Abstract
Purpose
To examine the effects of caffeinated coffee consumption on intraocular pressure (IOP), ocular perfusion pressure (OPP), and ocular pulse amplitude (OPA) in those with or at risk for primary open-angle glaucoma (POAG).
Methods
We conducted a prospective, double-masked, crossover, randomized controlled trial with 106 subjects: 22 with high tension POAG, 18 with normal tension POAG, 20 with ocular hypertension, 21 POAG suspects, and 25 healthy participants. Subjects ingested either 237 ml of caffeinated (182 mg caffeine) or decaffeinated (4 mg caffeine) coffee for the first visit and the alternate beverage for the second visit. Blood pressure (BP) and pascal dynamic contour tonometer measurements of IOP, OPA, and heart rate were measured before and at 60 and 90 min after coffee ingestion per visit. OPP was calculated from BP and IOP measurements. Results were analysed using paired t-tests. Multivariable models assessed determinants of IOP, OPP, and OPA changes.
Results
There were no significant differences in baseline IOP, OPP, and OPA between the caffeinated and decaffeinated visits. After caffeinated as compared with decaffeinated coffee ingestion, mean mm Hg changes (±SD) in IOP, OPP, and OPA were as follows: 0.99 (±1.52, P<0.0001), 1.57 (±6.40, P=0.0129), and 0.23 (±0.52, P<0.0001) at 60 min, respectively; and 1.06 (±1.67, P<0.0001), 1.26 (±6.23, P=0.0398), and 0.18 (±0.52, P=0.0006) at 90 min, respectively. Regression analyses revealed sporadic and inconsistent associations with IOP, OPP, and OPA changes.
Conclusion
Consuming one cup of caffeinated coffee (182 mg caffeine) statistically increases, but likely does not clinically impact, IOP and OPP in those with or at risk for POAG.
Similar content being viewed by others
Introduction
Primary open-angle glaucoma (POAG) is the most common type of glaucoma and a major cause of blindness worldwide.1 It is characterized by optic nerve damage, resulting in irreversible vision loss. Risk factors for the development and progression of POAG and open-angle glaucoma (OAG) include elevated intraocular pressure2, 3, 4, 5, 6, 7, 8, 9 (IOP) and low ocular perfusion pressure (OPP).10, 11, 12, 13, 14, 15, 16, 17, 18 As IOP and OPP may be influenced by modifiable lifestyle activities,19 identifying such factors may guide the development of preventative measures for POAG.
Caffeine consumption is a modifiable lifestyle activity that warrants investigation as it is widespread among older adults at risk for POAG (ie, 80% of US adults >50 years old ingest caffeine daily)20 and changing dietary habits is a relatively inexpensive measure that could prevent the development of a comparatively costly disease.21, 22, 23 Caffeinated coffee deserves particular examination because it is the primary source of dietary caffeine and reportedly the most commonly ingested beverage wordwide.24
Advice regarding caffeine consumption varies because of controversy regarding the degree to which acute caffeine intake influences IOP levels. Several studies found IOP changes to be negligible,25, 26, 27, 28, 29, 30 whereas others report increases of approximately 1–4 mm Hg.31, 32, 33, 34, 35, 36
A recent meta-analysis37 called for more high-quality randomized clinical trials (RCTs) to better assess caffeine's effects on IOP in those with or at risk for glaucoma and in older subjects. Most RCTs investigating caffeine intake and IOP have examined healthy subjects25, 28, 29, 33, 34 with a mean age of 25 years.37 Only two RCTs31, 32 have enrolled glaucoma and glaucoma suspect patients, and neither disclosed the subjects' ages. Furthermore, neither trial31, 32 was participant-masked, and one study31 was not investigator-masked.
Two trials28, 29 have investigated caffeine's effects on OPP. Although both were double-masked, only young (24–30.7 mean years old), healthy participants were enrolled. No studies have assessed caffeine's effects on ocular pulse amplitude (OPA), a surrogate of choroidal perfusion.
To the best of our knowledge, there are no prospective, double-masked RCTs that evaluate caffeine's effects on IOP, OPP, or OPA in those with or at risk for glaucoma. We report the results of a prospective, double-masked crossover RCT to assess the relationship between caffeinated coffee consumption and IOP, OPP, and OPA in patients with or at risk for POAG who are at least 40 years of age.
Materials and methods
Study participants
The study was conducted at Massachusetts Eye and Ear Infirmary (MEEI) from November 2010 to August 2011. Participants were recruited from the glaucoma and comprehensive ophthalmology clinics, and healthy subjects were additionally recruited from MEEI employees and spouses of enrolled subjects.
