Abstract
Most children with glaucoma will require surgery in their lifetime, often in their childhood years. The surgical management of childhood glaucoma is however challenging, largely because of its greater potential for failure and complications as compared with surgery in adults. The available surgical repertoire for childhood glaucoma has remained relatively unchanged for many years with most progress owing to modifications to existing surgery. Although the surgical approach to childhood glaucoma varies around the world, angle surgery remains the preferred initial surgery for primary congenital glaucoma and a major advance has been the concept of incising the whole of the angle (circumferential trabeculotomy). Simple modifications to the trabeculectomy technique have been shown to considerably minimise complications. Glaucoma drainage devices maintain a vital role for certain types of glaucoma including those refractory to other surgery. Cyclodestruction continues to have a role mainly for patients following failed drainage/filtering surgery. Although the prognosis for childhood glaucoma has improved significantly since the introduction of angle surgery, there is still considerable progress to be made to ensure a sighted lifetime for children with glaucoma all over the world. Collaborative approaches to researching and delivering this care are required, and this paper highlights the need for more high-quality prospective surgical trials in the management of the childhood glaucoma.
Similar content being viewed by others
Introduction
Managing glaucoma in childhood is one of the greatest challenges in the field of glaucoma, especially with regard to surgical treatment.1 Childhood glaucoma is characterised by elevated intraocular pressure (IOP)-related damage to the eye, which can be caused by a diverse group of conditions.2 Its presentation can vary because depending on the age of onset, elevated IOP can affect the whole eye, and not just the optic disc and has recently been redefined to reflect this fact. 2
Once a child has been diagnosed with glaucoma, the goal, where possible, is to provide a lifetime of vision. Medications are an important part of management; they are usually first line treatment for most glaucomas, they temporise IOP control prior to surgery, for example, primary congenital glaucoma (PCG), and are often required as adjunctive therapy after partially successful surgery for IOP control.3 However, surgery is the mainstay of treatment for childhood glaucoma and is often inevitable in a child’s lifetime.4
The available surgical repertoire for childhood glaucoma has remained relatively unchanged for many years. Each surgical technique has its advantages and disadvantages with potentially good success rates when chosen appropriately and performed with meticulous attention to detail to minimise complications.5 Given that most children with glaucoma have normal life expectancies and may, therefore, need several operations to control IOP, the impact of successful surgical treatment on the patients and their families cannot be underestimated. However, glaucoma surgery in children is more challenging and associated with higher failure6, 7 and complication rates compared with adults.
Internationally, there is a markedly diverse approach to surgery for childhood glaucoma, more so than for adult glaucoma and this was confirmed in the international childhood glaucoma surgery survey conducted as part of the recent World Glaucoma Association consensus meeting on Childhood Glaucoma.5 This reflects the rarity and variations of the disease, the difficulty we face in controlling the IOP, training and experience, the local availability of facilities and equipment, individual population challenges, including drop availability, affordability and access to care, and local variations in disease beliefs, compliance and fear of surgery. It is further compounded by the fact that there is a paucity of randomised surgical trials in childhood glaucoma to guide us.
This review starts with a brief history of childhood glaucoma surgery and reviews factors that influence our choice of surgery. We then discuss each main operation in our armamentarium in some detail with emphasis on recent developments. We conclude with thoughts on the future direction of the management of this complex, potentially blinding disease, and goals for the 21st century.
History
Childhood glaucoma surgery in the present, or even the future, is best discussed in the context of the past. Almost all techniques in the childhood glaucoma surgical armamentarium have originated for use first in adults, then transferred, and adapted for use in children. The evolution of childhood glaucoma surgery exemplifies well the fact that advances in surgery usually occur in an attempt to improve outcomes, in this case longer term IOP control with the associated visual and quality of life benefits, and to reduce complications.
Significant turning points in childhood glaucoma surgery began in the early 1940s when Barkan8 first published his results in children with glaucoma of an angle procedure he called goniotomy. Barkan9 along with De Vincentiis,10 the originator of this technique, had tried goniotomy unsuccessfully first in adults. However, in children Barkan8 was able to control IOP and preserve visual function in the majority, which until then was unprecedented. With time, goniotomy proved to be both successful and safe, providing there was adequate corneal clarity to view the angle.11, 12 The next turning point occurred in 1960 when the technique of rupturing the inner wall of Schlemm canal was described independently by both Smith,13 with use of a nylon filament, and Burian,14 with a rigid probe (trabeculotome) who named the procedure trabeculotomy ab externo. As trabeculotomy could be performed regardless of corneal clarity, its popularity increased rapidly all over the world especially in populations where corneal opacification on presentation was a common finding. Subsequently, endoscopic goniotomy15, 16 was described to enable goniotomy in the presence of a hazy cornea but it failed to be extensively adopted. Both goniotomy and trabeculotomy, which incise the angle in an attempt to improve innate aqueous outflow, with time revealed similar high rates of success when repeated, especially in favourable PCG cases for example, onset between 1–24 months of age.11 However, it was in recognition of the fact that angle surgery was not always successful in PCG and less so in secondary glaucoma cases17, 18 that alternative operations were sought that had better outcomes than full thickness drainage procedures.
The late 1960s saw the introduction of both trabeculectomy by Cairns19 and the first glaucoma drainage device (GDD) by Molteno20 in the adult glaucoma world. These operations, which created an external outflow pathway, were soon adopted for use in children, especially for those with refractory glaucoma. Publications also appeared describing cyclodestruction (cyclocryotherapy)21 as treatment for glaucoma, later to be eventually replaced by diode laser.22
These techniques have all stood the test of time but since the late 1960s, no new operation has found routine use in childhood glaucoma. Major advances have instead relied on combining techniques, revisiting old techniques or modifications to existing techniques to move the subspecialty forward. We have also continued to adopt new technologies pioneered in adult glaucoma surgery.
In 1980 Maul et al23 first described combining trabeculotomy with trabeculectomy to improve success. Combined trabeculotomy–trabeculectomy with time became and remains popular particularly in populations with advanced disease on presentation and those thought to be at greater risk of failure from angle surgery such as in the Middle East and India.24, 25, 26, 27 However, no prospective comparisons exist to support the argument that combining the procedures improves success.
With the knowledge that incising a greater extent of the angle when repeating angle surgery often improved outcomes, in 1994 Beck and Lynch28 revisited Smith’s trabeculotomy technique using a blunted 6/0 prolene suture instead of nylon to achieve a circumferential incision with one procedure alone that did not need to be repeated, circumferential (360°) suture trabeculotomy. The introduction of an illuminated microcatheter, first used in adult canaloplasty surgery, as a substitute for the suture, improved the safety of the procedure.29
The 1990s were also remarkable for the widespread introduction of anti-scarring agents in trabeculectomy surgery to improve success.30, 31 As a primary or secondary procedure in children, trabeculectomy was still associated with failure in many cases due to excessive scarring. In 1991, Miller and Rice32 demonstrated that the use of beta radiation as an anti-scarring agent at the time of surgery prolonged trabeculectomy survival in children. The single intraoperative use of Mitomycin C (MMC) with trabeculectomy in children appeared to increase the success in some series but complications too, especially those related to hypotony and bleb-related complications including endophthalmitis.33, 34, 35, 36 Subsequently, simple modifications to the intraoperative application of MMC and to the surgical technique have reported much reduced long-term complication rates and more favourable bleb morphology.37, 38
In 1994, Tixier et al39 were the first to publish their results of non penetrating surgery (deep sclerectomy) in children following reports in adults of its advantageous risk profile. Again the origins of this technique, like penetrating surgery (trabeculectomy) derived from the 1960s when Krasnov40 described it in an attempt to avoid the potential complications associated with ocular entry. Subsequent studies suggested significant conversion rates to trabeculectomy41, 42 or unintentional macroperforations (30%).43 More recently, some authors have argued for improved results by combining deep sclerectomy and trabeculectomy.44
Deep sclerectomy and numerous other techniques described in adults including viscocanalostomy,45 suprachoroidal shunts (SOLX (SOLX Inc, Waltham, MA, USA), CyPass (Transcend Medical Inc, Menlo Park, CA, USA)), canaloplasty, trabecular meshwork bypass shunts (eg, iStent (Glaukos Corporation, Laguna Hills, CA, USA), Hydrus (Ivantis Inc, Irvine, CA, USA)) and transscleral shunt (AqueSys Xen (AqueSys Inc, Aliso Viejo, CA, USA)) have not been widely adopted in children because they are yet to be proven efficacious or safe in children and because of the technical challenges of buphthalmic eyes with thin sclera. A recent addition to angle surgery, trabectome surgery (trabeculotomy ab interno) uses a disposable, high frequency electrocautery handpiece to remove the inner wall of Sclemm canal and the trabecular meshwork.46 As in goniotomy, the handpiece is introduced via the temporal cornea and a clear view of the angle is required. Although studies include small numbers of paediatric cases, there are no specific details of outcomes in children.47
Challenges to successful surgery
There are a great many challenges to successful surgical management of the childhood glaucomas. Some relate to the difficulties of operating on eyes with distorted anatomy owing to buphthalmos, anatomical features of some of the secondary glaucomas, and the legacy of previous surgeries. Another major challenge is the aggressive healing response, which can hinder the effectiveness of surgeries that depend on creating alternative pathways for aqueous drainage from the eye, such as trabeculectomy and GDD. This is all compounded by the difficulty of administering care to children with limited ability to co-operate and cope with the post-operative medications required for the success of many of these surgeries.
