Abstract
Purpose
The study aims to identify the association between the baseline retinal vascular calibre and visual outcome of patients with diabetic macular oedema (DMO) treated with intravitreal ranibizumab.
Methods
The 1-M field (as defined in the ETDRS study) of the digital colour fundus photographs of DMO patients who had been treated primarily with ranibizumab in a clinical trial was assessed. Of the 84 patients, 25 had gradable retinal photographs that could be subjected to analyses by the Interactive Vessel Analysis (IVAN) software at baseline. The average retinal vascular calibre of the six largest venules (CRVE) and the six largest arterioles (CRAE) in the peripapillary area (0.5 and 1 disc diameter from the optic disc margin) was measured. The relationship between CRVE and CRAE at baseline and the change in visual acuity at month 12 was assessed using the Mann–Whitney U test.
Results
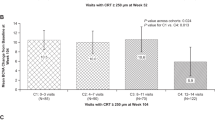
Ten eyes from 10 patients who had shown an improvement of ≥2 lines of best corrected visual acuity (BCVA) at month 12 had a wider baseline CRVE (248.3±24.5 μm) compared with the 15 eyes from 15 patients who did not show the improvement of ≥2 lines (226.6±44.8 μm, P<0.05). The baseline CRAE did not differ significantly in these patients (156.1±22.7 vs 142±17.5 μm, P=0.17).
Conclusions
A wider baseline retinal venular calibre may be a predictor of better visual outcome in DMO eyes treated with ranibizumab. Further prospective studies with a larger sample size and a broader range of disease severity and visual acuity are needed to confirm this finding.
Similar content being viewed by others
Introduction
Changes in retinal vascular calibre (broadening or narrowing) have been considered a risk factor for the development of various systemic diseases in several large population-based studies including the Beaver Dam Eye Study, the Blue Mountain Eye study, and the Wisconsin Epidemiologic Study of Diabetic Retinopathy.1, 2, 3, 4 Furthermore, wider retinal venular calibre has been regarded as an independent risk factor for the subsequent incidence and progression of diabetic retinopathy (DR).5
The discovery of anti-vascular endothelial growth factor (anti-VEGF) therapy has considerably transformed the management and treatment of diabetic macular oedema (DMO). Ranibizumab (Lucentis, Genentech, San Francisco, CA, USA) (RBZ), an anti-VEGF agent, is a recombinant, humanised monoclonal antibody fragment that binds to all isoforms of VEGF-A, which is a critical stimulus in the pathogenesis of DMO.6 The RISE and RIDE studies demonstrated that ranibizumab is an effective treatment for DMO. The RISE study showed that 44.8% of patients receiving 0.3 mg RBZ and 39.2% of patients receiving 0.5 mg RBZ gained ≥15 letters, while the RIDE study demonstrated that the matching proportions were 33.6% and 45.7%, respectively.7 The factors that predict the treatment response to RBZ in DMO patients are currently not apparent to clinicians and scientists. Bressler et al recently evaluated 361 eyes that were randomly assigned to intravitreal RBZ with prompt or deferred laser treatment within a trial of RBZ, triamcinolone acetonide, and laser treatment for centre-involved DMO. The study was done to identify factors that predict the success or failure of treatment with intravitreal RBZ. The authors have demonstrated that younger age, milder DR on clinical examination, the absence of surface-wrinkling retinopathy, and the reduction in central subfield thickness during the first treatment year better predicted visual acuity outcomes.8
Furthermore, studies have demonstrated that diabetic patients have a wider retinal arteriolar calibre4 and these patients have a greater chance of developing incident retinopathy. Therefore, changes in retinal vascular calibre are considered to be a potential subclinical marker of DR.9 The Blue Mountains Eye Study also revealed that the severity of DR is associated with widening of the retinal venular calibre.4 Klein et al5 have confirmed this finding in a recently published study. They concluded that increase in the retinal venular calibre, but not the arteriolar calibre, was independently associated with the occurrence and advancement of DR.
