Abstract
Purpose
To describe the intraretinal microstructure using serial spectral domain optical coherence tomography (SD-OCT) preceding and following pars plana vitrectomy and delamination of fibrovascular membranes in patients with proliferative diabetic retinopathy (PDR).
Methods
This retrospective, interventional case series includes 28 eyes. Outcome measures included LogMAR distance best-corrected visual acuity (BCVA), SD-OCT integrity of photoreceptor inner and outer segments junction (IS/OS), and integrity of external limiting membrane (ELM).
Results
Pre-operative central macular thickness (CMT) was significantly correlated with the final post-operative LogMAR BCVA (Pearson’s coefficient r=0.89; P=0.001). The eyes were categorised into three groups based on post-operative IS/OS integrity (group 0: IS/OS intact; group 1: IS/OS irregular but not completely disrupted; group 2: IS/OS completely disrupted). Mean BCVA improved significantly in group 0 (n=9) from 1.13±0.75 preoperatively to 0.34±0.21 (Student’s t-test: P=0.06), in group 1 (n=10) the BCVA improved from 0.88±0.56 to 0.58±0.31 (Student’s t-test: P=0.053) and in group 2 (n=9) the BCVA improved from 1.64±0.53 to 1.53±0.75 (Student’s t-test: P=0.652).
IS/OS integrity and ELM integrity at 3 months post operatively, were significantly and positively correlated with final BCVA (Pearson’s coefficient: r=0.83, P<0.001 and r=0.72, P<0.001, respectively).
Conclusions
Pre-operative CMT and post-operative disruption of the IS/OS and ELM are useful prognostic indicators in fibrovascular delamination surgery for patients with PDR.
Similar content being viewed by others
Introduction
Optical coherence tomography (OCT) is a well-described method of viewing and measuring various aspects of the retinal architecture in vivo. The amount of detail and information that can be obtained from such images has already been documented extensively.1 In particular, spectral domain OCT (SD-OCT) delineates four highly reflective bands in the outer retina. These are from innermost to outermost: the external limiting membrane (ELM), the photoreceptor inner and outer-segment (IS/OS) junction, the outer-segment tips also referred to as Verhoeff’s membrane and the retinal pigment epithelium (RPE)/Bruch’s/choriocapillaris bands. Spaide and Curcio2 have reviewed the current evidence and report that the anatomical attributions to the middle two hyper-reflective bands remain in question. The innermost two bands, the ELM and the IS/OS junction, are considered to represent important hallmarks of photoreceptor integrity and disruptions of these bands correlate with poor visual acuity in diabetic macular oedema (DMO), resolved central serous chorioretinopathy, branch retinal vein occlusion and post-retinal detachment repair.3, 4, 5, 6, 7, 8
The concept of hierarchy of vulnerability among the ELM, IS/OS and cone outer-segment tips lines has been postulated.9 Thus diseases such as age-related macular degeneration are more likely to affect cone outer-segment tips, as well as the IS/OS junction and in advanced cases the ELM, in contrast to idiopathic epiretinal membrane (ERM) where traction results in disruption further towards the inner retina, leaving the ELM intact and the IS/OS largely unaffected except in advanced cases.9, 10 Thus, despite the fact that diabetic retinopathy (DR) is considered to be an inner retinal disease because of retinal non-perfusion, structural change in the outer retina is observed as epiretinal fibrosis and traction develop. Although the strength and adhesion of the epiretinal membranes is not measurable, surgical experience shows that the strength of the adhesions in proliferative diabetic retinopathy (PDR) membranes is greater than that observed in ERM and also that, subretinal fluid (SRF) may be an important prognostic factor in traction retinal detachment (TRD) secondary to PDR.11, 12, 13 Interestingly, reduced photoreceptor outer-segment thickness also correlates with poor visual function in DMO, indicating that outer retinal structural changes in the absence of traction may be observed in diabetic eyes.14 In one recent study, the integrity of the IS/OS and ELM bands were shown to correlate well with visual acuity following pars plana vitrectomy (PPV) for PDR.15 The study included a significant number of eyes with non-clearing vitreous haemorrhage and pre-macular haemorrhage that may have contributed to worse mean visual acuity levels preoperatively and significantly improved mean levels of vision at last follow-up.15
There is limited pre-operative SD-OCT data in PDR and post-operative SD-OCT data following PPV for complications of PDR. In the present study, we limited our entry criteria to eyes with severe pre-retinal fibrosis, as well as TRD involving or threatening the macula. We described serial SD-OCT scans preceeding and following PPV with pre-retinal membrane delamination and report on the value of imaging the ELM and IS/OS junction in relation to visual recovery. We postulated that the integrity of the IS/OS and ELM post-operatively would correlate with visual outcomes.
