Abstract
Purpose
To evaluate the surgical outcome of combined trabeculotomy–trabeculectomy in Ghanaian children with primary congenital glaucoma.
Materials and methods
A retrospective case series involving 19 eyes of 12 consecutive children with primary congenital glaucoma who had primary trabeculotomy–trabeculectomy from 12 August 2004 to 30 June 2008, at the Korle-Bu Teaching Hospital, Ghana. Main outcome measures were preoperative and postoperative intraocular pressures, corneal diameter, corneal clarity, bleb characteristics, duration of follow-up, surgical success, and complications.
Results
A total of 19 eyes of 12 patients met the inclusion criteria. Six of the patients were males. Mean age at diagnosis was 4.4 (range 2–8) months. Mean age at surgery was 5.9 months (range 3–16). Eight (67%) infants had bilateral disease. Mean duration of follow-up was 13.1 (range 5–38) months. The preoperative mean horizontal corneal diameter was 13.4±1.1(range 12–16) mm. Complete success (intraocular pressure <21 mm Hg) was obtained in 15 (79%) eyes. The probability of success was 94.4, 83.3, 66.7, 44.4, 38.9, 33.3, and 13.3% at 3, 6, 9, 12, 15, 18, and 21 months, respectively (Kaplan–Meier analysis). All eyes had corneal oedema preoperatively. Seventeen eyes (90%) had clear cornea at their last follow-up. Mean preoperative and postoperative intraocular pressures were 30.3±8.8 and 18.1±6.8 mm Hg respectively (P<0.001, t-test). Twelve (63%) eyes had well-functioning blebs at the last follow-up. One eye (5%) developed seclusio pupillae and cataract postoperatively.
Conclusion
The overall success for combined trabeculotomy–trabeculectomy in Ghanaian children with primary congenital glaucoma was 79%. The probability of success reduced from more than 66% in the first 9 months postoperatively to below 45% after that.
Similar content being viewed by others
Introduction
Primary congenital glaucoma (PCG) is a hereditary childhood glaucoma resulting from abnormal development of the filtration angle, which occurs unassociated with other ocular or systemic abnormalities.1, 2
Surgical interventions are the main treatment for PCG3 and are designed to eliminate the resistance to aqueous outflow created by structural abnormalities in the anterior chamber angle.4, 5 Goniotomy and trabeculotomy have traditionally been regarded as procedures of choice for PCG because of high reported success rates. Goniotomy has the advantage of preserving the conjunctiva for future use, but requires a clear cornea and may have to be repeated more than once.6 Trabeculotomy is technically easier and produces a more predictable result than goniotomy.9, 10 Trabeculotomy has the added advantage of being possible in eyes in which visualization is not possible, but has the disadvantage of damaging the conjunctiva. In developing countries, majority of the children with congenital glaucoma present with severe disease and cloudy cornea precluding goniotomy.7, 8, 12 Recent reports have found combined trabeculotomy–trabeculectomy (CTT) to yield superior results in comparison with conventional procedures.9, 10, 11, 12, 13, 14, 15, 16
In Ghana, majority of children with PCG present with severe disease and cloudy cornea. Conventional trabeculectomy has been the surgical method commonly used for PCG treatment, but anecdotal data show poor outcomes. A modified trabeculectomy has been tried in the past on some children in the same population showing initial success rate more than 90% at 1 year follow-up (FUP),17 but poor FUP and the small numbers studied rendered this procedure of little hope and inconclusive for better outcome. A primary surgical procedure that yields higher long-term success rate will therefore be of great benefit to these children. To the best of our knowledge, there are no published reports on the success of CTT from the West African subregion to review.
The purpose of this study was to determine the surgical outcome of CTT for PCG in Ghanaian children.
Materials and methods
The medical records of all children who had CTT as a primary procedure from 12 August 2004 to 30 June 2008 were retrieved. As an institutional practice, all clinical and surgical notes of all children are routinely recorded on pre-designed forms at the time of diagnosis, during FUP evaluation and surgery for every child. All surgeries were performed by a single surgeon. A total of 32 glaucoma surgeries were performed and 24 of these were CTT. Patients with <3 months FUP were excluded from the study.