Several studies have evaluated the association between intravitreal treatments and retinal vascular calibres. Wickremasinghe et al,10 using Interactive Vessel Analysis (IVAN) software, demonstrated that intravitreal triamcinolone acetate has a significant narrowing effect on both retinal arteriolar and venular calibres after a single injection over a 3-month time period. This study also demonstrated that there was no change in retinal arteriolar or venular calibres in those who were treated with sham injections. Additionally, Tatlipinar et al11 assessed eight DMO patients treated with intravitreal injections of 1.25 mg bevacizumab over a period of 1 month. They had reported that there would be a trend towards vasoconstriction in arterioles and venules at day 7, but this difference did not reach statistical significance (P>0.05). Further, Wickremasinghe et al's12 findings demonstrated a potential association between wider baseline venular calibre and a worst response in eyes with neovascular age-related macular degeneration (AMD) treated with RBZ.
Therefore, the measurement of retinal vascular calibre may potentially prove to be an anatomical indicator of underlying disease severity in patients with DMO and may also provide the scientific community with a better understanding of the factors that determine visual outcome in patients needing anti-VEGF treatment.
Materials and methods
Study population
This study was based on data from the READ-2 study, which was a phase II randomised multicentre clinical trial designed to evaluate the safety and efficacy of intravitreal RBZ in patients with DMO. The study protocol and primary outcomes have been reported.13, 14 The READ-2 study subjects whose data were included in this vessel calibre analysis included those who had been treated primarily with RBZ alone or in combination with laser and had gradable retinal photographs at baseline.
Measurement of retinal vascular calibre
Optic disc-centred digital colour fundus photographs (field 1) of DMO patients were assessed at baseline.15 All photographs were taken prior to the first treatment with RBZ or laser plus RBZ in the READ-2 Study. The retinal vascular calibre was measured using the computer program IVAN version 1.30 (University of Wisconsin, Madison, WI, USA) according to a detailed protocol that has been described by Hubbard and Wong.16, 17 All vessels coursing through an area one-half to one-disc diameter from the optic disc margin (double arrow in Figure 1) were measured. The mean vessel calibre of the largest six arteries was termed central retinal artery equivalent (CRAE) while that of the largest six venules was coined central retinal vein equivalent (CRVE) using formulas developed by Hubbard et al16 and later modified by Knudtson et al.18
An optic disc-centred digital colour fundus photograph of the right optic nerve head of a DMO patient. All vessels coursing through an area one-half to one-disc diameter from the optic disc margin (double arrow) were measured and the largest six were termed central retinal artery equivalent (CRAE) and central retinal vein equivalent (CRVE).
Main outcome measures
In the READ-2 Study, best-corrected visual acuity (BCVA) was measured using the ETDRS charts. Optical coherence tomography (OCT) was obtained by experienced technicians who were using the fast macular scan protocol (Stratus OCT Carl Zeiss Meditec, Dublin, CA, USA) at baseline; no spectral domain OCT was available at the time the READ-2 was conducted. Primary outcome measures included changes in visual acuity and central macular thickness (CMT) at month 12 compared to baseline. In addition, demographics (age, gender, race, and ethnicity), HbA1c level, and mean arterial blood pressure (MAP) were collected and correlated to outcome measurements.
Statistical analysis
In this vessel calibre analysis, improvement in visual acuity at month 12 was defined as a ≥10 letter gain in vision after the initiation of RBZ or RBZ plus laser treatment for DMO. The association between baseline CRVE and CRAE and the change in BCVA and CMT at month 12 was assessed using the Mann–Whitney U test.
This study was conducted with the approval of Johns Hopkins University School of Medicine Institutional Review Board and in accordance with the principles of the Declaration of Helsinki.