All participants were 40–89 years old and demonstrated in both eyes: (1) open angles on Van Herick screening or gonioscopy; and (2) slit lamp biomicroscopy showing no secondary causes of glaucoma. Subjects were excluded if they had a history of cardiac arrhythmia, liver or kidney damage, allergy to topical anaesthetic, or ocular trauma. Of the 106 participants, 103 were European-derived Caucasians and 3 were Hispanic Caucasians.
Patients were categorized into one of the five study groups: high tension POAG (HTG), normal tension POAG (NTG), POAG suspect, ocular hypertension (OHTN), and healthy. Categorization was based on visual fields (VFs), IOP history, and cup-disc ratios (CDRs). VF: Consistent with the Primary Open-Angle Glaucoma Genes and Environment Study,38 POAG eyes demonstrated either: (A) the same glaucomatous VF defects (nasal step, nasal depression, paracentral scotoma, arcuate, or temporal wedge) on at least two reliable Humphrey VFs (HVFs); or (B) a glaucomatous VF defect on one reliable HVF with a CDR≥0.7. Reliable fields had a fixation loss rate ≤33% and false-positive and -negative rate ≤20%. VF defects were either early or moderate based on the glaucoma staging system.39 POAG suspects, OHTN, and healthy subjects demonstrated no or minimal VF defect(s) per the glaucoma staging system39 on all available, reliable HVF(s) for both eyes. IOP HISTORY: HTG and OHTN patients had a history of IOP ≥22 mm Hg in at least one eye and in the study eye, whereas NTG and healthy patients had no history of IOP ≥22 mm Hg in both eyes. POAG suspects had no IOP restrictions. CDR: POAG suspects demonstrated a ≥0.7 CDR in at least one eye or ≥0.2 CDR asymmetry between eyes. OHTN and healthy subjects had ≤0.6 CDRs in both eyes and ≤0.1 CDR asymmetry between eyes.
One eye per patient was enrolled. Eyes were excluded if they had: (1) anterior segment laser procedure or cataract surgery in the prior 6 months; (2) glaucoma surgery; or (3) impending glaucoma laser or surgery. When both eyes of a subject were eligible, the eye with the greater CDR was selected in POAG suspects and the right eye was chosen in all other subjects.
A total of 1227 patients were screened for eligibility. In all, 963 patients were ineligible, 152 declined to participate, and 112 enrolled in the study (Figure 1). Six participants dropped out after the first study visit. Only data from the 106 participants who completed both study visits were included in the final analyses.
This study was approved by the MEEI Human Research Committee and registered on http://www.clinicaltrials.gov, identifier NCT01364207. All subjects gave written informed consent before study participation. All applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed.
Study design
This clinical trial was a prospective, randomized, double-masked crossover study. Enrolled study patients were randomized in blocks of 10 by computer-generated numbers (http://www.randomizer.org) to receive 237 ml of caffeinated or decaffeinated coffee on their first study visit and the alternate beverage on their second visit. Pharmacy staff not involved in the trial at a separate site generated and maintained the randomization list, prepared the coffee in a standardized manner, and poured the coffee into individual thermoses labelled only with the patient's initials, which were then provided to study staff. Study staff and subjects had no information regarding the content of the thermoses and were masked to subject assignment.
Harvard Biological and Chemical Laboratories (Harvard University, Cambridge, Massachusetts) determined the caffeine levels in the study coffee using liquid chromatography mass spectrometry. Each 237 ml cup of caffeinated and decaffeinated coffee contained 182 and 4 mg of caffeine, respectively, similar to caffeine levels documented in other RCTs examining coffee and IOP.31, 32
All visits commenced between 8:00 and 10:00 hours, and each participant started each of their study visits at the same time. The second study visit was completed 2 days–4 weeks after the first. At each visit, participants ingested the coffee with 22 ml of cream in ≤15 min under direct study staff observation. Subjects were required to: (1) abstain from all sources of caffeine, other than the study coffee, starting at 12:01 hours the day of each visit and ending immediately after each visit; (2) continue to take all medications including any glaucoma medications with no medication changes on and between the study visits; (3) take all morning medications at least 1 h and at the same time before each study visit; (4) abstain from fluids or foods other than the study coffee during each visit. Additionally, current smokers (n=6) refrained from smoking during and at least 1 h before each visit. Compliance with these requirements was ascertained by subject self-report.