Materials and methods
This is a retrospective, consecutive interventional non-comparative case series for patients who underwent PPV and delamination of fibrovascular membranes secondary to PDR between 1st August 2012 and 31st March 2014. All cases were identified through a search of the surgical records database at Whipps Cross University Hospital NHS Trust (Medisoft Ophthalmology, Medisoft Limited, Leeds, UK). We recorded patients demographics, history and clinical examination findings, and reviewed details of the surgical records including per-operative and post-operative complications. The study did not require IRB approval and complied with the tenets of the Declaration of Helsinki. Patients with concurrent macular diseases or patients with significant cataracts or other media opacities reducing the ability to image the retina were excluded.
All eyes underwent logMAR distance visual acuity testing using Thompson’s visual acuity chart (Thompson software solutions, Herts, UK). SD-OCT imaging was obtained at each clinic visit by an OCT-trained technician. SD-OCT scans were performed for each eye using the Cirrus OCT instrument (Carl Zeiss Meditec, Dublin, CA, USA). Visual acuity measurements were recorded at the time of corresponding OCT scans.
Three vitreoretinal-trained masked observers (HZ, ID and LP) agreed on a grading system before the start of the study, which was applied for the analysis of all scans. SD-OCT scans were graded independently. Central macular thickness (CMT) was measured using the automated central 1 mm subfield thickness of the macular cube 512/128 function in which a 6 × 6 mm area is scanned with 128 horizontal lines each consisting of 512 scans per line. If the automatic plane recognition software failed to appropriately identifying the ILM and RPE, then the in-built calliper was utilised. The high definition 5-line raster scans were used for the purpose of identifying the presence of ERM, cystoid macular oedema (CMO), vitreomacular traction (VMT) and integrity of the IS/OS and ELM hyper-reflective bands. CMO, ERM and VMT were graded as present (grade 1) or absent (grade 0). The photoreceptor layer was imaged as a hyper-reflective line showing the IS/OS junction above the retinal pigment epithelium and the next hyper-reflective line on the inner aspect of the IS/OS line being the ELM line.2 The integrity of the IS/OS and ELM were graded as follows: grade 0 was given when an intact hyper-reflective line was found, grade 1 was assigned for any focal disruption of the respective line, and grade 2 was assigned for total disruption of the respective line. The scores and OCT assessments for each grader were recorded independently. OCT scans of poor quality were excluded from the analysis. Where a patient had bilateral delamination surgery, one eye was randomly chosen to remain in the study and the other eye was excluded.
All procedures were performed by two surgeons (HZ and CM) using the Bausch and Lomb Stellaris Vision Enhancement System (Bausch and Lomb, Rochester, NY, USA). No triamcinolone or per-operative dyes were used as part of vitrectomy surgery. Membrane removal was performed using curved and/or vertical vitreoretinal scissors as completely as possible. In no patient, ILM peel was attempted. Panretinal endolaser photocoagulation was performed when this was considered clinically indicated in particular, if insufficient laser had been applied preoperatively or for the management of retinal breaks. This study followed the Tenets of the Declaration of Helsinki. We certify that all applicable institutional and governmental regulations concerning the ethical use of human subjects were followed during this research
Statistical analysis
Interobserver agreement was obtained for grading of OCT scans using the kappa test. Pairs of means were compared using Student’s t-test and groups of means were compared using ANOVA. Correlations were examined using Pearson’s product-moment coefficient (r). A P-value of <0.05 was taken as statistically significant.
Results
Twenty-eight eyes of 28 patients were included in the study. Mean (±SD) duration of follow-up was 11.4 (±5.7) months. Twelve eyes were excluded due to ungradable or unobtainable OCT images, 4 eyes were excluded by random selection in patients with bilateral surgery. Fifteen eyes (54%) had pre-operative OCT scans, 14 eyes had OCT scans at 1–3 months and 27 eyes had OCT scans >3 months post operatively.