Data were compiled using pre-designed forms on: age at onset of symptoms (months), age at presentation (months), age at which surgery was performed (months), gender, preoperative visual acuity, postoperative visual acuity at the last visit, horizontal corneal diameter (mm), corneal clarity at presentation, corneal clarity at the last FUP, preoperative intraocular pressure (IOP; mm Hg), IOP at the last FUP (mm Hg), preoperative optic disc vertical cup/disc ratio (VC/D), postoperative VC/D at the last FUP, preoperative medications used, postoperative medications used, complications, refractive errors, and duration of FUP.
Examinations
Initial examination of all children was performed in the office setting to make a provisional diagnosis of congenital glaucoma. Diagnosis was confirmed under general anaesthesia using 1–1.5% halothane. The Child's condition was explained to parents and consent was obtained for the examination under general anaesthesia (EUA) and for the surgery that was performed at the same setting for the EUA. Both eyes were examined under anaesthesia but surgery was performed in one eye. In bilateral cases surgery was performed in the fellow eye after 1 or 2 week(s).
The IOP was measured at the initial phase of halothane inhalation 1–1.5% when the patients were just sedated, using Goldmann applanation method (Perkins tonometer by Clement Clarke International, Harlow, UK) in some patients, and in a few patients by indentation method using Shiötz tonometer when the former was not available.
The cornea was assessed under high magnification using handheld slit lamp (Zeiss HSO 10 Hand slit lamp and ophthalmoscope illuminator H, Carl Zeiss Meditec AG, Jena, Germany) in the office setting or with a torchlight and a 20 D lens in theatre before induction of anaesthesia. Corneal clarity was assessed based on the following criteria:
-
Grade 1: iris texture and pupil seen clearly
-
Grade 2: iris texture and pupil seen hazily
-
Grade 3: iris and pupil seen, texture not visible clearly
-
Grade 4: iris and pupil seen very hazily
-
Grade 5: iris and pupil not seen.
Horizontal corneal diameter (white to white) was measured using callipers. Assessment of the rest of the eyes including anterior segment and fundoscopy was carried out when cornea was clear enough to allow this.
Visual acuity could not be checked in most of the children preoperatively because of photophobia and some aged less than 3 months. Postoperative visual acuity was checked where possible using fixation methods or Cardiff cards.
Surgical procedure
Surgery was performed by one surgeon (EVA). Under general anaesthesia and aseptic technique, superior rectus bridal suture or corneal stay suture was placed using 4–0 or 6–0 silk. A limbus- or fornix-based conjunctival flap was raised and haemostasis was secured with cautery. A 4 × 4 mm partial thickness scleral flap was dissected into about 1 mm of clear cornea. A 2 × 2 mm inner trabeculectomy groove was carried out. A radial incision was then carried out across the inner trabeculectomy site about 2 mm from the limbus or the junction between white and bluish transitional zone of the sclera (this marks externally the site of the Schlemm's canal), until the Schlemm's canal was entered; evidenced by a gush of aqueous humour and/or blood. Trabeculotomy ab externo was then performed using the internal arm of Harm's trabeculotome probes, first to the left then to the right to complete about 100–120° of the circumference. The pre-marked 2 × 2 mm inner block tissue comprising trabecular meshwork and scleral spur was excised with Vannas scissors and peripheral iridectomy was performed with a base of at least 2 mm. The partial thickness scleral flap was sutured using three interrupted sutures (at apex and the two sides) with 10–0 nylon. The conjunctival flap was closed with 8–0 or 6–0 vicryl (polyglactin) continuous stitches. At the end of the surgery, the patency of the peripheral iridectomy and scleral flap and how watertight the conjuctival flap were assessed. Dexamethasone (1 mg) and gentamicin (20 mg) were injected subconjunctivally. Topical cyclopentolate 1% and ciprofloxacin 0.3% eye drops were instilled and an eye patch and eye shield applied.
Postoperative management
Children were examined at postoperative day 1, 1 week, 2 weeks, 1 month, and then 3 monthly in the first year, 6 monthly in the second year, and yearly thereafter. Postoperative treatment included gtt. cyclopentolate 1% b.i.d. for 1 month and prednisolone acetate forte 1% q.i.d. for 6 weeks, and gtt. ciprofloxacin 0.3% q.i.d. for at least 1 week.
At each postoperative visit the patients were examined and the following parameters were noted: visual acuity, corneal clarity, bleb characteristics, IOP (in the office where possible using Perkins tonometer or Keeler Pulsair non-contact tonometer (part number 2414-P-6000, Keeler Ltd, Windsor, UK), the latter in two eyes, else under general anaesthesia as described earlier). The optic nerve assessment by indirect ophthalmoscopy and cycloplegic refraction was carried out periodically and especially at EUA.