Buphthalmic eyes have low scleral rigidity and are predisposed to surgical complications related to low IOP such as anterior chamber (AC) collapse, maculopathy, choroidal effusion, suprachoroidal haemorrhage, and phthisis. Procedure-specific difficulties may also be encountered which include: correctly positioning the trabeculectomy flap or identifying Schlemm canal in the presence of altered anatomy (stretched limbus), fashioning a scleral flap in the presence of thin tissue, suturing the scleral flap without cheese-wiring through the delicate tissue, adequately sealing the aqueous outflow of the trabeculectomy and leakage around the tunnel of GDDs. A lack of familiarity with buphthalmic eyes is associated with more complications. Furthermore, specific ocular conditions associated with glaucoma (eg, Sturge–Weber syndrome, aphakia, aniridia), limited access to the surgical site (eg, small palpebral aperture and small orbits in infants and young children), and underlying general medical conditions can all contribute to the challenges of surgically managing children with glaucoma.
The aggressive healing response of paediatric eyes is thought to contribute to the lower success rates for glaucoma surgery compared with adults. Trabeculectomy surgery is, therefore, often enhanced by the use of anti-scarring agents but they may be associated with significant complications.
In the post-operative period, regular and sometimes intensive topical drop therapy is required to mitigate against complications of excessive scarring and infection. This may present real challenges for the caregivers of these children who may have to overcome difficulties with co-operation in young children, or at times resistance from schools or other caregivers in assisting with instilling drops and post-operative activity restrictions. Additionally caregivers need to commit to frequent visits to the ophthalmic unit for post-operative monitoring, which impacts the child’s schooling and potentially the carer’s ability to commit to work or care for the rest of their family. The surgical team also faces challenges when trying to examine these children adequately and perform post-operative manipulations such as suture removal or application of further anti-scarring agent. Examinations under anaesthesia (EUA) may be required for this purpose, often on a repeated basis.
Even when surgical success is achieved for these children, concurrent ametropia correction and amblyopia therapy, where indicated, is essential to optimise long-term visual outcome, which is the true measure of success.48 The management of amblyopia and ongoing monitoring of glaucoma requires continued commitment from the caregivers and the ophthalmic team.
In light of the above significant challenges, the recent World Glaucoma Association Consensus on Childhood Glaucoma has stated that surgery should preferably be performed by a trained surgeon in centres where there is sufficient volume to ensure surgical experience and skill, and safe anaesthesia.5 In parts of the world where this is possible, increasingly cases are managed in tertiary centres with specialist experience.3
The choice of surgical procedure
In the surgical management of childhood glaucoma, the best chance of successfully controlling IOP and preserving vision lies with the first operation chosen7, 49, 50 and having a long-term surgical strategy. The best surgical procedure for any particular child with glaucoma cannot always simply be determined by a set algorithm. The decision is made based on a combination of diverse factors including: the underlying aetiology of the glaucoma, the associated ocular features, previous ocular surgery, the likelihood of further ocular surgery (eg, cataract extraction), the age of the child, the extent of glaucomatous optic nerve damage, the visual prognosis, the general health of the child, the social circumstances (ie, the likelihood of follow-up) and available carer support, local facilities, and surgeon expertise. It is worth mentioning that one must carefully consider the risks and benefits of any intervention in discussion with the parents, particularly in refractory cases when the fellow eye is healthier or if the child only has one eye.
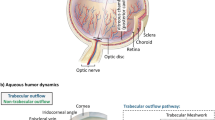
Broadly, the common surgical choices may be divided into those which: (i) enhance the innate aqueous outflow pathway (angle surgery), (ii) create an external aqueous outflow (trabeculectomy and GDD) and (iii) reduce aqueous production (cyclodestructive procedures). Each of these is described below including the indications, success rates, and complications.
Surgical armamentarium
Angle surgery
The attraction of angle surgery is the potential to harness the innate or ‘natural’ outflow mechanism by allowing aqueous access to Schlemm canal and the collector system; in so doing it is the closest approach we have to addressing the fundamental underlying cause of the glaucoma in cases of primary trabecular dysgenesis. Its undisputed role is as primary surgery for PCG with the proviso that it is less successful with early (<1 month of age) and late presentations (>2 years of age) and with enlarged ocular dimensions (corneal diameter of >14 mm). Some have advocated its use in secondary glaucomas such as JOAG and aphakic glaucoma, but it is generally less successful with the exceptions of uveitic glaucoma51 and in conditions with ‘PCG-like’ angles eg, congenital rubella17, 52 and infantile presentations of Sturge–Weber syndrome.53
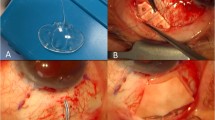
Goniotomy and trabeculotomy have been widely practiced since their introduction. Their difference lies in the approach to the angle—goniotomy from an internal approach (via a paracentesis and instruments in the AC) and trabeculotomy from an external approach (using a scleral cut down to access Schlemm canal). Goniotomy technique has largely remained unchanged from the time it was described by Barkan with the addition only of minor modifications such as the use of: viscoelastic or AC infusion to maintain AC depth, needles instead of a tapered knife for the angle incision, various goniolenses, and the use of alcohol or hyperosmotic solutions to clear the epithelial oedema. The trabeculotomy technique has developed with regard to the mechanism of angle incision from a metal probe (trabeculotome) to a blunted suture filament or an illuminated microcatheter. (Refer to Table 1).
The question is whether recent developments and modifications improve their success and safety profiles and when to use which procedure. Advances in technology, especially in the 21st century, have extended the scope of both trabeculotomy and goniotomy a little further; in the case of trabeculotomy, an illuminated microcatheter allows visualisation of its safe passage through Schlemm canal, and the potential to treat the whole angle in one surgery and potentially improve its success rate; in the case of goniotomy, an endoscopic approach allows visualisation of the angle in situations of poor corneal clarity but possibly owing to cost and the learning curve associated with a new skill to master, it has not been extensively practiced.54, 55 Photodisruptive goniotomy has been described with Q-switched neodymium:yttrium aluminium garnet (Nd:YAG) laser to avoid invasive intraocular surgery, but despite encouraging early results when compared with surgical goniotomy56 it did not prove to be a useful long-term tool for goniotomy (verbal communication with Vivian Balakrishman and David Taylor) when used at a major paediatric glaucoma centre.