During each study visit, masked trained study staff measured IOP, OPA, heart rate (HR), and blood pressure (BP) before and 60 and 90 min after coffee ingestion, similar to time points used in other RCTs examining coffee and IOP.31, 32, 34 Three quality 1 or 2 Pascal Dynamic Contour Tonometer (Ziemer Ophthalmic Systems Group Company, Port, Switzerland) measurements of IOP, OPA, and HR were taken at each time point. Two seated brachial BP measurements were taken at each time point using the digital BP monitor Omron HEM-907XL Pro (Omron Corporation, Tokyo, Japan), with a third taken if either the systolic BP (SBP) or diastolic BP (DBP) in the first two measurements differed by >10 mm Hg. The mean of the three IOP, OPA, HR; and 2–3 BP measurements taken per time point was used in data analyses. OPP was calculated as 2/3*[DBP+1/3*(SBP−DBP)]–IOP.16, 18
Subjects completed a validated questionnaire40 regarding their daily caffeine intake. Additionally, the following was recorded for each: (1) participant—age; gender; hypertension; diabetes; family history of glaucoma in a biological parent, sibling, or child; body mass index calculated as kg/m2; hypertension medications; and (2) study eye—spherical equivalent calculated as sphere+(0.5*cylinder), glaucoma laser(s), cataract surgery, glaucoma medications, and central corneal thickness as measured with a PachPen pachymeter (Accutome Inc., Malvern, PA, USA).
Statistical analysis
A P-value <0.05 was statistically significant. Pooling all groups together, comparisons between the caffeinated and decaffeinated visits were analysed using paired t-tests. Comparisons among groups were assessed by one-way analysis of variance and χ2 test for independence. If the one-way analysis of variance tests revealed significant differences, follow-up Tukey–Kramer Multiple Comparison tests among the groups were conducted. Linear and logistic regression models assessed for determinants of IOP, OPP, and OPA changes.
For the primary hypothesis, assuming an alpha error of 5% and a power of 90%, a minimum sample size of 17 subjects per group was required to detect the smallest RCT-reported IOP change after caffeinated coffee ingestion (∼1 mm Hg).31, 32, 33, 34
Sample size calculations were conducted using http://www.dssresearch.com/KnowledgeCenter/toolkitcalculators/samplesizecalculators.aspx. All data analyses except regression analyses were performed using GraphPad InStat Version 3.1a (GraphPad Software Inc., La Jolla, CA, USA). Regression analyses were conducted with SAS version 9.2 (SAS Institute Inc., Cary, NC, USA).
Results
The demographic and ocular features of the subjects who completed the trial are described in Table 1. The five groups differed significantly in terms of the percentage with a family history of glaucoma (P=0.0393), percentage on glaucoma medications (P<0.0001), mean number of prescribed glaucoma medications (P<0.0001) and percentage with a history of glaucoma laser procedure(s) (P<0.0001). The HTG group had the highest, and the healthy group generally had the lowest, percentages or numbers of these four features.
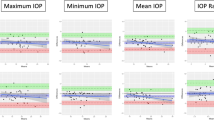
Pooling all groups together, there were no differences in baseline parameters (IOP, OPP, OPA, SBP, DBP, and HR) between the caffeinated and decaffeinated visits (Table 2). However, after caffeinated, as compared with decaffeinated, coffee ingestion all these parameters increased significantly at 60 and 90 min except for HR, which demonstrated no significant changes at both 60 and 90 min. Mean changes (±SD) in IOP, OPP, and OPA after caffeinated, as compared with decaffeinated, coffee consumption at 60 and 90 min were, respectively, in mm Hg: 0.99 (±1.52, P<0.0001) and 1.06 (±1.67, P<0.0001); 1.57 (±6.40, P=0.0129) and 1.26 (±6.23, P=0.0398); and 0.23 (±0.52, P<0.0001) and 0.18 (±0.52, P=0.0006). Comparison of the changes in IOP, OPP, OPA, SBP, DBP, and HR at 60 vs 90 min after caffeinated, as compared with decaffeinated, coffee intake revealed no statistically significant differences (data not shown).
We compared IOP, OPP, and OPA between the five groups (Table 3). At baseline, each of these parameters differed significantly between the groups. However, the changes in these parameters generally did not differ significantly between the five groups after caffeinated, as compared with decaffeinated, coffee ingestion at 60 and 90 min. The exception was the change in IOP at 60 min (±SD) in mm Hg: the HTG group demonstrated a significantly smaller change (0.19 ±1.09) compared with the POAG suspect (1.51 ±1.53, P<0.05) and OHTN (1.61 ±1.85, P<0.05) groups.
