Abstract
Objective
To describe the pre- and postoperative features of the visible iris sign (VIS), which is the apparent visibility of iris colour through a closed upper eyelid, in patients undergoing anterior approach surgery for severe involutional aponeurotic ptosis, and to assess its effect on postoperative outcome.
Design
Prospective, comparative interventional case series.
Methods
Prospective series of all patients undergoing surgery for severe involutional aponeurotic ptosis during a 16-month period at a single centre.
Inclusion criteria
Severe involutional ptosis (upper eyelid margin reflex distance (MRD) ≤1 mm) treated by anterior-approach surgery.
Main outcome measures
Presence of VIS, type of ptosis (primary or recurrent), preoperative MRD, levator function and skin crease height, documented unusual intra-operative findings, postoperative complications, and follow-up time.
Results
Of 133 procedures for involutional aponeurotic ptosis, 96 procedures (56 patients) were included in the study. In total, 12 patients (21%, 12/56, 2 males, and 10 females) had been identified as having VIS preoperatively. In order to avoid any selection bias, only patients with severe degree of ptosis were included in the two groups with the two groups being alike in the preoperative lid height, levator function or the skin crease. In the VIS group, 55% (12/22) had a thinned, significantly retracted levator aponeurosis and a thin tarsus prone to full-thickness suture passes (36.3%, 8/22) during aponeurosis reattachment. Immediate persistent overcorrection during surgery was seen in three procedures, with one patient having an under corrected outcome when treated with a hang-back suture. In the non-VIS group, no patients were documented intra-operatively, as having significant retraction of the levator aponeurosis. However, 14% (10/74) of the eyelids were recorded as having a very attenuated levator and one patient (3%, 1/44) was noted to have a floppy tarsus that was difficult to suture. The total incidence of intra-operative difficulties during surgery were 78% in the VIS group and 22% in the non-VIS group. Mean postoperative follow-up was 22 weeks. (median 18, range 12–64). The overall success rates were 63.6% (14/22) in the VIS group, compared with 77.0% (57/74) in the non-VIS group (P=0.260). After excluding cases undergoing concurrent blepharoplasty and non-caucasions, success rates were 57.1% (4/7) and 69.2% (9/13) in the VIS and non-VIS groups, respectively (P=0.598). All failures were because of under-correction.
Conclusion
The VIS is a clinical sign of severe involutional ptosis. Patients with VIS have one or more features, including a retracted levator aponeurosis, a thinned tarsus prone to full-thickness suture passes, and a tendency for immediate persistent overcorrection following levator advancement. Preoperative identification of VIS may help in appropriate patient counselling, procedure selection, anticipation of intraoperative difficulties, and possibly further standardisation of future cohorts when evaluating the results of involutional ptosis surgery.
Précis
The authors describe the pre-, intra- and postoperative features of visible iris sign. They discuss the success rates of anterior approach surgery in VIS patients and discuss the contributing factors for a poorer outcome.
Similar content being viewed by others
Introduction
Involutional aponeurotic ptosis is the most commonly acquired ptosis requiring surgical correction, and is defined by several well-known clinical features. These include constant ptosis, good levator function, a high or absent skin crease, increased lid excursion on downgaze, and a thinned eyelid.1, 2, 3
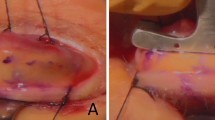
The visible iris sign (VIS) describes patients with involutional aponeurotic ptosis, in whom there is apparent visibility of iris colour through a closed upper eyelid (Figure 1). These signs have been previously alluded to1 and most likely reflect the severe end of the spectrum of clinicopathological changes described for this ptosis,2, 3, 4, 5 which include retraction of an attenuated, dehisced, or detached aponeurosis, retraction of orbital septum and preseptal orbicularis oculi muscle, stretching of the underlying Muller's muscle, and age-related atrophy of soft tissue, all of which will result in an increased translucency of the upper eyelid.
The authors recognised the VIS as a confirmatory sign of aponeurotic ptosis, but more importantly, as a possible predictor of an unpredictable outcome, and in 2005 began prospectively documenting its presence or absence, as well as per- and postoperative features, in all patients with ptosis seen in our unit. We describe the features of VIS in patients undergoing surgery for severe involutional aponeurotic ptosis, and assess its effect on postoperative outcome compared with patients without VIS.