Until recently, the argument when considering the choice of angle surgery between goniotomy and conventional trabeculotomy was based on the issues of the potential impact of angle surgery on future glaucoma surgeries and corneal clarity. As is often the case for surgical procedures in rare diseases, there is a paucity of truly randomised controlled studies comparing the two. It is generally accepted that for similar degrees of disease severity the two procedures offer similar rates of success (70–90% after multiple attempts in favourable cases).11, 12, 49, 57, 58, 59, 60, 61, 62, 63 However, proponents of goniotomy argue in its favour when considering the long-term effects in children who are likely to face further glaucoma surgery at some other point in their lives. It is now well accepted that future success of trabeculectomy is prejudiced when there have been previous surgeries that involve the conjunctiva. As a scleral cut down is required for the external approach of trabeculotomy, this violates the conjunctiva and sclera and makes future trabeculectomy (or GDD placement) potentially more technically challenging as well as more prone to failure. Employing an inferotemporal approach when performing trabeculotomy preserves the superior site for future trabeculectomy and may mitigate against some of these effects. The main advantage that trabeculotomy enjoys over goniotomy is that it can be performed in the presence of an opaque cornea and it allows access potentially to 360° of the angle through one incision. When corneal haziness is primarily due to epithelial microcystic oedema, however, there are several manoeuvres that may assist in achieving sufficient corneal clarity to allow a goniotomy and so capitalise on its advantages, such as stripping the epithelium following pre-treatment with topical alcohol.64
In cases of an inadequate response, both goniotomy and conventional trabeculotomy with probes can be repeated, in the untreated angle. This increases the overall success rate of surgery, though is not always sufficient, which may lead to a third angle surgery or filtering surgery as the next step. This incremental step-wise approach employs multiple surgeries, and there is a tension between the need for repeated anaesthetics to allow sufficient monitoring and treatment of the disease and the concern for possible deleterious effects on young brain development.65, 66 In this regard, the recent evolution of circumferential (360°) trabeculotomy using an illuminated microcatheter,29, 67 instead of a suture, may offer a significant improvement to the approach to the paediatric angle in the 21st century. It potentially allows treatment of 360° of the angle in a single surgical episode, confidence that the TM has been ruptured to connect Schlemm canal with the AC, and is not associated with prolene suture complications such as subretinal positioning from misdirection.68, 69 The success of circumferential (360°) trabeculotomy in eyes with PCG varies from 77–92% after 1–4 years28, 67, 70, 71 similar to success rates of angle surgery after multiple operations. However, despite its advantages, success may not always be possible with a single incision as the suture or microcatheter may not advance all the way around Schlemm canal.28, 67 If the IOP response is inadequate, the next step would be filtration surgery (trabeculectomy or GDD) as there would be no gain in further angle treatment. Again, a temporal approach may mitigate against some of the disadvantages of an external approach, and on balance the advantages of a single surgical episode to treat the whole angle may outweigh the incremental approach, even though 360° angle treatment is not necessarily required in many cases. The answer to the question as to which is the next best operation after failed angle surgery for PCG is disputed. No randomised trials exist and the results from published retrospective series are conflicting.72, 73
When choosing between the angle surgeries, we favour goniotomy as first line for PCG and ‘PCG-like angles’ up to the age of 3 years because it spares conjunctiva and sclera. We may consider it in older children owing to the ease and safety of surgery, but complications such as hypotony may be more common and the success rate lower. We would generally only repeat angle surgery if there had been some response to the first operation and virtually never do more than two angle surgeries. Circumferential trabeculotomy using the illuminated microcatheter holds significant promise as a way forward in PCG cases but less so in secondary glaucoma where the results are poorer and complications potentially higher.71 Once angle surgery fails we usually move on to trabeculectomy surgery, even in infants.
Trabeculectomy
The initial studies published on trabeculectomy in children involved eyes with advanced glaucoma and numerous previous surgeries. Unsurprisingly, the results were poor and the complication rates were high.74 Despite more encouraging reports with primary unenhanced trabeculectomy,75, 76 excessive scarring remained a barrier to success for many cases. Intraoperative application of beta radiation (750 cGy) to the surgical site was associated with improved outcomes, diffuse elevated blebs, and no increase in complications.32 MMC, a more potent inhibitor of fibroblast function, is thought to improve success rates,33, 77, 78 however this is disputed by other studies.79, 80 Furthermore, it can be used at varying potencies and requires only intraoperative exposure, which is a major advantage over 5FU in children.
The use of MMC is associated with higher complication rates that are well documented in the literature and include early complications related to hypotony (shallow or flat AC, hypotony maculopathy, choroidal effusion, suprachoroidal haemorrhage) and late complications associated with thin avascular, cystic blebs prone to leakage and potentially blinding infection, as high as 17%.33, 35, 36, 81, 82 These complications have led to trabeculectomy developing a poor reputation in children.
With regard to success, poor results for trabeculectomy in children with glaucoma following congenital cataract surgery even with MMC have been reported by many investigators.34, 78, 83 Furthermore, success in infants has been reported to be lower than older age groups33, 35, 82 and when compared with GDD.72 However, it is our experience that with simple modifications to the surgical technique and with suitable anti-scarring potency and application technique (Moorfields Safer Surgery System),37, 38 trabeculectomy can be associated with satisfactory outcomes in appropriate cases, even infants.
The main questions regarding trabeculectomy surgery are: who are the best candidates for it; which is the appropriate scarring agent and dose and what to do when it fails? The answers to these questions are difficult to obtain from the available literature as all studies of trabeculectomy in childhood glaucoma have numerous limitations which include: retrospective design, various case mix, variable technique, and follow-up along with regional and surgeon preference bias. Our approach is for trabeculectomy to be first line for most secondary glaucomas with the exception of those known to have a poor prognosis such as in cases of aphakia or pseudophakia associated either with congenital cataract surgery or with uveitis In other secondary glaucomas, the presence of a cataract that may need removal in the near future, or corneal pathology that may require transplantation in the near future, would also argue against trabeculectomy.
In PCG cases, our most common indication for trabeculectomy is failed angle surgery but may also be considered by surgeons unfamiliar with angle surgery or if angle surgery is not possible. Further indications may be in situations where very low target pressures are required (advanced optic disc damage or to improve corneal clarity) and where there are poor prognostic factors for angle surgery. With regard the anti-scarring agent, we suggest MMC for those experienced in its use. The number of risk factors for failure determines the most appropriate dose. An approach when using MMC in infants following failed angle surgery is to use a low dose for example, 0.1–0.2 mg/ml at the time of surgery which minimises the risk and duration of early complications such as hypotony but then to ‘top up’ the agent with multiple 5FU injections at the time of post-operative EUAs. An AC maintainer is used in all cases to minimise intraoperative hypotony and also to facilitate the accurate judgement of flow through the scleral flap. When trabeculectomy fails to control IOP, bleb needling may be attempted with an anti-scarring agent if the bleb architecture allows and the sclerostomy is patent. Repeated needling may be necessary with early failure. Trabeculectomy may be repeated with a stronger dose of MMC or a GDD may be considered if further surgery is required.
GDD
Molteno84 first published the use of his GDD in children in 1973. Since then further GDDs have been introduced with the most commonly used devices currently being the Ahmed implant (96 mm2/184 mm2) with uni-directional flow restriction, which theoretically reduces the risk of early hypotony (New World Medical Inc., Rancho Cucamonga, CA, USA) and the Baerveldt implant (250 mm2 and 350 mm2), which is an unrestricted implant (AMO Inc., Abbott Park, IL, USA) and so requires additional measures to minimise early hypotony.5
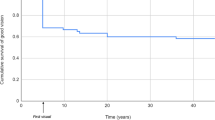
Success rates in published studies of GDDs are difficult to compare because of the same limitations stated above for trabeculectomy studies. Common to all studies is reduced success over time and the need for adjunctive medication. At 1–2 year follow–up, many studies report a success of around 80%85, 86, 87, 88 and this falls to around 50% in the longer term.72, 89, 90, 91, 92 When debating which GDD performs best in children—there is no clear superiority of one type of GDD versus another, however the Baerveldt implant may provide slightly better long-term IOP control but the Ahmed implant fewer short term complications.93, 94, 95 A prospective study comparing the polypropylene against the silicone Ahmed implant in children, has shown better long-term IOP control with the silicone Ahmed.96 The choice of implant is often determined by factors, such as the diagnosis, implant availability and affordability, positioning (when placing the surgery superonasally, the Baerveldt implant may be better because of its lower profile and it does not extend as far back posteriorly as the Ahmed implant), the surgeon’s experience, and the child’s circumstances.