Results
In this analysis, 25 patients (25 eyes; male: 15, female: 10, mean age: 61.9 years (SD 9.1)) had baseline photographs that were gradable by IVAN software. The visual acuity information was collected for these patients at baseline and month 12. Table 1 shows the demographics, mean HbA1c level, mean MAP, and the treatment group assignment at baseline, as well as the association between the characteristics and visual outcome of the eyes at month 12. Group 1 (G1) includes 10 eyes of 10 patients who showed visual improvement that was ≥2 lines over the study period. These patients have been classified as demonstrating improved visual acuity. Group 2 (G2) includes 15 eyes of 15 patients with <2—line vision gain or a decrease in visual acuity when compared to the baseline.
Anatomical (CRVE, CRAE) and functional (BCVA) characteristics of the eyes in this study and their correlations with visual outcome after 12 months have been summarised in Table 2. Race, sex, and baseline CRVE were significantly different in both groups (P<0.05). Marginal correlations were demonstrated when baseline mean MAP and mean HbA1c were compared (P<0.10).
The eyes that showed improvement in this study also had a wider baseline venular calibre (CRVE=248.3±24.5 μm) when compared with the eyes that did not show significant improvement (CRVE=226.6±44.8 μm) (P<0.05). On the other hand, the baseline arteriolar calibre did not demonstrate a significant correlation with visual outcome, since there was no significant difference between the two groups (CRAE: 156.1±22.7 vs 142±17.5 μm, P=0.17). The mean BCVA at baseline has no significant difference in G1 and G2 (26.5 vs 25.6 letters, P=0.7), and thus it did not correlate with visual outcomes at month 12 (The mean number (SD) of RBZ injections was 5.12±1.91 and no significant difference in treatment frequency between the two groups was appreciated (4.88±2.02 vs 5.26±1.90, P>0.5)). There was no significant difference between the mean number of injections of RBZ in the group that gained ≥10 letters and the group with<10 letters (4.88±2.02 vs 5.26±1.90, P>0.5).
Discussion
The index study is among the first to analyse and find a correlation between retinal vessel calibre and visual outcome in patients with DMO. Our study has demonstrated that eyes that showed moderate improvement (≥10 ETDRS letters) had a wider baseline venular calibre when compared to eyes that did not show moderate improvement. A wider baseline CRVE was significantly correlated with vision improvement, while a wider baseline CRAE was not. As Klein et al5 have suggested that CRVE can be used to predict DR progression, it is possible that retina specialists may use CRVE to predict visual improvement in patients with DMO treated with RBZ.
Klein et al evaluated the correlation of change in retinal vascular calibre to the subsequent 6-year incidence and progression of DR and incidence of proliferative diabetic retinopathy (PDR) and macular oedema in patients with diabetes mellitus. Their results showed that widening of the retinal venular, but not arteriolar, calibre was associated with subsequent incidence and progression of DR, independent of the DR severity level, glycemic control, and other factors. They believe the CRVE may provide additional information about the risk of incidence and progression of DR beyond traditional risk factors.5
In a recently published study, Tatlipinar et al11 evaluated the short-term effects of a single intravitreal bevacizumab injection on the retinal vascular calibres in patients with DMO. There appeared to be a trend towards vasoconstriction, but did not reach statistical significance. The results suggested that intravitreal injection of bevacizumab might induce retinal vasoconstriction. However, the small number of subjects might have prevented the difference from reaching statistical significance. In our study of patients receiving treatments with RBZ the results have demonstrated that patients with a wider CRVE at baseline exhibited greater improvement in visual acuity at 12 months. CRVE may thus be considered as an indirect marker and indicator of how an eye with DMO may respond to anti-VEGF therapies such as RBZ. Perhaps, the intraocular level of VEGF may correlate with CRVE.
Furthermore, Sacu et al19 investigated the effect of intravitreal ranibizumab (0.5 mg) on retinal vascular calibres and retrobulbar blood velocities in patients with acute branch retinal vein occlusion (BRVO). Their study using retinal vessel analyser (RVA) showed significant vasoconstriction in retinal veins and arteries of the affected eye as well as a reduction in flow velocities in the eyes with BRVO. However, it appeared that the reduction in retinal vascular calibres and flow velocities did not correlate with change in visual acuity or number of re-treatments. Additionally, they found that there was no correlation between the degree of vasoconstriction and visual outcome when RBZ was used, while there was a correlation when laser treatment was used. Our study showed that there was a statistically significant relationship between baseline CRVE and visual acuity.