We examined each of the 106 participants' changes in IOP, OPP, and OPA at 90 min after caffeinated, as compared with decaffeinated, coffee consumption. With respect to ΔIOP in mm Hg, 33 subjects had ≥+2, 71 had between +2 and −2, and 2 had ≤−2. In terms of ΔOPP in mm Hg, 7 participants had ≥+10, 94 had between +10 and −10, and 5 had ≤−10. With regards to ΔOPA in mm Hg, 7 subjects had ≥+1, 96 had between +1 and −1, and 3 had ≤−1. Of the participants with ΔIOP ≥+2 mm Hg, five also demonstrated ΔOPP ≤−5 mm Hg and zero demonstrated ΔOPP ≤−10 mm Hg. The 60 min results are similar.
Multiple linear and logistic regression models (data not shown) assessed determinants of IOP, OPP, and OPA changes at 60 and 90 min. There were no consistently statistically significant associations between any of the covariates of interest (age, gender, body mass index, hypertension, diabetes, glaucoma status, family history of glaucoma, baseline IOP, daily caffeine intake) and outcome parameters.
Discussion
In this double-masked crossover RCT, we demonstrated that consuming 237 ml of caffeinated, as compared with decaffeinated, coffee significantly increases, at 60 and 90 min: IOP by ∼1 mm Hg, OPP by ∼1.25–1.50 mm Hg, and OPA by ∼0.2 mm Hg. On average, the small increase in IOP was offset by an increase in OPP of similar magnitude. These one-time, modest and presumably transient increases in IOP and OPP are unlikely to impact conversion to or progression of glaucoma. However, a small minority of subjects demonstrated larger and potentially clinically significant increases in IOP or decreases in OPP after caffeinated, as compared with decaffeinated, coffee consumption. Our multivariate analyses, which may be underpowered, failed to reveal consistently significant determinants of changes in IOP, OPP, or OPA. Also, owing to the few studies examining OPA and clinical outcomes,41, 42 it is unclear whether the OPA changes observed in our trial are clinically significant. However, the absence of a decrease in OPA, within the context of slight increases in IOP and OPP, is consistent with our overall results.
Our IOP findings are consistent with those reported in Higginbotham et al32 who examined glaucoma and glaucoma suspect subjects in an investigator-masked RCT and also found a statistically but not clinically significant IOP elevation after caffeinated coffee consumption. Our OPP results differ from those reported in two double-masked studies, which found no change in OPP after caffeine tablet ingestion in 10 or 14 young (age range 20–44 years), healthy subjects.28, 29 However, these two studies may be underpowered to detect a statistically significant change in OPP and the studies' results may not be generalized to older patients and those with or at risk for glaucoma. Although no prior studies have investigated the effects of caffeine consumption on OPA, our baseline OPA results are consistent with previous reports.41, 42, 43 Our SBP and DBP increases are consistent with the BP changes after acute caffeine intake documented in the literature.29, 31, 32, 34, 44 Our HR results are consistent with those reported in other RCTs investigating the effects of acute caffeine intake.28, 29, 32
Caffeine may increase IOP through several possible mechanisms. First, as a phosphodiesterase inhibitor, caffeine increases intracellular cyclic AMP,45 which may increase aqueous humour (AqH) formation. However, evidence suggests that inhibition of phosphodiesterase activity does not occur with the caffeine blood levels achieved from 2–3 cups of coffee.46 Second, one investigator theorized34 that caffeine's adenosine receptor antagonist effect could inhibit AqH outflow by decreasing smooth muscle tone in the filtration apparatus, leading to trabecular fenestrae closure. However, Kurata et al47 demonstrated in beagle dogs that caffeine's IOP elevating effects may be due to increased AqH formation and not through the inhibition of AqH drainage through the trabecular meshwork. Third, caffeine's adenosine receptor blockade46, 48, 49 is thought to be responsible for caffeine's well-known BP-elevating effect,50, 51, 52, 53 which could increase the hydrostatic pressure for AqH formation. In rats intravenously injected with caffeine, ultrastructural changes in the non-pigmented ciliary epithelium were observed, suggesting AqH transportation enhancement.54 Additionally, acute caffeine may increase BP before causing IOP elevations.34 Although our study was not designed to determine the mechanism of IOP change after caffeine consumption, the increases in SBP, DBP, and OPP we observed lend support to the third proposed mechanism. It is possible that caffeine may increase OPP and OPA also through the inhibition of adenosine receptors, resulting in reduced vasodilation and increased BP.