OCT results are summarised in Table 1. Of the 28 patients 64% were male, the mean age was 54 (±13) years. The right eye was the study eye in 58% of cases. Age was not significantly correlated with final best-corrected visual acuity (BCVA) (Pearson’s coefficient: r=0.077, P=0.346). The overall inter-observer agreement for the grading of IS/OS and ELM status was 89% (Kappa statistic: 0.709; P<0.01). At final visit 43% (n=12) of patients were pseudophakic and 56% (n=15) were using anti-glaucoma medication in the study eye. Sixty-eight percent of eyes (n=19) had gaseous intraocular tamponade, 18% of cases (n=5) used silicone oil, and 7% (n=2) had silicone oil tamponade at last visit. In addition to PDR, 57% had TRD, 25% had non-clearing vitreous haemorrhage with pre-retinal fibrosis, 11% had combined traction rhegmatogenous retinal detachment, and 7% had taught thickened posterior hyaloid.
In the 16 patients with pre-operative scans, the pre-operative CMT was shown to be significantly correlated with the final post-operative logMAR BCVA (Pearson’s correlation r=0.89; P=0.001; Table 1 and Figure 1). Two other pre-operative factors that were moderately correlated with final logMAR BCVA, SRF, and pre-operative logMAR BCVA, had correlation coefficients of 0.69 (P=0.03) and 0.50 (P=0.49), respectively (Table 1).
Scatter plot of pre-operative CMT (in microns; x axis) against final post-operative logMAR BCVA (y axis). The best-fit line and Pearson correlation coefficient (r=0.89) are depicted, along with the 95% confidence belt (broken lines, shaded area). This strong correlation was positive and significant (P=0.001).
For all 28 eyes, the mean pre-operative logMAR BCVA improved significantly from 1.24 (±0.64) to 0.81 (±0.77, P=0.006) at last post-operative visit. Fifty-four percent (n=15) of patients experienced a final post-operative improvement in BCVA equivalent to ≥3 lines on the ETDRS (Early Treatment of Diabetic Retinopathy Study) chart, whereas 14% of patients (n=4) experienced a deterioration of ≥3 ETDRS lines. Three of these four patients had pre-operative OCT scans and all (3/3) had ELM and ISOS grades of 2, which was a significantly worse mean grade than the other 13 patients with pre-operative scans (unpaired Student’s t-test: P=0.003 and P=0.006, respectively). All four patients with loss of ≥3 ETDRS lines had post-operative ELM and ISOS grades of 2.
In Table 2 and Figure 2, the eyes were divided into three groups based on post-operative IS/OS integrity. Mean BCVA improved significantly in group 0 (n=9) from 1.13±0.75 preoperatively to 0.34±0.21 (P=0.06; Figure 3), in group 1 (n=10) the BCVA improved from 0.88±0.56 to 0.58±0.31 (P=0.053) and in group 2 (n=9) the BCVA improved from 1.64±0.53 to 1.53±0.75 (P=0.652).
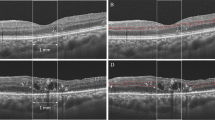
(a) A high definition pre-operative macular OCT scan and (b) the same patient 12 months following PPV and delamination surgery. The patient was a 55-year old with type 2 diabetes managed with insulin. The pre-operative OCT (a) displays a thickened taut posterior hyaloid, with cystoid macular oedema, a focally disrupted IS/OS=1 and ELM=1. The BCVA was 0.8 and the CMT was 450 microns. The post-operative scan (b) 10-months post PPV and delamination surgery. The BCVA improved to 0.54 and the CMT has reduced to 271 microns, the ELM was complete (ELM=0) and the IS/OS was focally disrupted but not completely disrupted (IS/OS=1).
Box-whisker plot depicting the BCVA for patients grouped by (a) IS/OS and (b) external limiting membrane integrity (group 0: IS/OS or ELM intact; group 1: IS/OS or ELM irregular but not completely disrupted; group 2: IS/OS or ELM completely disrupted), before (pre-operative) and after (post-operative) delamination of fibrovascular membranes in proliferative diabetic retinopathy.
Eyes were also categorised in three subgroups based on the integrity of the ELM. The mean BCVA improved significantly in group 0 (from 1.10±0.71 to 0.36±0.22; P=0.008; Figure 3b) and group 1 (from 1.03±0.56 to 0.54±0.23; P=0.016). Group 2 remained unchanged with a mean pre-operative BCVA of 1.71±0.51 and a mean post-operative BCVA of 1.70±0.88 (P=0.974).