Materials and methods
This was a prospective audit of an interventional case series of all patients undergoing surgery for severe involutional aponeurotic ptosis between October 2005 and February 2007 at the Queen Victoria Hospital, East Grinstead, UK.
Involutional aponeurotic ptosis had been diagnosed in patients with ptosis that was constant in all positions of gaze, good levator function, and a high or absent skin crease. In addition, in an attempt to match controls for severity, only cases with upper eyelid margin reflex distance (MRD) ≤1 mm were included. That is to say, patients with mild–moderate involutional ptosis were excluded. Patients with congenital, myogenic, neurogenic, or traumatic aponeurotic ptosis, inadequate data, including postoperative follow-up data with photographs less than 3 months, and those who underwent posterior-approach surgery were also excluded.
A total of 80 patients undergoing 133 procedures for involutional aponeurotic ptosis repair were identified, however, 96 procedures (56 patients) fulfilled our inclusion criteria. Of those excluded, all mild–moderate ptosis were non-VIS cases.
Patients were further divided into two groups for comparison, those with VIS and those without VIS. To define VIS positivity, the patient was instructed to gently close (but not squeeze) their eyes and two observers (usually the consultant, RM and the fellow) were required to agree that there was apparent visibility of the iris colour and/or part of the circumferential outline of the iris through a closed upper eyelid, with its overlying skin gently stretched both above and below. In dark-skinned individuals or where the iris colour may be hard to define, the presence of the circumferential iris outline is determined by its contrast in relation to adjacent white sclera and VIS was considered positive if at least 2–3 clock-hours of iris-sclera outline were discernable.
In total, 12 patients (mean age 69 years, range 50–87) were identified as having VIS preoperatively and 44 non-VIS (mean age 70 years, range 24–90) patients underwent 22 and 74 ptosis procedures, respectively.
In the VIS group, two patients were of Asian origin (Indian) and in the non-VIS group, two were Asian (Indian) and one Afro-Caribbean. All remaining patients were Caucasian. In the VIS group, iris colour was subjectively defined as blue (5), light brown (3), hazel brown (2), and dark brown (2). In the non-VIS group, iris colour was defined as blue (26), light brown (8), dark brown (7), green (2), and no agreement (1). The majority of procedures (83% VIS, 68% non-VIS) underwent simultaneous bilateral ptosis repairs.
Data collected for comparison between the two groups included type of ptosis (primary or recurrent), details of any previous ptosis surgery, preoperative MRD, levator function, and skin crease height, documented unusual intraoperative findings, type of ptosis repair (anterior-approach levator advancement or posterior-approach Muller's muscle resection), postoperative complications, and follow-up time.
Surgical success was defined as a postoperative MRD of ≥2 mm and ≤4.5 mm, inter-eyelid height asymmetry of ≤1 mm, and satisfactory eyelid contour.
During the study period, we began carrying out posterior-approach Muller's muscle resection. These cases were excluded from the final analysis, however, our indication (which has since changed) for this procedure at the time, was the absence of the VIS sign, minimal dermatochalasis and in which a satisfactory reversal of ptosis with instillation of 2.5% phenylephrine drops could be demonstrated. Institutional Review Board approval for this prospective audit was obtained.
Surgical technique
All cases were performed under local anaesthesia with subcutaneous infiltration using 2% lignocaine and 1 : 80 000 epinephrine. Selected patients also received intravenous sedation at the time of local anaesthetic infiltration at the beginning of the procedure, but were alert for the remainder of the operation.
Following skin crease incision, the entire superior tarsal width is exposed with dissection and inferior retraction of pretarsal orbicularis oculi muscle. The levator aponeurosis is identified through incision of the orbital septum and superior retraction of the preaponeurotic fat, with avoidance of fat excision. The dehisced or disinserted inferior aponeurotic edge is reattached to the anterior tarsal surface with one to two 6–0 Vicryl horizontal mattress sutures. The amount of aponeurotic advancement is adjusted until a satisfactory eyelid height and contour are achieved with the patient's eyes open in primary gaze and in the supine position. We generally aim for an overcorrection of 1–2 mm higher than the desired postoperative level. The skin crease is reformed in the usual manner with 6–0 Vicryl sutures.