Outcome measures
Outcome measures studied were preoperative and postoperative IOP, horizontal corneal diameter, corneal clarity, bleb characteristics, surgical success, and complications. Surgical success was defined by the following criteria IOP⩽21 mm Hg, stable corneal diameter and clear cornea, at least 3 months FUP.
Statistical analysis
Data were captured using Microsoft Office Excel and analysed using Epi Info version 3.4.3 software (Centers for Disease Control and Prevention, Atlanta, GA, USA). Continuous numerical data were captured as mean and standard deviation (SD) and categorical data as percentages (%). The difference of means was determined using paired t-test. A P<0.05 was considered statistically significant. Cumulative success probability was determined using Kaplan–Meier survival analysis.
Results
A total of 19 eyes of 12 patients met the inclusion criteria. There were 6 male and 6 female patients. The mean age at diagnosis was 4.4 months (range, 2–8; median, 4.0 months). The mean age at surgery was 5.9 months (range, 3–16 months; median, 4.0 months). Eight (67%) of the infants had bilateral disease.
Intraocular pressure
The mean preoperative IOP was 30.3 mm Hg (range, 15–42.1; median, 31.6 mm Hg). Three eyes had normal IOP preoperatively; one eye was on anti-glaucoma medication and the medication was stopped on the day of surgery; the other two eyes had the IOP determined in the deep phase of halothane anaesthesia. They however had features consistent with congenital glaucoma.
The mean postoperative IOP (at last FUP) was 18.1 mm Hg (range, 10–42; median, 17.3 mm Hg). The IOP in the two eyes checked with Pulsair non-contact tonometer without anaesthesia and in the office setting was normal. There was a statistically significant difference in the preoperative and last FUP IOPs (P<0.001, paired t-test).
Corneal clarity and diameters
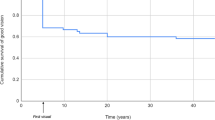
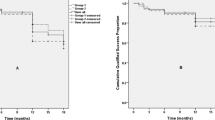
All the eyes had some degree of corneal oedema preoperatively, with subsequent improvement resulting in clear cornea in majority of the eyes postoperatively Figure 1. The mean horizontal corneal diameter was 13.4±1.1 mm ranging between 12 and 16.
Bleb characteristics
An ideal, clinically well-functioning bleb is one that is elevated (low to moderately) and diffuse, without any restricting scar, and relatively avascular. This was present in 12 (63%) of 19 eyes, which included 2 eyes that had fornix-based conjunctival flaps. In the remainder of the eyes (n=7), the blebs were flat, scarred, and appeared to be clinically non-functional. The bleb characteristics for analysis were those recorded at the patients’ last FUP visits. A comparison in bleb morphology between the eyes that had fornix-based conjunctival flaps (2, 10% eyes) and those with limbal-based conjunctival flaps (17, 90% eyes) could not be carried out statistically on account of the small numbers of the fornix-based flaps.
Optic disc cupping
The optic disc cupping could not be assessed preoperatively in any of the eyes. Postoperatively, the assessment was carried out in nine eyes at the last FUP. The range of the vertical cup/disc ratio was 0.5–0.8, mean 0.7 (±0.12).
Surgical success rate and follow-up
The mean duration of FUP was 13.1 months (range, 5–38 months; median, 10.0 months). Complete success as defined in this study (IOP<21 mm Hg) was obtained in 15 eyes (79%) whereas 4 eyes (21%) were considered to be failures at the last FUP. Kaplan–Meier survival analysis revealed the probability of success of more than 66% in the first 9 months postoperatively reducing significantly below 44% from 12 months and beyond (Figure 2; Table 1). A similar result was obtained when the number of persons was considered, with those with bilateral condition one eye was randomly selected for the analysis. Figure 3a and b shows the preoperative and 24 month postoperative photographs, respectively, of a patient with a successful outcome.
Surgical complications
Out of 19, 1 (5%) eye developed hyphaema that cleared postoperatively and out of 19, 3 (16%) eyes had subconjuctival haemorrhage. There was a false passage of the trabeculotome probe intraoperatively resulting in detached iris root in one eye (5%). One eye (5%) had sight threatening postoperative complication of seclusion pupillae and cataract.
