Abstract
Purpose
To assess the changes in diabetic retinopathy (DR) in type 2 diabetes (T2DM) patients post bariatric surgery and report on the risk factors that may be associated with it.
Patients and methods
Retrospective observational study of T2DM patients who underwent bariatric surgery in a UK specialist bariatric unit between 2009 and 2015. Preoperative and postoperative weight, HbA1c, and annual DR screening results were collected from medical records. Patients with preoperative retinal screening and at least one postoperative retinal screening were eligible for analysis. Multivariate analysis was used to explore significant clinical predictors on postoperative worsening in DR.
Results
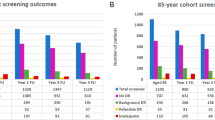
A total of 102 patients were eligible for analysis and were followed up for 4 years. Preoperatively, 68% of patients had no DR compared to 30% with background retinopathy, 1% pre-proliferative retinopathy, and 1% proliferative retinopathy. In the first postoperative visit, 19% of patients developed new DR compared to 70% stable and 11% improved. These proportions remained similar for each postoperative visit over time. Young age, male gender, high preoperative HbA1c, and presence of preoperative retinopathy were the significant predictors of worsening postoperatively.
Conclusion
Bariatric surgery does not prevent progression of DR. Young male patients with pre-existing DR and poor preoperative glycaemic control are most at risk of progression. All diabetic patients should attend regular DR screening post bariatric surgery to allow early detection of potentially sight-threatening changes, particularly among those with identifiable risk factors. Future prospective studies with prolonged follow-up are required to clarify the duration of risk.
Similar content being viewed by others
Introduction
Bariatric surgery is becoming increasingly popular with the rising prevalence of obesity. With up to a quarter of the UK population affected by obesity,1 approximately 6000 bariatric operations are currently performed in the UK each year.2 Increasingly, bariatric surgery has been recognised not only as an effective treatment for achieving substantial sustained weight loss, but also in inducing significant and rapid glycaemic control resulting in remission of type 2 diabetes in approximately 80% of cases within 2 years.3 Therefore, NICE has recommended bariatric surgery as a treatment option for obese patients with type 2 diabetes who are refractory to other weight-loss management options.4 In particular, NICE has recognised the benefit of bariatric surgery for obese patients with recent-onset type 2 diabetes and recommend an expedited assessment to be offered to patients with recent-onset type 2 diabetes even if their body mass index (BMI) is below the usual cut-off criteria.
However, little is known about the effect of bariatric surgery on diabetic microvascular complications such as diabetic retinopathy (DR). As observed during intensification of diabetes management in pregnancy,5 initiation of insulin pumps,6 and after pancreatic transplantation,7 rapid improvement in glycaemic control may cause a paradoxical worsening in DR. Currently there is conflicting evidence on the evolution of DR post bariatric surgery. From case studies8to short-term retrospective studies9, 10, 11, 12, 13 and pilot prospective studies,14, 15, 16 mixed results have been reported. The aim of our study was to provide clarification on the evolution of DR post bariatric surgery and report on the risk factors that may be associated with it.
Subjects and methods
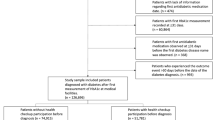
Record retrieval
Under UK guidelines, the analysis was classified as a service evaluation and as such did not require ethical approval. The medical records of all diabetic patients receiving bariatric surgery and diabetes care at the Sunderland Specialist Bariatric Surgery Centre and Sunderland Diabetes Centre from 2009 to 2015 were identified by a prospectively collected electronic database. All patients were assessed by the diabetes team preoperatively and a diagnosis of type 2 diabetes was confirmed. Demographic and clinical details, including age, gender, type of bariatric surgery, and duration of diabetes prior to surgery were extracted from the database for analysis. Immediate preoperative and 1-year postoperative glycated haemoglobin level (HbA1c) and weight were also obtained. Annual DR screening results were extracted from local DR screening service databases. The immediate preoperative DR screening grade and annual DR grades following surgery were recorded using the National Screening Committee (NSC) Diabetic Retinopathy Grading system.