Patients are routinely reviewed at 1–2 weeks and 3 months postoperatively,
Statistical analysis
All analyses were performed using the SAS Version 9.13 (SAS Institute Inc., Cary, NC, USA). Comparisons between preoperative and postoperative measurements from the VIS and non-VIS groups were statistically analysed using a mixed model of Analysis of Variance (SAS, PROCMIXED) to account for the correlation caused by observations within the same patient. The success rates were modified using a logistic regression in which a term to compare the VIS and non-VIS groups was included; the correlation between the observations of the same patient was accounted for by the William procedure.6
Results
In both groups, the majority of procedures were performed for primary involutional ptosis with 9% (2/22) and 14% (10/74) being recurrent cases in the VIS and non-VIS groups, respectively.
Performing surgeon
A smaller proportion of procedures in the non-VIS group, (11%, 8/74) than the VIS group (59%, 13/22), were performed by the main Consultant surgeon (RM), the remainder by oculoplastic fellows trained in the above surgical techniques, and often under supervision.
Additional upper eyelid/brow procedures performed
Blepharoplasty was simultaneously performed in 55% of VIS (12/22) and 77% of non-VIS (57/74) ptosis procedures. Additional bilateral endoscopic brow lift was carried out in one patient in the non-VIS group.
Preoperative findings
In order to avoid any selection bias, only patients with severe degree of ptosis were included in the two groups that patients with preoperative MRD'S of one or less.
A mixed model analysis of variance and a modified logistic regression analysis confirmed that the two groups were identical in severity of ptosis.
Intraoperative findings
In the VIS group, documented intraoperative findings included a thinned and significantly retracted levator aponeurosis that was difficult to isolate intra-operatively (12/22, 55%) and a thin tarsus prone to full-thickness suture passes during aponeurosis reattachment (8/22, 36.3%) (Figure 2).
In the non-VIS group, no patients were documented intra-operatively, as having significant retraction of the levator aponeurosis. However, 14% (10/74) eyelids were recorded as having a very attenuated levator. Only one patient (3%, 1/44) was noted to have a floppy tarsus that was difficult to suture.
Three primary procedures performed in the VIS group were noted intraoperatively to persistently overcorrect during aponeurosis-tarsal reattachment, with up to 2 mm of upper scleral show. However, when left in the overcorrected state, two of these procedures spontaneously settled to a satisfactory eyelid height by the end of surgery (Figure 3), whereas one patient treated with a hang-back suture to compensate for this persistent overcorrection subsequently had an under-corrected postoperative outcome.
The total incidence of intraoperative difficulties during surgery were 78% in the VIS group and 22% in the non-VIS group.
Outcomes
Mean post-operative follow-up was 22 (median 18, range 12–64) weeks.
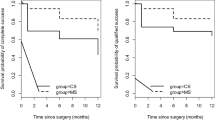
The overall success rates were 63.6% (14/22) in the VIS group, compared with 77.0% (57/74) in the non-VIS group (P=0.260).
In both groups, all failures were due to under correction, rather than asymmetry in height or unsatisfactory contour. The mean time to failure was 11.3±4.5 (range 2–16) weeks in the VIS group and 15.7±10.0 (range 2–29) weeks, in the non-VIS group (P=0.449).
There were no significant postoperative complications in either group.
Outcomes of caucasian patients undergoing ptosis surgery only
Asian or Afro-Caribbean patients and those who had undergone concurrent blepharoplasty and browlift surgery may have confounded final outcomes. We excluded these (seven VIS and 35 VIS) patients. The remaining five VIS (mean age 67 years, range 50–83, one male and four females) and nine non-VIS (mean age 72 years, range 54–82, five male and four female) patients underwent seven and 13 ptosis procedures, respectively. The majority of procedures (six VIS, eight non-VIS) were simultaneous bilateral ptosis repairs. The majority of procedures were primary with 28.6% (2/7) and 38.4% (5/13) being recurrent cases in the VIS and non-VIS groups, respectively. In the VIS group, iris colour was blue (3), hazel brown (1), and light brown (1) and in the non-VIS group, blue (3), light brown (4), and dark brown (2).