Post-operative hypotony is a major sight-threatening complication of GDD surgery in children. External ligation of both flow restricted and unrestricted implants has been described to reduce aqueous flow and reduce this risk.97, 98, 99, 100, 101 Absorbable suture material may be used for the external ligature so that restricted flow is spontaneously released after a number of weeks, or non-absorbable material used enabling the surgeon to release the ligature at a planned interval by laser suture lysis or surgical removal. In unrestricted implants, an intraluminal stent may be used in addition to, or as an alternative to, external ligation to restrict aqueous flow and to avoid hypotony. Despite restriction of aqueous flow through the GDD, hypotony may still occur unless a watertight tunnel into the AC is achieved. An alternative strategy to minimise hypotony is implantation of the GDD in a two-stage procedure, whereby the plate is secured to the sclera at the first surgery and the tube then inserted some weeks later when encapsulation of the plate has occurred.102, 103, 104
Other complications particularly pertaining to GDDs include: corneal touch with corneal decompensation, lens touch with cataract formation, iris touch with persistent iritis or dyscoria, and migration of the tube. This tube migration can occur either into the AC or posteriorly out of the AC, tube obstruction from vitreous, iris, haemorrhage, fibrin or inflammatory membrane, and tube erosion and exposure leading to infection and endophthalmitis.105 Furthermore, GDDs can be cosmetically unsightly and cause motility issues.
Our usual preference is for the Baerveldt 350-mm2 implant, where possible, because of it larger surface area. The 250 mm2 is preferred for uveitic eyes that are prone to aqueous hyposecretion and microphthalmic eyes that have smaller ACs that can easily shallow with hypotony. To keep complications to a minimum, we use various strategies including the use of an AC maintainer to minimise intraoperative hypotony, a tight tunnel with a 25-gauge needle, both an extraluminal ligature (6/0 vicryl) and an intraluminal stent (3/0 supramid) to restrict flow. In the early post-operative period, elevated IOP is mitigated by the use of tube fenestration (venting slit). Viscoelastic may be utilised to maintain depth of the AC postoperatively if required.
Complications related to tube touch are minimised by directing the tube tunnel at the point of entry close to and parallel to the iris away from the cornea. An anterior vitrectomy in aphakic patients minimises the risk of tube occlusion by vitreous. The risk of tube exposure is reduced by constructing the tunnel at least 1–2 mm from the limbus and avoiding a corneal tunnel that would not be covered by the patch graft. Patch graft material, such as sclera or cornea unsuitable for transplantation, is used to reduce the risk of tube erosion, although techniques have been described using only scleral flaps or long tunnels of insertion. Other materials used to cover the tube are pericardium, thick amniotic membrane or dura mater.106, 107, 108
Tubes are most often inserted into the AC where the proximal tip can be easily visualised. In circumstances where the cornea is in danger of decompensation or when the AC is very shallow, posterior insertion through pars plana or the ciliary sulcus may be considered, although this approach is best reserved for pseudophakic or aphakic eyes and performed in combination with a thorough anterior vitrectomy to prevent tube occlusion. However, the incidence of complications may be higher with pars plana versus limbal tube insertion and includes tube occlusion by vitreous, choroidal effusions, suprachoroidal haemorrhage, vitreous haemorrhage, and retinal detachment.109
The main cause of GDD failure is fibrosis and encapsulation around the plate. Whereas in trabeculectomy the use of anti-scarring agents to reduce fibrosis is thought to improve the success of surgery, the same advantage has not been clearly established in GDD surgery with conflicting results in the published paediatric literature.110, 111, 112 In patients who have failed GDD surgery, it is our experience that further GDD surgery with MMC can be successful.
The threshold for using GDDs in childhood glaucoma has been lowered in recent years, as surgical techniques have been refined to improve the success rates and reduce the complications of surgery, particularly the prevention of hypotony. Although GDDs have the advantage of potentially requiring fewer post-operative interventions to achieve IOP control as compared with trabeculectomy, which may require suture lysis, adjustment or removal, needling and supplemental subconjuctival anti-scarring injections; this must be balanced with the potential for complications of this surgery and slightly higher post-operative IOP with GDD compared with a MMC enhanced trabeculectomy. Our preference is to use a GDD as the primary surgery for children with uveitis who are aphakic or pseudophakic, children who develop glaucoma following cataract surgery or who have a cataract that will need future imminent removal. Also we use a GDD in preference to trabeculectomy in patients with Sturge–Weber syndrome who have a choroidal haemangioma, as with the technique described above, post-operative hypotony is less likely compared with trabeculectomy in which early post-operative IOP may be less predictable. An additional indication is failed enhanced trabeculectomy and very severe disease with onset at birth as these cases have a very high failure rate even with MMC trabeculectomy.
Following failure of GDD, the introduction of topical glaucoma therapy provides the simplest and lowest risk option. Needling or surgical revision of the bleb over the plate (capsule excision) may be attempted but published studies have shown the outcomes are inferior to additional GDD implantation.113, 114, 115 Sequential tube surgery may, however, result in more corneal complications. In children, small series of sequential tube surgery in a different quadrant report reasonable success rates.116, 117 One study comparing cyclophotocoagulation with sequential tube surgery following failure of primary GDD in children suggested similar success and complication rates, although again no long-term follow-up data are available.118 Our experience with needling and surgical revision suggests that the satisfactory IOP control is short lived especially with needling. After a failed GDD, we usually prefer diode laser as the next procedure before proceeding with a second GDD.
Cyclodestruction
Cyclodestruction, with the aim of reducing aqueous production, by cyclocryotherapy was associated with poor long-term results in children.119, 120 It was traditionally reserved for challenging, refractory childhood glaucoma cases because of its significant association with complications.121
It eventually became replaced with the less destructive, laser cyclophotocoagulation. Specifically, transcleral diode laser (810 nm)122 became more popular than Nd:YAG laser123 because it was better tolerated and associated with fewer complications. But a major drawback of the transcleral approach is ensuring accurate laser placement in buphthalmic eyes with distorted landmarks and hence difficulty in titration of laser energy. Endoscopic diode laser allows precise treatment of the ciliary processes,124 but the disadvantage is it requires an intraocular approach and caution is suggested in phakic patients. Complications associated with diode laser include: hypotony, significant uveitis, phthisis, conjunctival burns, uveitis, scleromalacia, scleral perforation, cataract, retinal detachment, and loss of vision especially in eyes with two or more treatments or in eyes with pre-existing poor vision.122, 125, 126, 127, 128 Short-to-medium term outcomes of transscleral diode laser quote over 50% success but with a high retreatment rate and a continuation of medical therapy.127, 128 Endoscopic diode achieves similar results with a lower re-treatment rate.124, 129, 130
Our preference is to use transscleral diode laser with transillumination of the eye to improve the accuracy of laser placement, and we avoid areas of pigmentation, haemorrhage, and scleral thinning. If future GDD surgery is planned, we do not treat the superotemporal quadrant to avoid scleromalacia. Lower energy doses as suggested for microphthalmic eyes. We commonly use it for treating blind, painful eyes or those with poor visual potential. Additional indications are, if surgery: has a poor prognosis; is technically difficult or impossible for example, severely scarred conjunctiva or there are significant ocular abnormalities; has failed for example, after a trabeculectomy or GDD. Occasionally it may be useful as a temporising measure, for example, an acute presentation of significantly elevated IOP as occurs following trauma, during the hypertensive phase of an Ahmed implant in aphakic/pseudophakic eyes or when a definitive procedure must be delayed for example, fellow eye has undergone major surgery. We advise against the use of diode laser in children with uveitis not only because it is associated with poor outcomes131 but also because it aims to reduce ciliary body function that may already be compromised by inflammation. Furthermore, future more invasive surgery may lead to problems with chronic hypotony.
Childhood glaucoma in the developing world
Childhood blindness from all causes is still largely untreated, or under-treated in the developing world. There are many barriers to care when looking after children with glaucoma in addition to the usual challenges.132, 133, 134, 135 Most of the glaucoma surgeries require microscopic surgical expertise and specialised equipment and as most new technologies have first world markets in their sights, less affluent and developed countries do not always enjoy their benefits. Addressing the gulf between the developed and developing world health care provision should be an aim of any surgical specialty in the 21st century. A significant barrier to appropriate treatment is the cost of GDDs in the developing world. Recently an Indian company has developed a non restricted GDD (Aurolab Artificial Drainage Implant, Madurai, India) at a fraction of the price of similar models. It is currently undergoing a clinical trial to evaluate safety and efficacy in patients with refractory glaucoma.