Bariatric surgery provision
Bariatric surgery is offered in the Sunderland Specialist Bariatric Surgery Centre as per NICE guidelines, for patients with a BMI >40 or BMI 35–40 and a serious health condition that could be improved if weight loss is achieved, such as type 2 diabetes and hypertension.4 Furthermore, the patient must fulfil the following criteria: all appropriate non-surgical methods have failed to achieve or maintain a beneficial level of weight loss, the patient has received intensive multidisciplinary team management, the patient agrees to commit to long-term follow-up treatment, and he or she is fit for surgery.4
Three main types of bariatric surgery are offered at Sunderland, all of which are usually performed laparoscopically: gastric banding, sleeve gastrectomy (both based on restriction), and gastric bypass (such as Roux-en-Y gastric bypass, mini loop gastric bypass) which uses a combination of restriction and malabsorption.17 Gastric balloon can be inserted endoscopically, and is often used as an interim option to achieve target weight before laparoscopic surgery.17
DR screening
DR screening in the study area is carried out on all diabetic patients over the age of 12 years by digital photography, with pupillary dilation according to nationally agreed standards.18 Two 45 degree fundal field images are captured: one disc-centred and one fovea-centred. Images are graded as per national guidelines, with an overall retinopathy grade and a maculopathy grade given for each eye. The NSC Diabetic Retinopathy Grading system includes the following: background (R1), pre-proliferative (R2) or proliferative retinopathy (R3); and, maculopathy as no maculopathy (M0) or evidence of maculopathy (M1). R2, R3, and M1 are regarded as referable grades to the hospital eye service and are termed sight-threatening DR.18
Inclusion criteria
All patients with type 2 diabetes who underwent bariatric surgery between 2009–2015, with at least one available preoperative and one postoperative retinal screening result were included.
Patients with no available preoperative or postoperative screening records for analysis were excluded. The Sunderland Bariatric Centre receives referrals from all over the North East region; we had access to the five major local screening service databases—Newcastle, Sunderland, County Durham and Darlington, South Tees,and North Tees, therefore patients who were screened outside these centres were excluded due to inaccessible results.
Statistical analysis
Descriptive and statistical analyses were performed using Minitab 17 version 1.0 (http://www.minitab.co.uk). Continuous variables were presented as median and interquartile range. Categorical variables were presented as frequency and percentage. T-tests were used to compare continuous variables between groups, log transforming to produce approximate normality if necessary. Categorical variables were compared between groups using a Chi-squared test. Statistical significance was considered with a P-value of 0.05 or less.
The retinal screening grades were coded as: R0, R1, R2, R3, M0, and M1. As there were a limited number of patients who had higher grades of DR, R1, R2, and R3 were combined into one category for the purpose of analysis. McNemar’s test was performed to analyse the association between preoperative vs postoperative retinopathy and maculopathy status.
Logistic regression was conducted to examine potential risk factors for the progression of DR at any of the postoperative visits. Both univariate and multivariate models were used to explore the predicted effect of the risk factors. The most important variables were selected using a stepwise procedure. Other variables that did not significantly improve the fit of the models were not included.
Results
Subject characteristics
A total of 203 diabetic patients underwent bariatric surgery during 2009–2015. One-hundred-one patients were excluded due to unavailable preoperative or postoperative DR screening results. Reasons include, patients being screened outside of accessible local programs, and patients failing to attend screening or death. Therefore, a total of 102 patients were eligible for analysis. The characteristics of these patients are summarised in Table 1. The median age was 55 years and the majority were female (67%). The most common surgical procedure undertaken was Roux-en-Y gastric bypass (n=69, 67%), followed by sleeve gastrectomy (n=14, 14%), gastric band (n=12, 12%), mini bypass (n=4, 4%), and gastric balloon (n=3, 3%). The median preoperative HbA1c of our cohort was 61 mmol/mol with a median weight of 123 kg. The median duration of diabetes, defined as the time in years from diagnosis to bariatric procedure, was 6 years in our cohort.
Following bariatric surgery, 86% of patients experienced an improvement in HbA1c. Median preoperative HbA1c was 61 mmol/mol, there was a significant median reduction in HbA1c of 14 mmol/mol (P<0.001) or 26% (P<0.001), resulting in a median postoperative HbA1c of 45 mmol/mol. In our cohort, 42% achieved an HbA1c level <43 mmol/mol—the threshold defined as reversal of diabetes.19, 20 There was no correlation between HbA1c changes (postoperative HbA1c, change in HbA1c, percentage change in HbA1c) and type of bariatric procedure undertaken (P=0.215, 0.324, 0.246 respectively). The median weight postoperatively was 103 kg with a weight loss of 22 kg (18%).