The total incidence of intraoperative difficulties during surgery were 85% in the VIS group and 15% in the non-VIS group. In the VIS group, documented intraoperative findings included a thinned and significantly retracted levator aponeurosis difficult to isolate (3/7), and thin tarsus prone to full-thickness suture passes during aponeurosis reattachment (1/7). Two primary procedures performed in the VIS group were noted intraoperatively to persistently overcorrect (see above). One spontaneously settled to a satisfactory eyelid height by the end of surgery and the other patient was treated with a hang-back suture and subsequently had an under-corrected postoperative outcome.
In the non-VIS group, no patients were documented intra-operatively, as having significant retraction of the levator aponeurosis. However, two of 13 eyelids were recorded as having a very attenuated levator.
Mean postoperative follow-up was 26 (median 23 weeks, range 12–61) weeks. The overall success rates were 57.1% (4/7) in the VIS group, compared with 69.2% (9/13) in the non-VIS group (P=0.598). All failures were due to under correction. The mean time to failure was 11±1.1 (range 9–13) weeks and 15.7±10.0 (range 2–29) weeks, in the VIS and non-VIS groups, respectively (P=0.449). There were no significant postoperative complications in either group.
Discussion
Our study describes a clinical sign, the VIS that most likely represents severe involutional aponeurotic ptosis. Patients are likely to have one or more features of a thinned and/or retracted levator aponeurosis, thin tarsus, and a tendency for persistent immediate overcorrection and retraction following levator advancement. We found this sign to be present in approximately 20% of eyelids evaluated prospectively. Given that only one of two values, 0 or 1 mm were recorded for MRD, there was effectively, very little difference between the two groups. However, after excluding cases undergoing concurrent blepharoplasty and so on, the overall success rates were lower using an anterior-approach (57.1% VIS versus 69.2% non-VIS) with failure due to under correction. We suggest that the VIS may be a useful objective clinical sign, which in contrast to existing linear (eg MRD or levator function) or subjective (eg brow compensation) observations can help define a sub-group of severe involutional ptosis. This in-turn may aid appropriate patient counselling and selection of procedure. Furthermore, it is possible that this sign may be useful in standardisation of a cohort when evaluating the results of involutional ptosis surgery, for example, for the purpose of audit or future studies.
The histopathological and clinical changes of involutional levator aponeurotic ptosis have been well described.2, 3, 4, 5, 7, 8 Ptosis results from localised or generalised disinsertion or dehiscence of the aponeurosis from the tarsal plate. The aponeurosis is usually attenuated, and in a subset of patients, there are also abnormalities of the levator muscle itself, with fatty degeneration3 or reduction of striated muscle fibres.9 Loss of the inferior attachments of the aponeurosis to the tarsus and orbicularis muscle results in upward movement of the visible skin crease, as well as superior retraction of the aponeurosis, orbital septum and preseptal orbicularis.1, 2, 3, 4, 5 The VIS most likely reflects the severe end of the spectrum of the changes described.
Surgical procedures to repair aponeurotic ptosis are well established, with the common aim of advancing and reattaching a dehisced or disinserted aponeurosis to the tarsus.10, 11, 12 The ability to adjust eyelid height intra-operatively during these procedures has contributed to more consistent and predictable postoperative results. Reported success rates for aponeurotic ptosis repair range from 70 to 95%, with varying objective and subjective criteria of success used.10, 11, 12, 13, 14
There have been few reports looking at factors that affect success rates following aponeurotic ptosis repair. As would be expected, patients with more severe ptosis and poorer levator function have been reported to be at increased risk of under-correction and a less favourable outcome.11, 14, 15 Patients with VIS most likely have greater thinning and retracted upper eyelid structures contributing to the visibility of the iris through eyelid tissue. We have found both light and dark irides to be readily visible in patients with VIS. In dark-skinned individuals, the iris colour may obviously be harder to define, however, iris colour in such individuals tends to be dark and the distinction between its circumferential outline and the adjacent white sclera tends to help determine its presence. We do not find quantification helpful, that is to say, attempting to grade the degree of iris colour visible and we consider VIS to be positive if merely the outline of the circular iris is visible. In such cases, at least 2–3 clock-hours of iris-sclera outline should be discernable.