Wickremasinghe et al12 using IVAN software evaluated patients with neovascular AMD treated with intravitreal RBZ and showed that wider baseline CRVE significantly correlated with poor visual outcome after 12 months. Our study in DMO demonstrated contradictory findings, suggesting the difference in pathophysiology and oxygenation effect of the two diseases, even though both neovascular AMD and DMO appear to be driven by VEGF. However, it does suggest that baseline CRVE may be considered as a predictor of visual acuity in patients with macular diseases treated with RBZ.
Several studies have employed the IVAN software to measure the retinal vascular calibres in different diseases and its association with the progression of ocular or systemic diseases. No study employing IVAN to evaluate the relationship between baseline retinal vascular diameters and response to RBZ in DMO patients has been reported. Although our pilot study employed the IVAN software to measure and analyse effectively the average retinal vascular calibres of the CRVE and the CRAE, and to show evidence that there is a potential correlation between baseline CRVE, but not CRAE, and visual outcomes, there are several limitations. First, the sample size is too small to generalise our results. Second, there may be limited generalisability of our findings to the general population, as our study population was derived from a multicentre clinical trial, where study subjects were carefully selected to meet the study criteria. Further, there may be inherent biases among the 25 fundus photographs of sufficient quality to be evaluated by IVAN software in this analysis. Applying similar analyses to a larger number of DMO eyes may yield different outcomes. Additionally, other associated factors such as cigarette smoking, diet, and body mass index (BMI) were not considered in this study using the READ-2 data. Finally, there might be measurement errors in the retinal vascular diameters measurement, given the limitations of the IVAN computer software when applied to retinal images of insufficient quality. Further studies with a greater number of DMO eyes managed with RBZ or other VEGF antagonists and a broader range of disease severity and visual acuity are needed to confirm our initial findings.

References
Klein R, Klein BE, Moss SE, Wong TY, Hubbard L, Cruickshanks KJ et al. The relation of retinal vessel caliber to the incidence and progression of diabetic retinopathy: XIX: the Wisconsin Epidemiologic Study of Diabetic Retinopathy. Arch Ophthalmol 2004; 122 (1): 76–83.
Klein R, Klein BE, Knudtson MD, Wong TY, Tsai MY . Are inflammatory factors related to retinal vessel caliber? The Beaver Dam Eye Study. Arch Ophthalmol 2006; 124 (1): 87–94.
Klein R, Klein BE, Moss SE, Wong TY . Retinal vessel caliber and microvascular and macrovascular disease in type 2 diabetes: XXI: the Wisconsin Epidemiologic Study of Diabetic Retinopathy. Ophthalmology 2007; 114 (10): 1884–1892.
Kifley A, Wang JJ, Cugati S, Wong TY, Mitchell P . Retinal vascular caliber and the long-term risk of diabetes and impaired fasting glucose: the Blue Mountains Eye Study. Microcirculation 2008; 15 (5): 373–377.
Klein R, Myers CE, Lee KE, Gangnon R, Klein BEK . Changes in retinal vessel diameter and incidence and progression of diabetic retinopathy. Arch Ophthalmol 2012; 130 (6): 749–755.
Nguyen QD, Tatlipinar S, Shah SM, Haller JA, Quinlan E, Sung J et al. Vascular endothelial growth factor is a critical stimulus for diabetic macular edema. Am J Ophthalmol 2006; 142 (6): 961–969.
Nguyen QD, Brown DM, Marcus DM, Boyer DS, Patel S, Feiner L et al. Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology 2012; 119 (4): 789–801.
Bressler SB, Qin H, Beck RW, Chalam KV, Kim JE, Melia M et al. Factors associated with changes in visual acuity and central subfield thickness at 1 year after treatment for diabetic macular edema with ranibizumab. Arch Ophthalmol 2012; 130 (9): 1153–1161.