Diabetic retinopathy
Prior to bariatric surgery, 68% of patients had no retinopathy, 30% had background retinopathy, 1% had pre-proliferative retinopathy and 1% had proliferative retinopathy. Ninety-four per cent of patients had no maculopathy preoperatively vs 6% with maculopathy. Three per cent of patients had previous photocoagulation treatment.
The median follow-up was 4 years (interquartile range 2-5 years). Throughout the duration of follow-up, 44% (n=45) of patients with no retinopathy, 25% (n=26) of patients with background retinopathy, and 1% (n=1) with proliferative retinopathy remained stable. At any postoperative visit, 4% (n=4) of patients with background retinopathy experienced an improvement to no retinopathy. Twenty-four per cent (n=24) of patients with no retinopathy experienced a progression to background retinopathy, 1% (n=1) of patients with background retinopathy and 1% (n=1) of patients with pre-proliferative retinopathy progressed to proliferative retinopathy. The overall incidence of new retinopathy was therefore 24% (n=24). The preoperative retinopathy grades vs worst postoperative retinopathy grades detected at any postoperative visit are presented in Table 2.
Regarding the evolution of maculopathy postoperatively, 88% (n=90) of patients with no maculopathy remained stable. Three per cent (n=3) of patients with maculopathy improved to no maculopathy, and 3% (n=3) remained the same. Incidence of new maculopathy was 6% (n=6). In particular, a 46-year-old man who had background retinopathy in one eye and no maculopathy preoperatively, developed bilateral maculopathy requiring treatment within 2 years of undergoing bariatric surgery. This was associated with a rapid reduction in his HbA1c from 112 to 37 mmol/mol within 12 months (Figure 1).
Bilateral colour fundus photographs of a 46-year-old man who developed new bilateral maculopathy 2 years post bariatric surgery despite improved HbA1c from 112 to 37 mmol/mol within 12 months. Top image showing right eye (blue circle indicating presence of intraretinal microvascular abnormalities); bottom image showing left eye.
There was no significant change in the proportion of patients who worsened, remained stable, or improved over the 4 years of follow-up (P=0.91)–see Table 3. In the first postoperative year, 19% (n=18) patients worsened, 70% (n=66) patients were stable, and 11% (n=10) patients improved. In the second year, 14% (n=10) patients worsened, with 10% (n=7) who maintained their deterioration from previous year, 68% (n=49) remained stable, 5% (n=4) improved, with 3% (n=2) maintaining their improvement. In the third year, 16% (n=9) patients worsened, with 9% (n=5) maintaining deterioration, 65% (n=36) remaining stable and 4% (n=2) improved, with 6% (n=3) maintaining improvement. In the fourth year, 7% (n=4) worsened, with 5% (n=3) maintaining deterioration, 80% (n=45) remaining stable and 4% (n=2) improved, with 4% (n=2) maintaining improvement. Overall, the incidence of worsening at any postoperative visit, irrespective of preoperative DR status is 25% (n=26) compared to 71% (n=72) remaining stable and 4% (n=4) experiencing improvement.
Risk factors
Age, gender, preoperative HbA1c, percentage change in HbA1c, and preoperative retinopathy were the significant predictors included in the logistic regression model. Type of bariatric surgery and preoperative weight were not significantly associated with the outcome and therefore not included in the model. Change in weight, percentage change in weight, and duration of diabetes diagnosis were correlated with the main key variables and were not found to be significant after allowance for the other variables in the multiple model. We found, a high preoperative HbA1c was associated with a higher probability of worsening in either eye at any postoperative visit (P<0.001, R2=18.8%). For every 1 mmol/mol increase in preoperative Hba1c level above 53 mmol/mol, the OR of worsening at any postoperative visit was 1.07 (95% CI 1.04, 1.11), P<0.001. A younger age and male gender were also associated with a greater risk of worsening at any follow-up visit (P<0.01; P<0.05 respectively). Features of patients who experienced progression vs those who remained stable or improved over follow-up period are presented in Table 4.
Significant predictors of progression at the first postoperative visit were preoperative HbA1c and age (both P<0.05). For every 1-year increase in age, this was associated with an OR of 0.93 (95% CI 0.88, 0.98), P=0.004. A small percentage change in HbA1c was not positively associated with worsening in the first visit but was for visits after that (P<0.001, R2=21.0%). For every 1% change in postoperative HbA1c, the OR of worsening was 0.96 (95% CI 0.94, 0.99), P<0.001.