Discussion
Conventional theory explains that poor visual outcomes following surgical treatment of PDR are the result of macular ischaemia or long standing TRD of the macula. Our data support the importance of intraretinal structural changes at the level of the ELM and IS/OS junction in eyes with severe PDR. As far as we know, this is the first study to examine pre-operative as well as post-operative SD-OCT images in the context of PPV for PDR.
The ELM and IS/OS junction findings at 3 months were the most strongly correlated findings with final logMAR BCVA, better than the ELM and IS/OS junction findings at final visit. We postulate that this effect of falling correlation may be due to other confounding issues such as cataract formation. It is noteworthy that ERM was present post-operatively in the majority of patients at the 3-month and final visits. The presence of ERM at 3 months was significantly correlated with a worse final BCVA, but this association was lost at final visit. Furthermore, post-operative CMT is not significantly correlated with final BCVA, whereas it was strongly and significantly correlated when measured preoperatively.
Our results show that BCVA and SD-OCT parameters assessed at 3 months post operatively were most strongly correlated with the final BCVA, indicating that good surgical outcomes at 3 months were usually maintained at last follow-up.
We speculate that the photoreceptor injury was beyond repair in eyes with disrupted IS/OS junction and/or ELM, leading to poor visual outcomes. We believe that the IS/OS and the ELM integrity may act as a surrogate of photoreceptor integrity and function in the present setting.
The IS/OS group 0 (based on final OCT scans) showed a significant final post-operative improvement in mean BCVA, which was also the case for the ELM groups 0 and 1. This finding supports the hypothesis that IS/OS and ELM integrity have an important role in maintaining macular function and that the disruption of these structures is associated with poorer post-operative outcomes. It would seem that minimal disruption of the IS/OS and ELM are desirable for a favourable BCVA post membrane delamination for PDR. A poor ELM and IS/OS grade preoperatively confers a greater likelihood of a poorer post-operative BCVA.
Shah et al examined post-operative outer-segment OCT changes in PDR. They reported a correlation with post-operative ELM, IS/OS integrity and final BCVA (52 and 55%, respectively), which is less than that of our study. This difference may be attributed to differing patient baseline characteristics as 17 of 36 (47%) patients in Shah’s paper had tractional macular detachments and cases with persistent ERM were excluded.15 All our patients had pre-retinal fibrosis with an element of traction requiring membrane delamination, furthermore eyes with post-operative ERM were not excluded. Baseline demographics were also slightly different as 85% of our patients suffered from type 2 DM and 70% were on insulin, compared with 89% (31/36) on insulin in the study reported by Shah et al.15
In only 15 of the 28 eyes were pre-operative scans available for analysis. This is due to the presence of concomitant VH and advanced macular detachment, which prevented quality scanning in the remaining 13 patients. Despite this limitation we have found three pre-operative factors (pre-operative BCVA, pre-operative CMT and presence of SRF preoperatively) that are significantly correlated with final BCVA.
Pre-operative and post-operative CMO, defined in this study as any cystoid spaces seen on the high definition SD-OCT images, does not correlate with final BCVA and neither does pre-operative VMT correlate with final BCVA. Our findings would suggest that intraretinal structural changes are the predominant predictive parameter of post-operative visual function and that the relative contribution of other findings such as VMT and CMO to have less relative contribution to final visual function. Eyes with PDR undergoing PPV for TRD have usually suffered from significant intraretinal structural change and have reduced visual potential, unlike those with DMO where a reduction in macular thickness and oedema may be more likely to result in a significant improvement in vision.
Study limitations include its retrospective design, small numbers, lack of randomisation, and the absence of a control group. Some of these limitations may be difficult to address, however, the advent of diabetic retinopathy screening services has resulted in a reduction in the progression to advanced stages of diabetic eye disease.16 Further research is needed to prevent the development of advanced stages of retinopathy and until this is possible, retinal traction-associated complications will continue to be managed surgically in the majority of eyes. Developments such as intraoperative OCT may yield further insight into the contribution of the IS/OS and ELM status on visual outcomes. Some patients were still phakic (55%) and had silicone oil filled eyes (7%) at last follow-up, this may have altered their BCVA, however we felt their inclusion caused less bias than their exclusion.
In summary, we report a significant correlation between pre-operative CMT, presence of SRF and pre-operative BCVA with final LogMAR BCVA. We also confirm the importance of the post-operative IS/OS and ELM status as prognostic factors following diabetic vitrectomy for complications of PDR. Ocular findings at 3 months appear to remain relatively stable at final follow-up. High-resolution SD-OCT should be an integral part of the post-operative management of diabetic vitrectomy.

