H, Kahn RS . Neurobiology of emotion and high risk for schizophrenia: role of the amygdala and the X-chromosome. Neurosci Biobehav Rev 2005; 29: 385–397.
Shores MM, Sloan KL, Matsumoto AM, Moceri VM, Felker B, Kivlahan DR . Increased incidence of diagnosed depressive illness in hypogonadal older men. Arch Gen Psychiatry 2004; 61: 162–167.
Almeida OP, Yeap BB, Hankey GJ, Jamrozik K, Flicker L . Low free testosterone concentration as a potentially treatable cause of depressive symptoms in older men. Arch Gen Psychiatry 2008; 65: 283–289.
Seidman SN, Araujo AB, Roose SP, McKinlay JB . Testosterone level, androgen receptor polymorphism, and depressive symptoms in middle-aged men. Biol Psychiatry 2001; 50: 371–376.
Wang C, Swerdloff RS, Iranmanesh A, et al. Transdermal testosterone gel improves sexual function, mood, muscle strength, and body composition parameters in hypogonadal men. J Clin Endocrinol Metab 2000; 85: 2839–2853.
Wang C, Cunningham G, Dobs A, et al. Long-term testosterone gel (AndroGel) treatment maintains beneficial effects on sexual function and mood, lean and fat mass, and bone mineral density in hypogonadal men. J Clin Endocrinol Metab 2004; 89: 2085–2098.
Steidle C, Schwartz S, Jacoby K, Sebree T, Smith T, Bachand R . AA2500 Testosterone gel normalizes androgen levels in aging males with improvements in body composition and sexual function. J Clin Endocrinol Metab 2003; 88: 2673–2681.
Welch JL, Austin JK . Stressors, coping and depression in haemodialysis patients. J Adv Nurs 2001; 33: 200–207.
Peters K, Apse K, Blackford A, McHugh B, Michalic D, Biesecker B . Living with Marfan syndrome: coping with stigma. Clin Genet 2005; 68: 6–14.
Chesney M, Folkman S, Chambers D . Coping effectiveness training for men living with HIV: preliminary findings. Int J STD AIDS 1996; 7( suppl 2): 75–82.
Kennedy P, Duff J, Evans M, Beedie A . Coping effectiveness training reduces depression and anxiety following traumatic spinal cord injuries. Br J Clin Psychol 2003; 42: 41–52.
Stafford L, Berk M, Jackson HJ . Are illness perceptions about coronary artery disease predictive of depression and quality of life outcomes?. J Psychosom Res 2009; 66: 211–220.
Broadbent E, Ellis CJ, Thomas J, Gamble G, Petrie KJ . Can an illness perception intervention reduce illness anxiety in spouses of myocardial infarction patients? A randomized controlled trial. J Psychosom Res 2009; 67: 11–15.
Petrie KJ, Cameron LD, Ellis CJ, Buick D, Weinman J . Changing illness perceptions after myocardial infarction: an early intervention randomized controlled trial. Psychosom Med 2002; 64: 580–586.
Pachankis JE . The psychological implications of concealing a stigma: a cognitive-affective-behavioral model. Psychol Bull 2007; 133: 328–345.
Gollust SE, Thompson RE, Gooding HC, Biesecker BB . Living with achondroplasia in an average-sized world: an assessment of quality of life. Am J Med Genet A 2003; 120A: 447–458.
Loewenstein J, Sutton E, Guidotti R, et al. The art of coping with a craniofacial difference: helping others through “Positive Exposure”. Am J Med Genet A 2008; 146A: 1547–1557.
Webb RE, Daniluk JC . The end of the line. Men Masculinities 1999; 2: 6–25.
Grassi L, Indelli M, Marzola M, et al. Depressive symptoms and quality of life in home-care-assisted cancer patients. J Pain Symptom Manage 1996; 12: 300–307.
Acknowledgements
The research was supported by the Intramural Research Program of the National Human Genome Research Institute. We thank the adolescents and adults with XXY who participated in this study and the XXY support networks for assisting us with study recruitment. We also thank Carolyn Bondy, MD, and Donald Rosenstein, MD, for their feedback on this article and Cristofer Price, PhD, at Abt Associates for his statistical input.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure: The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Turriff, A., Levy, H. & Biesecker, B. Prevalence and psychosocial correlates of depressive symptoms among adolescents and adults with Klinefelter syndrome. Genet Med 13, 966–972 (2011). https://doi.org/10.1097/GIM.0b013e3182227576
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e3182227576
Keywords
This article is cited by
-
The Influence of Parental Migration on Left-behind Children’s Mental Health in China: the Mediating Roles of Daily Stress and Sense-Making
Applied Research in Quality of Life (2022)
-
Quality of life in Klinefelter patients on testosterone replacement therapy compared to healthy controls: an observational study on the impact of psychological distress, personality traits, and coping strategies
Journal of Endocrinological Investigation (2021)
-
Perspectives of adults with Klinefelter syndrome, unaffected adolescent males, and parents of affected children toward diagnosis disclosure: a Thai experience
Journal of Community Genetics (2020)
-
Sex differences in psychiatric disorders: what we can learn from sex chromosome aneuploidies
Neuropsychopharmacology (2019)
-
Gonadotropin-releasing hormone (GnRH) deficiency under treatment: psychological and sexual functioning impacts
Hormones (2018)