Presence of any retinopathy preoperatively (background, pre-proliferative, or proliferative) was associated with a very high probability of either remaining in this category or progressing further during any postoperative visit (P<0.001). A similar trend was also found when analysing the effect of preoperative retinopathy grade on the first postoperative visit result (P=0.07). The presence of existing maculopathy was not associated with increased chance of persisting maculopathy post surgery.
There was no evidence of a change in the proportions of patients who improved, maintained improvement, stable, worsened, and maintained stable over time (P=0.91).
Discussion
The results of our study, one of the largest to date, have shown that bariatric surgery does not guarantee improvement or prevention of DR, despite improved HbA1c in 86% of our patients and 42% achieving normalised HbA1c. The incidence of developing new DR at each postoperative visit ranged from 19-7%, with 10-5% of patients maintaining deterioration from previous screening. While national screening guidelines exist, there is still limited awareness of the potential risk of DR progression postoperatively, including patients achieving non-diabetic HbA1c levels and the need to continue regular screening; two patients within our cohort were discharged from the DR screening service by their General Practitioner after bariatric surgery. Our study clearly shows that patients can continue to develop DR post bariatric surgery, including potentially sight-threatening maculopathy. Therefore, our results support the current UK NHS diabetic eye screening programme recommendations that all patients should be screened annually if there has ever been a definite diagnosis of diabetes, even if they are in remission due to an intervention such as bariatric surgery.21
Our 1-year incidence of 19% of patients worsening was similar to the results described in the literature to date, where a wide range has been reported: 1% (n=63),13 5% (n=56),15 11% (n=56),16 16% (n=318),10 18% (n=38),12 18% (22),11 45% (n=20).14 Kim et al 14 reported the highest rate of progression so far in the literature; 45% in a cohort of 20 patients in a prospective pilot study. Other than the difference in study design, the preoperative HbA1c in their cohort was much higher than our study (81 vs 61 mmol/mol) and a different grading system was used, which may contribute to the difference in results reported. Conversely, Miras et al13 reported a very low rate of 1% in a cohort of 67 patients in a prospective study; however, HbA1c results were not reported and progression was defined as change in at least two steps in a different grading system. Moreover, many of these studies were limited in their small sample size and short follow-up duration which further restricts direct comparisons.
As expected, the presence of any retinopathy preoperatively predicted a high risk of either remaining in this category or progressing further during any postoperative visit. The other major risk factor associated with progression was a higher preoperative HbA1c; every 1 mmol/mol increase in preoperative Hba1c level above 53 mmol/mol was associated with an OR 1.07 (95% CI 1.04, 1.11), P<0.001. This was consistent with previous studies showing poor glycaemic control preoperatively predicted a high risk of progression postoperatively.10 A younger age and male gender were also associated with a greater risk of worsening at any visit.
In regards to predicting acute progression after bariatric surgery, preoperative HbA1c and young age are the significant factors correlating with progression at the first postoperative screening. For every 1-year increase in age, this was associated with OR 0.93 (95% CI 0.88, 0.98), P=0.004. We did not find a large reduction in postoperative HbA1c that was associated with a higher retinopathy grade in follow-up as reported by Murphy et al.10 In fact, our results showed that a small percentage change in HbA1c was not associated with worsening in the first postoperative visit but was associated with worsening in the visits after that. For every 1% change in postoperative HbA1c, the OR of worsening was 0.96 (95% CI 0.94, 0.99), P<0.001. This suggests persistent hyperglycaemia is a predictor for progression and is consistent with large epidemiological studies showing that poor glycaemic control is associated with DR progression over time in a non-bariatric surgical patient cohort.22 Our results suggest that patients with risk factors such as pre-existing DR, young age, male gender, a high preoperative HbA1c, and failure to improve glycaemic control significantly postoperatively need to be closely followed up over time. In particular, young patients with a high preoperative HbA1c may require more intensive monitoring in the first year post surgery to allow early detection of potential acute progression.
The type of bariatric surgery was not found to be associated with any change observed in the level of retinopathy. This may have been due to the lack of any significant correlation between changes in HbA1c and type of bariatric procedure undertaken. Similarly preoperative weight and change in weight postoperatively were also not significantly associated with worsening, having allowed for the key variables, which were similar to other study results9, 13 suggesting that metabolic control may be the main predictor of DR progression postoperatively.