One of the hallmarks of the 21st century is the ubiquitous nature of the cell phone and its ever expanding functions in the form of image transfer and user-friendly applications. This provides penetration for a web based approach in bringing first world expertise to support care in more remote and underserved areas. 136
Future
Although the surgical treatment of childhood glaucoma has improved considerably in the last few decades, there are still considerable unmet needs. The ideal surgical treatment across the world needs to have several characteristics. It has to achieve a good IOP, preferably at levels close to 10 mm Hg, last the patient’s lifetime, have no complications, maintain good vision, be completed in a relatively short time, and achieve a 100% success rate even in traditionally highly refractory patients. Currently, no treatment is close to this ideal, but in selected cases of angle surgery, particularly goniotomy, it come close to this with some of our original patients well controlled for nearly six decades to date after a goniotomy taking 10 min.
New devices that can be much more easily placed with fluid regulating and biocompatible qualities far better than current devices together with better anti-scarring agents may allow for many aspects of the ideal glaucoma surgery in the future. Current and future technologies are now coming closer to this ideal. We have set an audacious goal of the 10 : 10 : 10 challenge for glaucoma—10 mm Hg, for 10 years done in 10 min. It will take multidisciplinary work across many areas of expertise to achieve this including fluid flow engineering, bioengineering, pharmacologists and clinician scientists to achieve this future.
From the perspective of angle surgery further advances in our ability to image angle structures for example, Schlemm canal would assist in determining those unsuitable for trabeculotomy surgery.
In keeping with most rare diseases, particularly in children, there is the paucity of high quality evidence in childhood glaucoma surgery to guide clinicians. The limited data available from prospective trials fail to address issues such as: the procedure of choice to control IOP in glaucoma refractory to angle surgery—enhanced trabeculectomy or GDD? Is trabeculotomy–trabeculectomy superior to either trabeculotomy or trabeculectomy alone? Is MMC indicated in primary trabeculectomy surgery or only when the conjunctiva has been previously incised? What is the ideal MMC concentration and duration of exposure? Does previous diode laser increase the failure rate of subsequent surgery? When evaluating surgical techniques, a standaridised definition of success is required, which is lacking in childhood glaucoma and needs to take into account more than just the IOP control achieved.
The Childhood Glaucoma Research Network (CGRN) was established by glaucoma specialists and paediatric ophthalmologists with an interest in glaucoma in 2011 to address these unmet needs and subsequently improve the care of children with glaucoma. Its initial focus was on defining and classifying glaucoma, which was recently adopted by the WGA consensus on childhood glaucoma.2 The CGRN hopes eventually to perform multicentre clinical trials to evaluate and compare present techniques and in doing so answer the many questions, which largely retrospective studies and experience currently attempt to inform. As a prelude to this an internet-based international registry of new childhood glaucoma patients, the International Pilot Survey of Childhood Glaucoma, has been established to ascertain existing clinical practice.
A neglected field within childhood glaucoma is the study of the impact of the diagnosis and surgery on the child’s quality of life and that of the caregivers. Evidence is sparse but it suggests the impact of childhood glaucoma is significant throughout the child’s life both at home and school.137 Furthermore, the emotional and psychological burden of caregivers of patients with childhood glaucoma is thought to be considerable.138 Recognition of the importance of the measuring the impact of illness, disability, and treatment from the patient’s perspective has resulted in development and evaluation of Patient-Reported Outcome Measures and Patient-Reported Experience Measures for use within paediatric ophthalmology.139 However, there is a paucity of vision-specific instruments. Hopefully, the fact that patient-led assessment of the impact of disease has developed a high profile in health service planning and policy in some countries will result in more funding for this research.140
Conclusion
Childhood glaucoma is recognised to be one of the most challenging diseases in the field of glaucoma, and this is especially so for its surgical management because of the potential for failure and complications. Over the past 70 years, a number of operations have been introduced to manage childhood glaucoma, most of which have stood the test of time but others have still to prove themselves. Internationally, there is a diverse approach to childhood glaucoma that largely reflects the diverse nature of the conditions, which cause it, the challenges of controlling the disease and the absence of controlled trials to inform decision-making. The 21st century prognosis for childhood glaucoma has improved significantly since the days when angle surgery was first introduced but the challenge for those who look after these children still remains, as it always has, to increase surgical success rates and reduce complications, and thereby keep these children seeing for as long as possible.
References
Khaw PT, Freedman S, Gandolfi S . Management of congenital glaucoma. J Glaucoma 1999; 8: 81–85.
Beck A, Chang TCP, Freedman S . Definition, Classification and Differential Diagnosis. In: Weinreb RN, Grajewski A, Papadopoulos M, Grigg J, Freedman S, (eds) Childhood Glaucoma.. WGA Consensus Series – 9. Kugler Publications: Amsterdam, 2013 pp 3–10.
Papadopoulos M, Cable N, Rahi J, Khaw PT . The British infantile and childhood glaucoma (BIG) eye study. Invest Ophthalmol Vis Sci 2007; 48: 4100–4106.
Taylor RH, Ainsworth JR, Evans AR, Levin AV . The epidemiology of pediatric glaucoma: the Toronto experience. J AAPOS 1999; 3: 308–315.
Papadopoulos M, Edmunds B, Chiang M, Mandal A, Grajewski AL, Khaw PT . Glaucoma Surgery in Children. In: Weinreb RN, Grajewski A, Papadopoulos M, Grigg J, Freedman S, (eds) Childhood Glaucoma.. WGA Consensus Series – 9. Kugler Publications: Amsterdam, 2013 pp 95–134.
Gressel MG, Heuer DK, Parrish RK 2nd . Trabeculectomy in young patients. Ophthalmology 1984; 91: 1242–1246.
Inaba Z . Long-term results of trabeculectomy in the Japanese: an analysis by life-table method. Jpn J Ophthalmol 1982; 26: 361–373.
Barkan O . Operation for congenital glaucoma. Am J Ophthalmol 1942; 25: 552–568.
Barkan O . A new operation for chronic glaucoma. Am J Ophthalmol 1936; 19: 951–966.
De Vincentiis C . Incisione dell’angolo irideo nel glaucoma. Ann di Ottal 1893; 22: 540–542.
Shaffer RN . Prognosis of goniotomy in primary infantile glaucoma (trabeculodysgenesis). Trans Am Ophthalmol Soc 1982; 80: 321–325.
Russell-Eggitt IM, Rice NS, Jay B, Wyse RK . Relapse following goniotomy for congenital glaucoma due to trabecular dysgenesis. Eye (Lond) 1992; 6: 197–200.
Smith R . A new technique for opening the canal of Schlemm. Preliminary report. Br J Ophthalmol 1960; 44: 370–373.
Burian HM . A case of Marfan’s syndrome with bilateral glaucoma. With description of a new type of operation for developmental glaucoma (trabeculotomy ab externo). Am J Ophthalmol 1960; 50: 1187–1192.
Joos KM, Alward WL, Folberg R . Experimental endoscopic goniotomy. A potential treatment for primary infantile glaucoma. Ophthalmol 1993; 100: 1066–1070.
Medow NB, Sauer HL . Endoscopic goniotomy for congenital glaucoma. J Pediatr Ophthalmol Strabismus 1997; 34: 258–259.
Rice NSC. The surgical management of congenital glaucoma. Aust J Ophthalmol 1977; 5: 174–179.
Luntz MH . Congenital, infantile, and juvenile glaucoma. Ophthalmology 1979; 86: 793–802.
Cairns JE . Trabeculectomy. Preliminary report of a new method. Am J Ophthalmol 1968; 66: 673–679.
Molteno AC . New implant for drainage in glaucoma. Clinical trial. Br J Ophthalmol 1969; 53: 606–615.
De Roetth A Jr . Cryosurgery for the treatment of glaucoma. Trans Am Ophthalmol Soc 1965; 63: 189–204.
Hennis HL, Stewart WC . Semiconductor diode laser transscleral cyclophotocoagulation in patients with glaucoma. Am J Ophthalmol 1992; 113: 81–85.
Maul E, Strozzi L, Munoz C, Reyes C . The outflow pathway in congenital glaucoma. Am J Ophthalmol 1980; 89: 667–673.
Elder MJ . Congenital glaucoma in the West Bank and Gaza Strip. Br J Ophthalmol 1993; 77: 413–416.
Debnath SC, Teichman KD, Salamah K . Trabeculectomy versus trabeculotomy in congenital glaucoma. Br J Ophthalmol 1989; 73: 608–611.