In total, 60% of patients in the VIS group were noted to have an attenuated and retracted levator aponeurosis that was difficult to isolate at the time of surgery. This retraction of the aponeurosis deep into the orbit may increase the risk of unnecessary dissection, damage to levator aponeurosis and muscle, and unintentional inclusion of the septum during reattachment of the aponeurosis to the tarsus. Furthermore, reattachment of a long-standing retracted aponeurosis appeared to result in immediate and in some cases, persistent overcorrection and eyelid retraction at the time of surgery, as noted in three procedures in this series. In two of these three procedures, this overcorrection spontaneously rectified itself to a satisfactory height before the end of the procedure, whereas in one case, in which the eyelid was placed on a hang-back suture to compensate, an unsatisfactory under-correction persisted postoperatively. This phenomenon may simply reflect a more-pronounced epinephrine effect, as it is possible that subcutaneous local anaesthetic (with epinephrine) infiltration diffuses more effectively or with greater effect upon Mullers muscle, in VIS patients.
A third of VIS procedures were complicated by a thinned tarsus that was difficult to suture and prone to full-thickness suture passes. This is a well-observed finding that has not been previously commented upon in relation to the spectrum of aponeurotic ptosis. Although the traditional anterior approach to ptosis repair allows formal dissection and reattachment of the levator aponeurosis to the tarsus, we wonder whether the posterior approach may have some potential advantages in the VIS patient. A posterior-approach aponeurosis advancement involves reattachment of the levator aponeurosis to the tarsus with full-thickness suture passes through the superior tarsus and onto the skin, in which they are tied. This approach eliminates the need to worry about unwanted full-thickness or inadequate partial-thickness tarsal bites during anterior-approach ptosis repair, and therefore, may allow more predictable reattachment of the aponeurosis. In the last 2 years, having switched almost exclusively to carrying out posterior-approach repair for involutional ptosis, we have completed a subsequent prospective audit of VIS and non-VIS involutional ptosis using posterior approach only and these results are presented in part 2.
Despite the preoperative identification of VIS and anticipation of its problems during surgery, the overall success rates after excluding cases undergoing concurrent blepharoplasty and so on were still lower in the VIS group (57.1 versus 69.2%).
The earlier and higher failure rates in the VIS group may be a reflection of the severity of ptosis, with thinner and more attenuated tissue predisposed to earlier stretching, cheese-wiring of sutures, inadequate suture bites through a thinned tarsus, and eventually disinsertion of the levator aponeurosis from the tarsus. Whether or not this could be partially overcome with the use of more apo-tarsal sutures (ie more than the one to two sutures used in this study) is a matter of speculation, and would be difficult to study given all the other variables potentially affecting success in the VIS group.
Although difficult to objectively report, there is also perhaps less apparent dermatochalasis and more upper sulcus hollowing in VIS ptosis, implying significant thinning and retraction, as well as possibly greater secondary brow over-compensation. This may be reflected in the slightly fewer (but statistically insignificant) number of associated blepharoplasty procedures carried in this group, in which dermatochalasis was not judged to require treating.
We acknowledge the many limitations of this retrospective analysis of a prospective audit. Although the VIS is a non-linear sign, in comparison to levator function, it is not entirely objective and requires one of many features rather than quantification to be considered present. We relied upon two observers agreeing on the presence of a visible iris, however, still noted that iris colour was hard to define through skin and were not clear, the presence of a circumferential segment of darkness in relation to adjacent white sclera (the iris outline) is used to help define VIS positivity. These criteria are obviously open to interpretation; however, in our opinion, this sign is obvious in a proportion of patients.