Furthermore, follow-up over 4 years revealed that the proportion of patients experiencing worsening and maintaining deterioration were similar for each postoperative visit. This was in contrast to Murphy et al,10 who reported increasing length of time postoperatively was related to a lower probability of having a retinopathy grade of moderate or above. A potential explanation for this result is the idea of metabolic memory, in which, the impact of hyperglycaemia in patients with type 2 diabetes mellitus before bariatric surgery persists for many years, despite the improvement in glucose metabolism observed post surgery. Our results highlight the importance of continuing DR screening post bariatric surgery for at least 5 years, particularly among those with risk factors for worsening.
We acknowledge that there are several limitations of this study. It was a retrospective study with limited collection of confounding variables, such as blood pressure and nephropathy. A control group could also have strengthened this study, although a well-balanced or randomised design is difficult to achieve in bariatric surgery. It was also not possible to account for any potential preoperative improvement in glycaemic control through medical management and diet restriction in preparation for surgery. However, many centres require a preoperative weight loss,23 and therefore our results extend to these settings. The strength of our study lies in its large cohort size with a prolonged follow-up compared to existing studies. We examined a large number of variables to determine the risk factors for progression. We also used a robust grading scheme, which was quality assured to NSC standards and 92% of our patients had complete data at 1 year of follow-up.
In conclusion, our study has shown that bariatric surgery does not guarantee prevention of DR progression. Young male patients with pre-existing DR, poor preoperative glycaemic control, and who fail to improve HbA1c significantly postoperatively are most at risk of progression. Therefore, based on our results, we recommend that all diabetic patients should attend regular DR screening post bariatric surgery to allow early detection of potentially sight-threatening changes, particularly among those with identifiable risk factors. Future prospective studies with prolonged follow-up is required to further investigate risk factors as well as clarify appropriate screening intervals and duration of screening for patients after bariatric surgery.

References
Health & Social Care Information Centre. Statistics on obesity, physical activity and diet 2016. Available from http://content.digital.nhs.uk/catalogue/PUB20562/obes-phys-acti-diet-eng-2016-rep.pdf. accessed on 10 August 2016.
The United Kingdom National Bariatric Surgery Registry. Bariatric Surgeon Level Outcomes Data Report 2 July 2013 Available from http://www.bomss.org.uk/wp-content/uploads/2014/04/Bariatric-Surgeon-Level-Outcomes-Data-Report-2-July-2013.pdf (accessed 5 August 2016).
Buchwald H, Estok R, Fahrbach K, Banel D, Jensen MD, Pories WJ et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med 2009; 122 (3): 248–256. e5.
National Institute For Health and Clinical Excellence (NICE). Obesity: identification, assessment and management (CG189). 2014. Available from https://www.nice.org.uk/guidance/cg189/resources/obesity-identification-assessment-and-management-pdf-35109821097925. accessed 10 August 2016.
Rasmussen KL, Laugesen CS, Ringholm L, Vestgaard M, Damm P, Mathiesen ER . Progression of diabetic retinopathy during pregnancy in women with type 2 diabetes. Diabetologia 2010; 53 (6): 1076–1083.
Ballegooie EV, Hooymans JMM, Timmerman Z, Reitsma WD, Sluiter WJ, Schweitzer NMJ et al. Rapid deterioration of diabetic retinopathy during treatment with continuous subcutaneous insulin infusion. Diabetes Care 1984; 7 (3): 236–242.
Ramsay RC, Goetz FC, Sutherland DER, Mauer SM, Robison LL, Cantrill HL et al. Progression of diabetic retinopathy after pancreas transplantation for insulin-dependent diabetes mellitus. N Engl J Med 1988; 318 (4): 208–214.
Silva RMJ, Moshfeghi D . Severe worsening of diabetic retinopathy following bariatric surgery. Ophthalmic Surg Lasers Imaging Retina 2013; 44 (6): E11–E14.
Amin AM, Wharton H, Clarke M, Syed A, Dodson P, Tahrani AA . The impact of bariatric surgery on retinopathy in patients with type 2 diabetes: a retrospective cohort study. Surg Obes Relat Dis 2016; 12 (3): 606–612.
Murphy R, Jiang Y, Booth M, Babor R, MacCormick A, Hammodat H et al. Progression of diabetic retinopathy after bariatric surgery. Diabet Med 2015; 32 (9): 1212–1220.