Our study has several strengths. It is the largest RCT to investigate the relationship between caffeine intake and IOP. It is also the first double-masked RCT that examines IOP, and the first study to assess OPP, after caffeine intake in those with or at risk of glaucoma. It is also the first trial to examine OPA after caffeine consumption. Other strengths include the wider 40–89-year-old age range and older 64-year-old mean age of our subjects, compared with the 20–44-year-old age range and approximately 25 year mean age of subjects in the other trials combined,25, 28, 29, 33, 34, 37 as the risk of POAG increases after age 40. The study's crossover design minimized individual variations, enhancing its power. Unlike other RCTs, we did not exclude subjects on antiglaucoma medications,25, 28, 29, 31, 33, 34 on systemic medications,25, 31 with a history of cataract surgery or glaucoma laser procedure before the 6 months preceding the study,25, 28, 31, 32, 33, 34 with systemic hypertension,25, 29, 31, 34 with diabetes,25, 29 who currently smoke,29, 33 who have a family history of glaucoma33, 34 and who ingest beyond a certain daily level of caffeine.25, 29 The absence of these exclusions enhanced the generalizability of our results.
Our study has some limitations. We did not determine the full duration of the IOP, OPP, and OPA elevations observed in our trial. Owing to feasibility concerns regarding the participants' time constraints, our study's time frame was limited to 90 min after coffee ingestion, similar to or longer than the time frames employed by most RCTs examining caffeine consumption and IOP.25, 29, 31, 32, 34 Our findings of statistically significant increases in IOP, OPP,and OPA at 60 and 90 min, as well as no significant differences in the changes in outcome parameters at 60 vs 90 min, suggest that the outcome parameter elevations may have continued beyond 1.5 h. Our results are consistent with those reported in Avisar et al31 and Higginbotham et al,32 who both demonstrated statistically significant IOP elevations at 90 min after caffeinated coffee intake but did not monitor IOP beyond this time point. Adams and Brubaker55 found no significant difference in IOP 4 h after caffeine ingestion, suggesting that caffeine's effects on IOP is transient. Caffeine levels generally peak 30–120 min after oral intake and caffeine's half-life is 3–6 h.44 Caffeine's BP-elevating effects typically occur within 30 min, peak in 1–2 h and may persist for more than 4 h.44 Thus, the outcome parameters increases observed in our trial possibly persisted beyond 1.5 h and declined to baseline within hours afterwards.
Other limitations of our study include our eligibility criteria. Our results may not be applicable to non-Caucasians; those with secondary glaucoma or glaucoma surgery; eyes with advanced glaucoma; those non-adherent with their glaucoma medications; and those with impending glaucoma laser or surgery.
Further investigation into the determinants of IOP, OPP, and OPA changes after caffeine intake is warranted, as caffeine may not be recommended for the minority of our study subjects who demonstrated potentially clinically significant changes in outcome parameters. More work is needed to elucidate the duration of outcome measure changes from one cup of coffee. Future trials can investigate the possibility that repeated exposure to caffeine throughout the day may cause sustained, clinically significant changes in IOP, OPP, and OPA in those with or at risk for glaucoma. The average American daily coffee consumption is about 3.5 cups56 and no trials have examined repeated acute caffeine ingestion in those with or at risk for glaucoma. Okimi et al33 did demonstrate that IOP levels were statistically increased at 3 h after young, healthy participants ingested four cups of caffeinated coffee within an hour. However, consuming 946 ml of coffee within 60 min likely does not mimic the drinking habits of the average person, and the study's results may not be applicable to older patients or those with or at risk for glaucoma. Additionally, coffee consumption has been associated with elevated IOP in OAG patients in a cross-sectional study.57 Kang et al58 found that caffeine intake may be a risk factor for incident HTG for those with a family history of glaucoma. Our study did not find that the ingestion of one cup of caffeinated coffee adversely effected IOP, OPP, or OPA among participants with a family history of glaucoma. Perhaps, a larger sample size and/or a higher level of caffeinated coffee consumption are needed to observe such effects.
We exposed subjects to caffeinated coffee to replicate realistic and clinically relevant scenarios. Our study was not designed or able to assess which caffeinated coffee components were responsible for the outcome parameter changes we observed. Non-caffeine components of caffeinated coffee could contribute to the IOP effects we report. In fact, negligible changes in IOP were found in three trials examining oral caffeine (vs placebo) tablets in healthy subjects25, 28, 29 and in a study investigating the effects of caffeine topical drops in five subjects.30 Thus, as Li et al37 noted, more study of the mechanism by which caffeine mediates its effects on ocular parameters is needed.