Al-Hazmi A, Awad A, Zwaan J, Al-Mesfer SA, Al-Jadaan I, Al-Mohammed A . Correlation between surgical success rate and severity of congenital glaucoma. Br J Ophthalmol 2005; 89: 449–453.
Mandal AK, Gothwal VK, Nutheti R . Surgical outcome of primary developmental glaucoma: a single surgeon’s long-term experience from a tertiary eye care centre in India. Eye (Lond) 2007; 21: 764–774.
Beck AD, Lynch MG . 360 trabeculotomy for primary congenital glaucoma. Arch Ophthalmol 1995; 113: 1200–1202.
Sarkisian SR Jr . An illuminated microcatheter for 360-degree trabeculotomy [corrected] in congenital glaucoma: a retrospective case series. J AAPOS 2010; 14: 412–416.
Chen CW, Huang HT, Bair JS, Lee CC . Trabeculectomy with simultaneous topical application of mitomycin-C in refractory glaucoma. J Ocul Pharmacol 1990; 6: 175–182.
Lanigan L, Stürmer J, Baez KA, Hitchings RA, Khaw PT . Single intraoperative applications of 5-fluorouracil during filtration surgery: early results. Br J Ophthalmol 1994; 78: 33–37.
Miller MH, Rice NS . Trabeculectomy combined with beta irradiation for congenital glaucoma. Br J Ophthalmol 1991; 75: 584–590.
Susanna R Jr, Oltrogge EW, Carani JC, Nicolela MT . Mitomycin as adjunct chemotherapy with trabeculectomy in congenital and developmental glaucomas. J Glaucoma 1995; 4: 151–157.
Beck AD, Wilson WR, Lynch MG, Lynn MJ, Noe R . Trabeculectomy with adjunctive mitomycin C in pediatric glaucoma. Am J Ophthalmol 1998; 126: 648–657.
Freedman SF, McCormick K, Cox TA . Mitomycin C-augumented trabeculectomy with postoperative wound modulation in pediatric glaucoma. J AAPOS 1999; 3: 117–124.
Sidoti PA, Belmonte SJ, Liebmann JM, Ritch R . Trabeculectomy with mitomycin-C in the treatment of pediatric glaucomas. Ophthalmology 2000; 107: 422–429.
Wells AP, Cordeiro MF, Bunce C, Khaw PT . Cystic bleb formation and related complications in limbus- versus fornix-based conjunctival flaps in pediatric and young adult trabeculectomy with mitomycin C. Ophthalmology 2003; 110: 2192–2197.
Khaw PT, Chiang M, Shah P, Sii F, Lockwood A, Khalili A . Enhanced trabeculectomy – The Moorfields Safer Surgery System. In: Bettin P, Khaw PT, (eds) Glaucoma Surgery. Dev Ophthalmol,. 50th Vol Karger: Basel, 2012 pp 1–28.
Tixier J, Dureau P, Becquet F, Dufier JL . Sclérectomie profonde dans le glaucome congénital. Résultats préliminaires. [Deep sclerectomy in congenital glaucoma. Preliminary results]. J Fr Ophtalmol 1999; 22: 545–548.
Krasnov MM . Sinusotomiia pri glaukome. Vestn Oftal 1963; 77: 33–41.
Luke C, Dietlein TS, Jaco bi PC, Konen W, Krieglstein GK . Risk profile of deep sclerectomy for treatment of refractory congenital glaucomas. Ophthalmology 2002; 109: 1066–1071.
Roche O, Beby F, Parsa A, Orssaud C, Dufier JL, Parsa CF . Nonpenetrating external trabeculectomy for congenital glaucoma: a retrospective study. Ophthalmology 2007; 114: 1994–1999.
Al-Obeidan SA, Osman EEA, Dewedar AS, Kestelyn P, Mousa A . Efficacy and safety of deep sclerectomy in childhood glaucoma in Saudi Arabia. Acta Ophthalmol 2014; 92: 65–70.
Feusier M, Roy S, Mermoud A . Deep sclerectomy combined with trabeculectomy in pediatric glaucoma. Ophthalmology 2009; 116: 30–38.
Noureddin BN, El-Haibi CP, Cheikha A, Bashshur ZF . Viscocanalostomy versus trabeculotomy ab externo in primary congenital glaucoma: 1-year follow-up of a prospective controlled pilot study. Br J Ophthalmol 2006; 90: 1281–1285.
Vold SD . Ab interno trabeculotomy with the trabectome system: what does the data tell us? Int Ophthalmol Clin 2011; 51: 65–81.
Minckler D, Mosaed S, Dustin L, Ms BF, Trabectome Study Group. Trabectome (trabeculectomy-internal approach): additional experience and extended follow-up. Trans Am Ophthalmol Soc 2008; 106: 149–160.
Khitri MR, Mills MD, Ying GS, Davidson SL, Quinn GE . Visual acuity outcomes in pediatric glaucomas. J AAPOS 2012; 16: 376–381.
McPherson SD Jr, McFarland D . External trabeculotomy for developmental glaucoma. Ophthalmology 1980; 87: 302–305.
Broadway DC, Grierson I, Hitchings RA . Local effects of previous conjunctival incisional surgery and the subsequent outcome of filtration surgery. Am J Ophthalmol 1998; 125: 805–818.
Bohnsack BL, Freedman SF . Surgical outcomes in childhood uveitic glaucoma. Am J Ophthalmol 2013; 155: 134–142.
Grajewski AL, Bitrian E, Levin A, Maul EJ . Congenital rubella. In: Weinreb RN, Grajewski A, Papadopoulos M, Grigg J, Freedman S, (eds) Childhood Glaucoma.. WGA Consensus Series – 9 Kugler Publications: Amsterdam, 2013 pp 194–196.
Olsen KE, Huang AS, Wright MM . The efficacy of goniotomy/trabeculotomy in early-onset glaucoma associated with the Sturge-Weber syndrome. J AAPOS 1998; 2: 365–368.
Bayraktar S, Koseoglu T . Endoscopic goniotomy with anterior chamber maintainer: Surgical technique and one year results. Ophthalmic Surg Lasers 2001; 32: 496–502.
Kulkarni SV, Damji KF, Fournier AV, Pan I, Hodge WG . Endoscopic goniotomy: early clinical experience in congenital glaucoma. J Glaucoma 2010; 19: 264–269.
Senft SH, Tomey KF, Traverso CE . Neodymium-YAG laser goniotomy vs surgical goniotomy. A preliminary study in paired eyes. Arch Ophthalmol 1989; 107: 1773–1776.
Barkan O . Surgery of congenital glaucoma; review of 196 eyes operated by goniotomy. Am J Ophthalmol 1953; 36: 1523–1534.
Haas JS . End results of treatment. Trans Am Acad Ophthalmol Otolaryngol 1955; 59: 333–341.
Morin JD, Merin S, Sheppard RW . Primary congenital glaucoma – a survey. Can J Ophthalmol 1974; 9: 17–28.
Luntz MH, Livingston DG . Trabeculotomy ab externo and trabeculectomy in congenital and adult-onset glaucoma. Am J Ophthalmol 1977; 83: 174–179.
Akimoto M, Tanihar H, Negi A, Nagata M . Surgical results of trabeculotomy ab externo for developmental glaucoma. Arch Ophthalmol 1994; 112: 1540–1544.
Dietlein TS, Jacobi PC, Krieglstein GK . Prognosis of primary ab externo surgery for primary congenital glaucoma. Br J Ophthalmol 1999; 83: 317–322.
Anderson DR . Trabeculotomy compared to goniotomy for glaucoma in children. Ophthalmology 1983; 90: 805–806.
Papadopoulos M, Khaw PT . Goniotomy and Trabeculotomy. In Shaarawy T, Sherwood MB, Hitchings RA, Crowston JG, (eds.) Glaucoma. Saunders/Elsevier: Philadelphia, 2009 pp 493–499.
McCann ME, Soriano SG . Anaesthetic neurotoxicity in children. Ophthalmol Int 2013; 8: 26–29.
Chang TC, Cavuoto KM . Anesthesia considerations in pediatric glaucoma management. Curr Opin Ophthalmol. 2014; 25 (2): 118–121.
Girkin CA, Rhodes L, McGwin G, Marchase N, Cogen MS . Goniotomy versus circumferential trabeculotomy with an illuminated microcatheter in congenital glaucoma. J AAPOS 2012; 16: 424–427.