Rogers SL, Tikellis G, Cheung N, Tapp R, Shaw J, Zimmet PZ et al. Retinal arteriolar caliber predicts incident retinopathy: the Australian Diabetes, Obesity and Lifestyle (AusDiab) study. Diabetes Care 2008; 31 (4): 761–763.
Wickremasinghe SS, Rogers SL, Gillies MC, Zhu M, Wong TY . Retinal vascular caliber changes after intravitreal triamcinolone treatment for diabetic macular edema. Invest Ophthalmol Vis Sci 2008; 49 (11): 4707–4711.
Tatlipinar S, Dinç UA, Yenerel NM, Görgün E . Short-term effects of a single intravitreal bevacizumab injection on retinal vessel calibre. Clin Exp Optom 2012; 95 (1): 94–98.
Wickremasinghe SS, Busija L, Guymer RH, Wong TY, Qureshi S . Retinal venular caliber predicts visual outcome after intravitreal ranibizumab injection treatments for neovascular AMD. Invest Ophthalmol Vis Sci 2012; 53 (1): 37–41.
Nguyen QD, Shah SM, Khwaja AA, Channa R, Hatef E, Do DV et al. Two-year outcomes of the ranibizumab for edema of the mAcula in diabetes (READ-2) study. Ophthalmology 2010; 117 (11): 2146–2151.
Nguyen QD, Shah SM, Heier JS, Do DV, Lim J, Boyer D et al. Primary end point (six months) results of the Ranibizumab for Edema of the mAcula in diabetes (READ-2) study. Ophthalmology 2009; 116 (11): 2175–2181.
Early Treatment Diabetic Retinopathy Study Research Group. Grading diabetic retinopathy from stereoscopic color fundus photographs—an extension of the modified Airlie House classification. ETDRS report number 10. Ophthalmology 1991; 98 (5 Suppl): 786–806.
Hubbard LD, Brothers RJ, King WN, Clegg LX, Klein R, Cooper LS et al. Methods for evaluation of retinal microvascular abnormalities associated with hypertension/sclerosis in the Atherosclerosis Risk in Communities Study. Ophthalmology 1999; 106 (12): 2269–2280.
Wong TY, Knudtson MD, Klein R, Klein BE, Meuer SM, Hubbard LD . Computer-assisted measurement of retinal vessel diameters in the Beaver Dam Eye Study: methodology, correlation between eyes, and effect of refractive errors. Ophthalmology 2004; 111 (6): 1183–1190.
Knudtson MD, Lee KE, Hubbard LD, Wong TY, Klein R, Klein BE . Revised formulas for summarizing retinal vessel diameters. Curr Eye Res 2003; 27 (3): 143–149.
Sacu S, Pemp B, Weigert G, Matt G, Garhofer G, Pruente C et al. Response of retinal vessels and retrobulbar hemodynamics to intravitreal anti-VEGF treatment in eyes with branch retinal vein occlusion. Invest Ophthalmol Vis Sci 2011; 52 (6): 3046–3050.
Acknowledgements
The authors would like to acknowledge Dr Ron Klein and his staff at the University of Wisconsin for their assistance with the software program.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
Dr Nguyen serves on the Steering Committees for the studies of ranibizumab and aflibercept for retinal vascular diseases sponsored by Genentech and Regeneron. Dr Do serves on the Steering Committee for the studies of aflibercept in diabetic macular oedema sponsored by Regeneron. The READ-2 Study was supported by the Juvenile Diabetes Research Foundation.
Additional information
The primary findings of this work have been presented at the Association for Research in Vision and Ophthalmology (ARVO) 2013 Annual Meeting, Seattle, WA, USA.
Rights and permissions
About this article
Cite this article
Moradi, A., Sepah, Y., Ibrahim, M. et al. Association of retinal vessel calibre and visual outcome in eyes with diabetic macular oedema treated with ranibizumab. Eye 28, 1315–1320 (2014). https://doi.org/10.1038/eye.2014.186
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2014.186