In summary, in this first double-masked RCT assessing IOP, OPP, and OPA after caffeinated coffee consumption in those with or at risk for POAG, we found that one cup of caffeinated (182 mg caffeine), as compared with decaffeinated (4 mg caffeine), coffee statistically increases but likely does not clinically impact IOP or OPP for the majority of study participants.

References
Quigley H . Number of people with glaucoma worldwide. Br J Ophthalmol 1996; 80: 389–393.
Nemesure B, Honkanen R, Hennis A, Wu SY, Leske MC . Incident open-angle glaucoma and intraocular pressure. Ophthalmology 2007; 114: 1810–1815.
Leske MC, Connell AMS, Wu S-Y, Nemesure B, Li X, Schachat A et al. Incidence of open-angle glaucoma: the Barbados Eye Studies. Arch Ophthalmol 2001; 119: 89–95.
Gordon MO, Beiser JA, Brandt JD, Heuer DK, Higginbotham EJ, Johnson CA et al. The Ocular HypertensionTreatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol 2002; 120: 714–720.
The AGIS Investigators. The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol 2000; 130: 429–440.
Leske MC, Heijl A, Hussein M, Bengtsson B, Hyman L, Komaroff E . Factors for glaucoma progression and the effect of treatment: the early manifest glaucoma trial. Arch Ophthalmol 2003; 121: 48–56.
Le A, Mukesh BN, McCarty CA, Taylor HR . Risk factors associated with the incidence of open-angle glaucoma: the Visual Impairment Project. Invest Ophthalmol Vis Sci 2003; 44: 3783–3789.
de Voogd S, Ikram K, Wolfs RCW, Jansonius NM, Hofman A, de Jong PTVM . Incidence of open-angle glaucoma in a general elderly population: the Rotterdam Study. Ophthalmol 2005; 112: 1487–1493.
Cedrone C, Mancino R, Ricci F, Cerulli A, Culasso F, Nucci C . The 12-year incidence of glaucoma and glaucoma-related visual field loss in Italy: the Ponza Eye Study. J Glaucoma 2012; 21: 1–6.
Tielsch JM, Katz J, Sommer A, Quigley HA, Javitt JC . Hypertension, perfusion pressure, and primary open-angle glaucoma: a population-based assessment. Arch Ophthalmol 1995; 113: 216–221.
Leske MC, Connell AM, Wu SY, Hyman LG, Schachat MD . Risk factors for open-angle glaucoma. The Barbados Eye Study. Arch Ophthalmol 1995; 113: 918–924.
Bonomi L, Marchini G, Marraffa M, Bernardi P, Morbio R, Varotto A . Vascular risk factors for primary open angle glaucoma: the Egna-Neumarkt Study. Ophthalmology 2000; 107: 1287–1293.
Quigley HA, West SK, Rodriguez J, Munoz B, Klein R, Snyder R . The prevalence of glaucoma in a population-based study of Hispanic subjects: Proyecto VER. Arch Ophthalmol 2001; 119: 1819–1826.
Hulsman CA, Vingerling JR, Hofman A, Witteman JC, Jong PT . Blood pressure, arterial stiffness, and open-angle glaucoma: the Rotterdam study. Arch Ophthalmol 2007; 125: 805–812.
Leske MC, Wu SY, Nemesure B, Hennis A . Incident open-angle glaucoma and blood pressure. Arch Ophthalmol 2002; 120: 954–959.
Leske MC, Wu SY, Hennis A, Honkanen R, Nemesure B . BESs Study Group. Risk factors for incident open-angle glaucoma: the Barbados Eye Studies. Ophthalmology 2008; 115: 85–93.
Leske MC, Heijl A, Hyman L, Bengtsson B, Dong L, Yang Z et al. Predictors of long-term progression in the early manifest glaucoma trial. Ophthalmology 2007; 114: 1965–1972.
Zheng Y, Wong TY, Mitchell P, Friedman D, Mingguang H, Aung T . Distribution of ocular perfusion pressure and its relationship with open-angle glaucoma: the Singapore Malay Eye Study. Invest Ophthalmol Vis Sci 2010; 51: 3399–3404.
Pasquale LR, Kang JH . Lifestyle, nutrition and glaucoma. J Glaucoma 2009; 18: 423–428.
Massey LK . Caffeine and the elderly. Drugs Aging 1998; 13: 43–50.