Neely DE . False passage: a complication of 360 degrees suture trabeculotomy. J AAPOS 2005; 9: 396–397.
Verner-Cole EA, Ortiz S, Bell NP, Feldman RM . Subretinal suture misdirection during 360 degrees suture trabeculotomy. Am J Ophthalmol 2006; 141: 391–392.
Mendicino ME, Lynch MG, Drack A, Beck AD, Harbin T, Pollard Z et al. Long-term surgical and visual outcomes in primary congenital glaucoma: 360 degree trabeculotomy versus goniotomy. J AAPOS 2000; 4: 205–210.
Beck AD, Lynn MJ, Crandall J, Mobin-Uddin O . Surgical outcomes with 360-degree suture trabeculotomy in poor-prognosis primary congenital glaucoma and glaucoma associated with congenital anomalies or cataract surgery. J AAPOS 2011; 15: 54–58.
Beck AD, Freedman S, Kammer J, Jin J . Aqueous shunt devices compared to trabeculectomy with mitomycin C for children in the first two years of life. Am J Ophthalmol 2003; 136: 994–1000.
Hill R, Ohanesian R, Voskanyan L, Malayan A . The Armenian Eye Care Project: surgical outcomes of complicated paediatric glaucoma. Br J Ophthalmol 2003; 87: 673–676.
Beauchamp GR, Parks MM . Filtering surgery in children: barriers to success. Ophthalmology 1979; 86: 170–180.
Burke JP, Bowell R . Primary trabeculectomy in congenital glaucoma. Br J Ophthalmol 1989; 73: 186–190.
Fulcher T, Chan J, Lanigan B, well R, O'Keefe M . Long-term follow up of primary trabeculectomy for infantile glaucoma. Br J Ophthalmol 1996; 80: 499–502.
Mandal AK, Walton DS, John T, Jayagandan A . Mitomycin C-augmented trabeculectomy in refractory congenital glaucoma. Ophthalmology 1997; 104: 996–1001.
Azuara-Blanco A, Wilson RP, Spaeth GL, Schmidt CM, Augsburger JJ . Filtration procedures supplemented with mitomycin C in the management of childhood glaucoma. Br J Ophthalmol 1999; 83: 151–156.
Rodrigues AM, Junior AP, Montezano FT, de Arruda Melo PA, Prata J Jr . Comparison between results of trabeculectomy in primary congenital glaucoma with and without the use of mitomycin C. J Glaucoma 2004; 13: 228–232.
Ozkiris A, Tamcelik N . Long-term results of trabeculectomy with different concentrations of mitomycin C in refractory developmental glaucoma. J Pediatr Ophthalmol Strabismus 2005; 42: 97–102.
Waheed MD, Ritterband DC, Greenfeld DS, Liebmann JM, Sidoti PA, Ritch R . Bleb-related ocular infection in children after trabeculectomy with mitomycin C. Ophthalmology 1997; 104: 2117–2120.
Al-Hazmi A, Zwaan J, Awad A, al-Mesfer S, Mullaney PB, Wheeler DT . Effectiveness and complications of MMC use during pediatric glaucoma surgery. Ophthalmology 1998; 105: 1915–1920.
Mandal AK, Bagga H, Nutheti R, Gothwal VK, Nanda AK . Trabeculectomy with or without mitomycin-C for paediatric glaucoma in aphakia and pseudophakia following congenital cataract surgery. Eye 2003; 17: 53–62.
Molteno A . Children with advanced glaucoma treated by draining implants. S Afr Arch Ophthalmol 1973; 1: 55–62.
Fellenbaum PS, Sidoti PA, Heuer DK, Minckler DS, Baerveldt G, Lee PP . Experience with the Baerveldt implant in young patient with complicated glaucomas. J Glaucoma 1995; 4: 91–97.
El Sayed Y, Awadein A . Polypropylene vs silicone Ahmed valve with adjunctive mitomycin C in paediatric age group: a prospective controlled study. Eye 2013; 27: 728–734.
Morad Y, Donaldson CE, Kim YM, Abdolell M, Levin AV . The Ahmed drainage implant in the treatment of pediatric glaucoma. Am J Ophthalmol 2003; 135: 821–829.
Ishida K, Mandal AK, Netland PA . Glaucoma drainage implants in pediatric patients. Ophthalmol Clin North Am 2005; 18: 431–442.
Budenz DL, Gedde SJ, Brandt JD, Kira D, Feuer W, Larson E . Baerveldt glaucoma implant in the management of refractory childhood glaucomas. Ophthalmology 2004; 111: 2204–2210.
Rolim de Moura C, Fraser-Bell S, Stout A, Labree L, Nilfors M, Varma R . Experience with the Baerveldt glaucoma implant in the management of pediatric glaucoma. Am J Ophthalmol 2005; 139: 847–854.
van Overdam KA, de Faber JT, Lemij HG, de Waard PW . Baerveldt glaucoma implant in paediatric patients. Br J Ophthalmol 2006; 90: 328–332.
O’Malley Schotthoefer E, Yanovitch TL, Freedman SF . Aqueous drainage device surgery in refractory pediatric glaucomas: I. Long-term outcomes. J AAPOS 2008; 12: 33–39.
Budenz DL, Barton K, Feuer WJ, Schiffman J, Costa VP, Godfrey DG et alAhmed Baerveldt Comparison Study Group. Treatment outcomes in the Ahmed Baerveldt Comparison Study after 1 year of follow-up. Ophthalmology 2011; 118: 443–452.
Christakis PG, Tsai JC, Kalenak JW, Zurakowski D, Cantor LB, Kammer JA et al. The Ahmed versus Baerveldt study: three-year treatment outcomes. Ophthalmology 2013; 120: 2232–2240.
Tanimoto SA, Brandt JD . Options in pediatric glaucoma after angle surgery has failed. Curr Opin Ophthalmol 2006; 17: 132–137.
El Sayed Y, Awadein A . Polypropylene vs silicone Ahmed valve with adjunctive mitomycin C in paediatric age group: a prospective controlled study. Eye (Lond) 2013; 27: 728–734.
Valimaki J, Tuulonen A, Airaksinen PJ . Outcome of Molteno implantation surgery in refractory glaucoma and the effect of total and partial tube ligation on the success rate. Acta Ophthalmol Scand 1998; 76: 213–219.
Trible JR, Brown DB . Occlusive ligature and standardized fenestration of a Baerveldt tube with and without antimetabolites for early postoperative intraocular pressure control. Ophthalmology 1998; 105: 2243–2250.
Kee C . Prevention of early postoperative hypotony by partial ligation of silicone tube in Ahmed glaucoma valve implantation. J Glaucoma 2001; 10: 466–469.
Park HY, Lee NY, Park CK . Risk factors of shallow anterior chamber other than hypotony after Ahmed glaucoma valve implant. J Glaucoma 2009; 18: 44–48.
Lee JJ, Park KH, Kim DM, Kim TW . Clinical outcomes of Ahmed glaucoma valve implantation using tube ligation and removable external stents. Korean J Ophthalmol 2009; 23: 86–92.
Hill RA, Heuer DK, Baerveldt G, Minckler DS, Martone JF . Molteno Implantation for glaucoma in young patients. Ophthalmology 1991; 98: 1042–1046.
Englert JA, Freedman SF, Cox TA . The Ahmed valve in refractory pediatric glaucoma. Am J Ophthalmol 1999; 127: 34–42.
Molteno AC, Ancker E, van Biljon G . Surgical technique for advanced juvenile glaucoma. Arch Ophthalmol 1984; 102: 51–57.
Nassiri N, Nouri-Mahdavi K, Coleman AL . Ahmed glaucoma valve in children: A review. Saudi J Ophthalmol 2011; 25: 317–327.
Lankaranian D, Reis R, Henderer JD, Choe S, Moster MR . Comparison of single and double thickness processed pericardium patch graft in glaucoma drainage device surgery: a single surgeon comparison of outcome. J Glaucoma 2008; 17: 49–51.
Anand A, Sheh H, Teng CC, Liebmann JM, Ritch R, Tello C . Use of amniotic membrane graft in glaucoma shunt surgery. Ophthal Surg Lasers Imaging 2011; 42: 184–189.