References
Drexler W, Fujimoto JG . State-of-the-art retinal optical coherence tomography. Prog Retin Eye Res 2008; 27: 45–88.
Spaide RF, Curcio CA . Anatomical correlates to the bands seen in the outer retina by optical coherence tomography: literature review and model. Retina 2011; 31: 1609–1619.
Otani T, Yamaguchi Y, Kishi S . Correlation between visual acuity and foveal microstructural changes in diabetic macular edema. Retina 2010; 30: 774–780.
Maheshwary AS, Oster SF, Yuson RM, Cheng L, Mojana F, Freeman WR . The association between percent disruption of the photoreceptor inner segment-outer segment junction and visual acuity in diabetic macular edema. Am J Ophthalmol 2010; 150: 63–7 e1.
Eandi CM, Chung JE, Cardillo-Piccolino F, Spaide RF . Optical coherence tomography in unilateral resolved central serous chorioretinopathy. Retina 2005; 25: 417–421.
Murakami T, Tsujikawa A, Ohta M, Miyamoto K, Kita M, Watanabe D et al. Photoreceptor status after resolved macular edema in branch retinal vein occlusion treated with tissue plasminogen activator. Am J Ophthalmol 2007; 143: 171–173.
Schocket LS, Witkin AJ, Fujimoto JG, Ko TH, Schuman JS, Rogers AH et al. Ultrahigh-resolution optical coherence tomography in patients with decreased visual acuity after retinal detachment repair. Ophthalmology 2006; 113: 666–672.
Sakamoto A, Nishijima K, Kita M, Oh H, Tsujikawa A, Yoshimura N . Association between foveal photoreceptor status and visual acuity after resolution of diabetic macular edema by pars plana vitrectomy. Graefes Arch Clin Exp Ophthalmol 2009; 247: 1325–1330.
Shimozono M, Oishi A, Hata M, Matsuki T, Ito S, Ishida K et al. The significance of cone outer segment tips as a prognostic factor in epiretinal membrane surgery. Am J Ophthalmol 2012; 153: 698–704, e1.
Oishi A, Hata M, Shimozono M, Mandai M, Nishida A, Kurimoto Y . The significance of external limiting membrane status for visual acuity in age-related macular degeneration. Am J ophthalmol 2010; 150: 27–32 e1.
Kay CN, Gendy MG, Lujan BJ, Punjabi OS, Gregori G, Flynn HW Jr . Composite spectral domain optical coherence tomography images of diabetic tractional retinal detachment. Ophthalmic Surg Lasers Imaging 2008; 39: S99–103.
Iwasaki T, Miura M, Matsushima C, Yamanari M, Makita S, Yasuno Y . Three-dimensional optical coherence tomography of proliferative diabetic retinopathy. Br J Ophthalmol 2008; 92: 713.
Barzideh N, Johnson TM . Subfoveal fluid resolves slowly after pars plana vitrectomy for tractional retinal detachment secondary to proliferative diabetic retinopathy. Retina 2007; 27: 740–743.
Forooghian F, Stetson PF, Meyer SA, Chew EY, Wong WT, Cukras C et al. Relationship between photoreceptor outer segment length and visual acuity in diabetic macular edema. Retina 2010; 30: 63–70.
Shah VA, Brown JS, Mahmoud TH . Correlation of outer retinal microstucture and foveal thickness with visual acuity after pars plana vitrectomy for complications of proliferative diabetic retinopathy. Retina 2012; 32: 1775–1780.
Garvican L, Clowes J, Gillow T . Preservation of sight in diabetes: developing a national risk reduction programme. Diabet Med 2000; 17: 627–634.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Presentation: The paper was presented at the EVER meeting in Nice, October 2014
Rights and permissions
About this article
Cite this article
Dooley, I., Laviers, H., Papavasileiou, E. et al. Spectral domain ocular coherence tomography findings pre- and post vitrectomy with fibrovascular membrane delamination for proliferative diabetic retinopathy. Eye 30, 34–39 (2016). https://doi.org/10.1038/eye.2015.178
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2015.178
This article is cited by
-
Persistent subretinal fluid following diabetic tractional retinal detachment repair: risk factors, natural history, and management outcomes
International Ophthalmology (2021)
-
An optical coherence tomography study of residual subfoveal fluid after successful pars plana vitrectomy in patients with diabetic tractional macular detachment
Eye (2018)