Traverso CE, Walt JG, Kelly SP, Hommer AH, Bron AM, Denis P et al. Direct costs of glaucoma and severity of the disease: a multinational long term study of resource utilisation in Europe. Br J Ophthalmol 2005; 89: 1245–1249.
Lee PP, Walt JG, Doyle JJ, Kotak SV, Evans SJ, Budenz DL et al. A multicenter, retrospective pilot study of resource use and costs associated with severity of disease in glaucoma. Arch Ophthalmol 2006; 124: 12–19.
Gieser DK, Tracy Williams R, O'Connell W, Pasquale LR, Rosenthal BP, Walt JG et al. Costs and utilization of end-stage glaucoma patients receiving visual rehabilitation care: a US multisite retrospective study. J Glaucoma 2006; 15: 419–425.
Coffee Statistics Report 2011. http://www.coffee-statistics.com/coffee_statistics_ebook.html. accessed 25 May 2011.
Ozkan B, Yuksel N, Anik Y, Altintas O, Demirci A, Caglar Y . The effect of caffeine on retrobulbar hemodynamics. Curr Eye Res 2008; 33: 804–809.
Ricklefs G . Studies on the ways of life of glaucoma patients. Doc Ophthalmol 1968; 25: 43–99.
Ricklefs G, Pohls EU . Effect of caffeine containing tablets and Coca-Cola on the intraocular pressure of patients without glaucoma and patients with regulated glaucoma. Klin Monatsbl Augenheilkd 1969; 154: 546–551.
Okuno T, Sugiyama T, Tominaga M, Kojima S, Ikeda T . Effects of caffeine on microcirculation of the human ocular fundus. Jpn J Ophthalmol 2002; 46: 170–176.
Lofti K, Grunwald JE . The effect of caffeine on the human macular circulation. Invest Ophthalmol Vis Sci 1991; 32: 3028–3032.
Chandra P, Gaur A, Varma S . Effect of caffeine on the intraocular pressure in patients with primary open angle glaucoma. Clin Ophthalmol 2011; 5: 1623–1629.
Avisar R, Avisar E, Weinberger D . Effect of coffee consumption on intraocular pressure. Ann Pharmacother 2002; 36: 992–995.
Higginbotham EJ, Kilimanjaro HA, Wilensky JT, Batenhorst RL, Hermann D . The effect of caffeine on intraocular pressure in glaucoma patients. Ophthalmology 1989; 96: 624–626.
Okimi PH, Sportsman S, Pickard MR, Fritsche MB . Effects of caffeinated coffee on intraocular pressure. Appl Nurs Res 1991; 4: 72–76.
Ajayi OB, Ukwade MT . Caffeine and intraocular pressure in a Nigerian population. J Glaucoma 2001; 10: 25–31.
Graeber W . On the effect of caffeine on intraocular pressure in surgically or conservatively managed simple chronic glaucoma. Klin Monatsbl Augenheilkd 1968; 152: 357–650.
Makabe R . Uber die Reaktionsdifferenz von Normal-und Glaucomaugen and Provokationstest. Ophthalmologica 1970; 161: 460–465.
Li M, Wang M, Guo W, Wang J, Sun X . The effect of caffeine on intraocular pressure: a systematic review and meta-analysis. Graefes Arch Clin Exp Ophthalmol 2011; 249: 435–442.
The Primary Open-Angle Glaucoma Genes and Environment (GLAUGEN) Study. Study Accession: phs000308.v1.p1. www.ncbi.nlm.nih.gov/gap?term=glaugen. accessed 29 March 2011.
Mills RP, Budenz DL, Lee PP, Noecker RJ, Walt JG, Siegartel LR et al. Categorizing the stage of glaucoma from pre-diagnosis to end-stage disease. Am J Ophthalmol 2006; 141: 24–30.
Caffeine Questionnaire. 2004; Fred Hutchinson Cancer Research Center. www.phenxtoolkit.org. accessed 20 May 2011, Ver 4.4.
Schweenn O, Troost R, Vogel A, Grus F, Beck S, Pfeiffer N . Ocular pulse amplitude in patients with open angle glaucoma, normal tension glaucoma, and ocular hypertension. Br J Ophthalmol 2002; 86: 981–984.
Vulsteke C, Stalmans I, Fieuws S, Zeyen T . Correlation between ocular pulse amplitude measured by dynamic contour tonometer and visual field defects. Graefes Arch Clin Exp Ophthalmol 2008; 246: 559–565.