Varadhan L, Humphreys T, Walker AB, Cheruvu CVN, Varughese GI . Bariatric surgery and diabetic retinopathy: a pilot analysis. Obes Surg 2012; 22 (3): 515–516.
Thomas RL, Prior SL, Barry JD, Luzio SD, Eyre N, Caplin S et al. Does bariatric surgery adversely impact on diabetic retinopathy in persons with morbid obesity and type 2 diabetes? A pilot study. J Diabetes Complications 2014; 28 (2): 191–195.
Miras AD, Chuah LL, Lascaratos G, Faruq S, Mohite AA, Shah PR et al. Bariatric surgery does not exacerbate and may be beneficial for the microvascular complications of type 2 diabetes. Diabetes Care 2012; 35 (12): e81.
Kim YJ, Seo DR, Kim MJ, Lee SJ, Hur KY, Choi KS . Clinical course of diabetic retinopathy in Korean type 2 diabetes after bariatric surgery: a pilot study. Retina 2015; 35 (5): 935–943.
Brynskov T, Laugesen CS, Svenningsen AL, Floyd AK, Sørensen TL . Monitoring of diabetic retinopathy in relation to bariatric surgery: a prospective observational study. Obes Surg 2016; 26 (6): 1279–1286.
Miras AD, Chuah LL, Khalil N, Nicotra A, Vusirikala A, Baqai N et al. Type 2 diabetes mellitus and microvascular complications 1 year after Roux-en-Y gastric bypass: a case–control study. Diabetologia 2015; 58 (7): 1443–1447.
Lucchese M, Scopinaro N . Minimally Invasive Bariatric and Metabolic Surgery: Principles and Technical Aspects. Springer International Publishing: Cham, Switzerland, Springer, 2015. pp 145–236.
Public Health England. Diabetic eye screening: programme overview 2014. Available from https://www.gov.uk/guidance/diabetic-eye-screening-programme-overview (accessed 10 August 2016).
Buse JB, Caprio S, Cefalu WT, Ceriello A, Del Prato S, Inzucchi SE et al. How do we define cure of diabetes? Diabetes Care 2009; 32 (11): 2133–2135.
Steven S, Carey PE, Small PK, Taylor R . Reversal of Type 2 diabetes after bariatric surgery is determined by the degree of achieved weight loss in both short- and long-duration diabetes. Diabet Med 2015; 32 (1): 47–53.
UK National Screening Committee. NHS Diabetic Eye Screening Programme - information for healthcare professionals. 2015. Available from http://webarchive.nationalarchives.gov.uk/20150408175925/http://diabeticeye.screening.nhs.uk/primarycare. accessed 10 August 2016.
Stratton MI, Kohner ME, Aldington JS, Turner CR, Holman RR, Manley ES et al. UKPDS 50: risk factors for incidence and progression of retinopathy in type II diabetes over 6 years from diagnosis. Diabetologia 2001; 44 (2): 156–163.
Ochner CN, Dambkowski CL, Yeomans BL, Teixeira J, Xavier Pi-Sunyer F . Pre-bariatric surgery weight loss requirements and the effect of preoperative weight loss on postoperative outcome. Int J Obes (Lond) 2012; 36 (11): 1380–1387.
Acknowledgements
We thank all the staff at the five local DR screening service programs – Newcastle, Sunderland, County Durham and Darlington, South Tees, and North Tees for their assistance with gathering data, in particular Ms Julie Moylan, Mr Saju Thomas, and Ms. Sreekumari Pushpoth.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Chen, Y., Laybourne, J., Sandinha, M. et al. Does bariatric surgery prevent progression of diabetic retinopathy?. Eye 31, 1131–1139 (2017). https://doi.org/10.1038/eye.2017.119
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2017.119
This article is cited by
-
Enhancing glycaemic control with impetus on weight management: Observing for early worsening of diabetic retinopathy
Eye (2024)
-
Bariatric Surgery and Remission of Diabetes Mellitus: the Long and Short in the Context of Diabetic Retinopathy
Obesity Surgery (2024)
-
The Importance of Glycaemic Control Before Bariatric Surgery: Preventing Microvascular and Metabolic Complications
Obesity Surgery (2024)
-
Bariatric surgery—what the ophthalmologist needs to know
Eye (2022)
-
Letter to the Editor Concerning: Adam S. et al. Improvements in Diabetic Neuropathy and Nephropathy After Bariatric Surgery a Prospective Cohort Study
Obesity Surgery (2022)