Zaita AH . Long-term experience of patch graft failure after Ahmed glaucoma valve surgery using donor dura and scleral allografts. Ophthal Surg Lasers Imaging 2012; 43: 408–415.
Sidoti PA, Mosny AY, Ritterband DC, Seedor JA . Pars plana insertion of glaucoma drainage implants and penetrating keratoplasty in patients with coexisting glaucoma and corneal disease. Ophthalmology 2001; 108: 1050–1058.
Al-Mobarak F, Khan AO . Two year survival of Ahmed valve implantation in the first 2 years of life with and without intraoperative mitomycin-C. Ophthalmology 2009; 116: 1862–1865.
Kirwan C, O’Keefe M, Lanigan B, Mahmood U . Ahmed valve drainage implant surgery in the management of paediatric aphakic glaucoma. Br J Ophthalmol 2005; 89: 855–858.
Mahdy RA . Adjunctive use of bevacizumab versus mitomycin C with Ahmed valve implantation in the treatment of pediatric glaucoma. J Glaucoma 2011; 20: 458–463.
Tsai JC, Grajewski AL, Parrish RK 2nd . Surgical revision of glaucoma shunt implants. Ophthalmic Surg Lasers 1999; 30: 41–46.
Burgoyne JK, WuDunn D, Lakhani V, Cantor LB . Outcomes of sequential tube shunts in complicated glaucoma. Ophthalmology 2000; 107: 309–314.
Shah AA, WuDunn D, Cantor LB . Shunt revision versus additional tube shunt implantation after failed tube shunt surgery in refractory glaucoma. Am J Ophthalmol 2000; 129: 455–460.
Ou Y, Yu F, Law SK, Coleman AL, Caprioli J . Outcomes of Ahmed glaucoma valve implantation in children with primary congenital glaucoma. Arch Ophthalmol 2009; 127: 1436–1441.
Yang HK, Park KH . Clinical outcomes after Ahmed valve implantation in refractory paediatric glaucoma. Eye (Lond) 2009; 23: 1427–1435.
Sood S, Beck AD . Cyclophotocoagulation versus sequential tube shunt as a secondary intervention following primary tube shunt failure in pediatric glaucoma. J AAPOS 2009; 13: 379–383.
Aminlari A . Cyclocryotherapy in congenital glaucoma. Glaucoma 1981; 3: 331–332.
al Faran MF, Tomey KF, al Mutlaq FA . Cyclocryotherapy in selected cases of congenital glaucoma. Ophthalmic Surg 1990; 21: 794–798.
Wagle NS, Freedman SF, Buckley EG et al. Long-term outcome of cyclocryotherapy for refractory pediatric glaucoma. Ophthalmology 1998; 105: 1921–1926.
Bock CJ, Freedman SF, Buckley EG, Shields MB . Transscleral diode laser cyclophotocoagulation for refractory pediatric glaucomas. J Pediatr Ophthalmol Strabismus 1997; 34: 235–239.
Phelan MJ, Higginbotham EJ . Contact transscleral Nd:YAG laser cyclophotocoagulation for the treatment of refractory pediatric glaucoma. Ophthalmic Surg Lasers 1995; 26: 401–403.
Plager DA, Neely DE . Intermediate-term results of endoscopic diode laser cyclophotocoagulation for pediatric glaucoma. J AAPOS 1999; 3: 131–137.
Sabri K, Vernon SA . Scleral perforation following trans-scleral cyclodiode. Br J Ophthalmol 1999; 83: 502–503.
Hamard P, May F, Quesnot S, Hamard H . La cyclophotocoagulation transsclérale au laser diode dans le traitement des glaucomes réfractaires du sujet jeune. [Trans-scleral diode laser cyclophotocoagulation for the treatment of refractory pediatric glaucoma]. J Fr Ophtalmol 2000; 23: 773–780.
Kirwan JF, Shah P, Khaw PT . Diode laser cyclophotocoagulation: role in the management of refractory pediatric glaucomas. Ophthalmology 2002; 109: 316–323.
Autrata R, Rehurek J . Long-term results of transscleral cyclophotocoagulation in refractory pediatric glaucoma patients. Ophthalmologica 2003; 217: 393–400.
Neely DE, Plager DA . Endocyclophotocoagulation for management of difficult pediatric glaucomas. J AAPOS 2001; 5: 221–229.
Carter BC, Plager DA, Neely DE, Sprunger DT, Sondhi N, Roberts GJ . Endoscopic diode laser cyclophotocoagulation in the management of aphakic and pseudophakic glaucoma in children. J AAPOS 2007; 11: 34–40.
Heinz C, Koch JM, Heiligenhaus A . Transscleral diode laser cyclophotocoagulation as primary surgical treatment for secondary glaucoma in juvenile idiopathic arthritis: high failure rate after short term follow up. Br J Ophthalmol 2006; 90: 737–740.
Beck AD . Primary congenital glaucoma in the developing world. Ophthalmology 2011; 118: 229–230.
Bowman RJ, Dickerson M, Mwende J, Khaw PT . Outcomes of goniotomy for primary congenital glaucoma in East Africa. Ophthalmology 2011; 118: 236–240.
Essuman VA, Braimah IZ, Ndanu TA, Ntim-Amponsah CT . Combined trabeculotomy and trabeculectomy: outcome for primary congenital glaucoma in a West African population. Eye (Lond) 2011; 25: 77–83.
Moore DB, Tomkins O, Ben-Zion I . A review of primary congenital glaucoma in the developing world. Surv Ophthalmol 2013; 58: 278–285.
Edmunds B . New apps to make eyes smart. Ophthalmol Int 2013; 3: 69.
Zhang XL, Du SL, Ge J, Chen WR, Fan Q, Peng SX et al. [Quality of life in patients with primary congenital glaucoma following antiglaucoma surgical management]. Zhonghua Yan Ke Za Zhi 2009; 45: 514–521.
Dada T, Aggarwal A, Bali SJ, Wadhwani M, Tinwala S, Sagar R . Caregiver burden assessment in primary congenital glaucoma. Eur J Ophthalmol 2013; 23: 324–328.
Rahi JS, Tadić V, Keeley S, Lewando-Hundt G, Vision-related Quality of Life Group. Capturing children and young people’s perspectives to identify the content for a novel vision-related quality of life instrument. Ophthalmology 2011; 118: 819–824.
Dada T, Rahi J, Bali SJ, Freedman S . Addendum - Patients, parents and providers as partners in managing childhood glaucoma. In: Weinreb RN, Grajewski A, Papadopoulos M, Grigg J, Freedman S, (eds) Childhood Glaucoma.. WGA Consensus Series – 9 Kugler Publications: Amsterdam, 2013 pp 249–254.
Acknowledgements
Dr Beth Edmunds was supported by an unrestricted grant to OHSU from Research to Prevent Blindness. Professor Sir Peng Tee Khaw was supported in part by the NIHR Biomedical Research Centre Moorfields Eye Hospital and UCL Institute of Ophthalmology, Fight for Sight, Moorfields Special Trustees, Mr John Nolan, Henry Hadaway MBE and the Helen Hamlyn Trust in memory of Paul Hamlyn.
Disclaimer
The views expressed in this publication are those of the authors and not necessarily those of the Department of Health. PTK has received funding for clinical trials by Pfizer, Alcon and Bausch and Lomb.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This has not been previously presented at a meeting.
Rights and permissions
About this article
Cite this article
Papadopoulos, M., Edmunds, B., Fenerty, C. et al. Childhood glaucoma surgery in the 21st Century. Eye 28, 931–943 (2014). https://doi.org/10.1038/eye.2014.140
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2014.140
This article is cited by
-
Effect of Trabeculodescemetic Window Perforation in Deep Sclerectomy on Intraocular Pressure in Primary Congenital Glaucoma
Ophthalmology and Therapy (2024)
-
Efficacy and safety of the PreserFlo implant with mitomycin C in childhood glaucoma after previous failed glaucoma surgeries
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
The associations of self-perception, movement competence, and clinical features of young school-aged children with glaucoma
European Journal of Pediatrics (2023)
-
The PAUL® glaucoma implant: 1-year results of a novel glaucoma drainage device in a paediatric cohort
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
Profile of primary childhood glaucoma at a child eye health tertiary facility in Malawi
BMC Ophthalmology (2022)