Stalmans I, Harris A, Vanbellinghen V, Zeyen T, Siesky B . Ocular pulse amplitutde in normal tension and primary open angle glaucoma. J Glaucoma 2008; 17: 403–407.
Mort JR, Kruse HR . Timing of blood pressure measurement related to caffeine consumption. Ann Pharmacother 2008; 42: 105–110.
American Hospital Formulary Service – drug information. American Society of Health System Pharmacists: Bethesda, MD, 2006; 2431–2432.
Nurminen M-L, Niittynen L, Korpela R, Vapaatalo H . Coffee caffeine and blood pressure: a critical review. Eur J Clin Nutr 1999; 53: 831–839.
Kurata K, Fujimoto H, Tsukuda R, Suzuki T, Ando T, Tokuriki M . Aqueous humor dynamics in beagle dogs with caffeine-induced ocular hypertension. J Vet Med Sci 1998; 60: 737–739.
James JE . Critical review of dietary caffeine and blood pressure: a relationship that should be taken more seriously. Psychosom Med 2004; 66: 63–71.
Haller CA . Caffeine. In: Olson KR (ed) Poisoning and drug overdose. 5th ed. New York: Lange Medical Books/McGraw-Hill: New York, 2007, pp 142–143.
Fuller RW, Maxwell DL, Conradson T-BG, Dixon CMS, Barnes PJ . Circulatory and respiratory effects of infused adenosine in conscious man. Br J Pharmacol 1987; 24: 309–317.
Smits P, Boekema P, De Abreu R, Thien T, van't Laar A . Evidence for an antagonism between caffeine and adenosine in the human cardiovascular system. J Cardiovasc Pharmacol 1987; 10: 136–143.
Coney AM, Marshall JM . Role of adenosine and its receptors in the vasodilation induced in the cerebral cortex of the rat by systemic hypoxia. J Physiol 1998; 509: 507–518.
Hartley TR, Lovallo WR, Whitsett TL, Sung BH, Wilson MF . Caffeine and stress: implications for risk, assessment, and management of hypertension. J Clin Hypertens 2001; 3: 354–361.
Kurata K, Maeda M, Nishida E, Tsukuda R, Suzuki T, Ando T et al. Relationship between caffeine induced ocular hypertension and ultrastructure changes of nonpigmented ciliary epithelial cells in rats. J Toxicol Sci 1997; 22: 447–454.
Adams BA, Brubaker RF . Caffeine has no clinically significant effect on aqueous humor flow in the normal human eye. Ophthalmology 1990; 8: 1030–1031.
Raebel MA, Black J . The caffeine controversy: what are the facts? Hospital Pharm 1984; 19: 257–267.
Chandrasekaran S, Rochtchina E, Mitchell P . Effects of caffeine on intraocular pressure. J Glaucoma 2005; 14: 504–507.
Kang JH, Willett WC, Rosner BA, Hankinson SE, Pasquale LR . Caffeine consumption and the risk of primary open-angle glaucoma: a Prospective Cohort Study. Invest Ophthalmol Vis Sci 2008; 49: 1924–1931.
Acknowledgements
This work was supported by a Fight for Sight Postdoctoral Grant (Angela V Turalba). Aliya Z Jiwani is funded by a Doris Duke Charitable Foundation One-Year Clinical Research Fellowship and a Yale School of Medicine Summer Fellowship. Louis R Pasquale is supported by a Research to Prevent Blindness Physician Scientist Award, Harvard Medical School Ophthalmology Scholar Award, and an Allergan Horizon Award.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work was presented as a poster at the American Glaucoma Society Meeting in New York City on 3 March 2012.
Rights and permissions
About this article
Cite this article
Jiwani, A., Rhee, D., Brauner, S. et al. Effects of caffeinated coffee consumption on intraocular pressure, ocular perfusion pressure, and ocular pulse amplitude: a randomized controlled trial. Eye 26, 1122–1130 (2012). https://doi.org/10.1038/eye.2012.113
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2012.113
Keywords
This article is cited by
-
Effects of caffeine on intraocular pressure are subject to tolerance: a comparative study between low and high caffeine consumers
Psychopharmacology (2019)
-
The Role of Diet in Glaucoma: A Review of the Current Evidence
Ophthalmology and Therapy (2018)
-
Caffeine intake is associated with pupil dilation and enhanced accommodation
Eye (2017)
-
Modifiable factors in the management of glaucoma: a systematic review of current evidence
Graefe's Archive for Clinical and Experimental Ophthalmology (2017)
-
The effect of flammer-syndrome on retinal venous pressure
BMC Ophthalmology (2014)