Potential confounding factors, including the presence of multiple surgeons in the study, the variation in number of apo-tarsal sutures used between surgeons, the subjective intraoperative findings susceptible to observer bias and the performance of additional procedures at the time of ptosis repair. In particular, a significantly higher proportion of patients in the non-VIS group underwent concomitant blepharoplasty and/or brow lifts compared with the VIS group, which although unlikely, but theoretically could affect final eyelid height and higher success rates seen in the non-VIS group. A more rigorous prospective study, may allow a more definitive statement regarding the impact of VIS on the success rates of anterior-approach ptosis surgery. We suggest that VIS most likely represents a simple clinical sign of the severe spectrum of ptosis in which the outcomes of anterior-approach ptosis surgery may have a more unpredictability outcome.
In conclusion, patients with VIS are likely to have more severe involutional ptosis with features, including a thinned tarsus prone to full-thickness suture passes and a retracted aponeurosis that may be difficult to isolate and cause immediate persistent overcorrection during reattachment. Forewarned is forearmed, and we suggest that the preoperative identification of VIS may help in appropriate patient counselling, procedure selection, anticipation of intraoperative difficulties and possibly further standardisation of future cohorts when evaluating the results of involutional ptosis surgery.

References
Leatherbarrow B . Blepharoptosis. In: Martin Dunitz (ed). Oculoplastic Surgery. Taylor and Francis: London, 2002, pp 21–43.
Siddens DJ, Nesi FA . Aquired ptosis: classification and evaluation. In: Nesi F, Lisman R, Levine R (eds). Smith's Ophthalmic Plastic and reconstructive surgery. Mosby -Year Book Inc: St Louis, 1998, pp 380–381.
Martin P, Rogers P . Involutional ptosis: recognition and management. Aust NZ J Ophthalmol 1985; 13 (2): 185–187.
Collin J . Involutional ptosis. Aust NZ J Ophthalmol 1986; 14: 109–112.
Holstrom H, Fillip C . Aponeurotic repair of involutional blepharoptosis. Scand J Plast Reconstr Surg Hand Surg 2002; 36: 160–165.
Dortzbach R, Sutula F . Involutional blepharoptosis: a histopathological study. Arch Ophthalmol 1980; 98: 2045–2050.
Sutula F . Histopathological changes in congenital and aquired blepharoptosis. Eye 1988; 2: 179–184.
Kuwabara T, Cogan D, Johnson C . Structure of the muscles of the upper eyelid. Arch Ophthalmol 1976; 93: 1189–1197.
Jones L, Quickert M, Wobig J . The cure of ptosis by aponeurotic repair. Arch Ophthalmol 1975; 93: 629–634.
Anderson R, Dixon R . Aponeurotic ptosis surgery. Arch Ophthalmol 1979; 97: 1123–1128.
Older J . Levator aponeurosis surgery for the correction of aquired ptosis. Ophthalmology 1983; 90: 1056–1059.
Linberg J, Vasquez R, Chao G . Aponeurotic ptosis repair under local anaesthesia. Ophathlmology 1988; 95: 1046–1052.
Berlin A, Vestal K . Levator aponeurosis surgery: a retrospective review. Ophthalmology 1989; 96: 1033–1037.
Frueh B, Musch D, Mc Donald H . Efficacy and efficiency of a new involutional ptosis correction procedure compared to a traditional aponeurotic approach. Trans Am Ophthalmol Soc 2004; 102: 199–207.
McCulley T, Kersten R, Kulwin D, Feuer W . Outcome and influencing factors of external levator palpebrae superioris aponeurosis advancement for blepharoptosis. Ophthalmic Plast Reconst Surg 2003; 19: 388–393.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Malhotra, R., Salam, A., Then, SY. et al. Visible iris sign as a predictor of problems during and following anterior approach ptosis surgery. Eye 25, 185–191 (2011). https://doi.org/10.1038/eye.2010.177
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2010.177
Keywords
This article is cited by
-
Influence of fatty deposits in the levator aponeurosis/levator palpebrae superioris muscle on outcomes of aponeurotic repair in a Japanese population
Eye (2018)
-
Outcomes for severe aponeurotic ptosis using posterior approach white-line advancement ptosis surgery
Eye (2018)
-
Influence of upper and temporal transconjunctival sclerocorneal incision on marginal reflex distance after cataract surgery
BMC Ophthalmology (2016)
-
Open-sky isolated subtotal Muller’s muscle resection for ptosis surgery: a review of over 300 cases and assessment of long-term outcome
Eye (2013)