Postoperative visual acuity and refractive status
Data on postoperative visual acuity and refraction at the last FUP were inadequate for us to make any meaningful statistical analysis.
Discussion
Our study showed that CTT achieves good success in our patients with PCG in the first 9 months postoperatively. The overall surgical success rate of CTT in our study was 79%. This corroborates findings from other studies in India and the Middle East, where this procedure is commonly used, with reported surgical success rates for CTT ranging between 75 and 94%.8, 11, 13, 15, 16 Many of these studies however involved larger numbers, long FUP periods, and differences in definition of surgical success, which may explain the wide range of success. In addition, some studies also involved the use of adjunctive anti-metabolites, which could explain higher success rate than ours.16
Survival analysis for success for CTT has demonstrated probability for success more than 70% after 1 year in Asian and Middle Eastern series,11, 12, 15, 16 even up to the sixth year in Indian children.18
Our study however showed initial high success in the first 9 months postoperatively, reducing below 45% after this period. This difference in success may be due to racial or genetic differences among other factors, and needs further studies.
Conventionally, goniotomy and trabeculotomy have been regarded as procedures of choice for PCG.2 Trabeculectomy, a glaucoma filtering surgery, is the standard surgical method of treatment for adults with glaucoma especially in West Africa, and most ophthalmologists are conversant with the surgical technique. It is often unsuccessful in children and young adults.19, 20
Some studies, however, have claimed satisfactory results.2, 3, 4, 5, 6, 17, 21 Some of these studies from the West African sub-region have been associated with short duration of FUP and small numbers17, 21 making prediction of long-term success difficult. A retrospective case series involving 36 children (65 eyes) in which a modified trabeculectomy was tried in the same population for our study, with FUP periods ranging from 3 months to 10 years (mean and median not stated), showed a success of up to 92% in the first year. However, the numbers at subsequent FUPs progressively decreased from 25 eyes at 2 years to 6 eyes at 10 years with varying definition of success for some of the years and conflicting numbers of eyes followed up.17 The poor FUP and the small numbers studied rendered this procedure inconclusive for better long-term outcome and as a procedure of choice. Second, it is a known fact that the use of trabeculectomy without anti-metabolites in adults with glaucoma of African descent is associated with poor outcome,22, 23 a fact that is also demonstrated in adult Ghanaians,23, 24 suggesting a possibility of failure in children of same racial descent. These facts, coupled with the poor result of trabeculectomy in children because of the aggressive wound-healing response, presence of a thick Tenon's capsule and low scleral rigidity,25 the mild to serious ocular complications that tend to be associated with adjunctive anti-fibrotic drug use, even though the latter on the average improves trabeculectomy outcome,25, 26, 27, 28, 29 all informed our quest to try the CTT alone as an alternate procedure.
Combining trabeculotomy ab externo with trabeculectomy offers many theoretical and practical advantages, with superior results over the other conventional techniques in controlling the IOP. CTT provides dual outflow pathways: trabeculotomy removes the possible obstruction to aqueous outflow, creating a direct continuity between the anterior chamber and Schlemm's canal and trabeculectomy by-passes the episcleral venous system. It also allows greater surgical flexibility in advanced buphthalmos for conversion to trabeculectomy in cases where identification of Schlemm's canal is not possible.11, 13 Studies from India and the Middle East corroborate the fact that CTT is superior to trabeculectomy in the treatment of PCG.11, 13, 16, 30
There was significant reduction of IOP from mean preoperative level of 30.3–18.1 mm Hg postoperatively. This is hoped to influence outcome as elevated IOP resulting from maldevelopment of angle structures is considered a significant factor in the pathogenesis of optic nerve and other ocular damage in PCG.2 Yalvac et al31 however did not find IOP and other factors such as corneal diameter, gender, and consanguinity to influence outcome. Other factors that influence prognosis of PCG include severity of disease,16, 32 time of presentation, and time of surgery. The earlier in life the disease occurs the worse the prognosis, and the more severe the disease the higher the failure rate.32 Our patients presented with advanced disease evidenced by large corneal diameters and cloudy corneae. The average corneal diameter at presentation was 13.4 mm with significant number presenting with corneal diameters between 14 and 16 mm. These corneae are undoubtedly too large for infants with an average age at presentation of about 4.4 months. Out of 18, 14 (78%) eyes had significant corneal oedema that precluded the details of structures beyond the cornea from detailed visualization. These may account, in part, for the decrease in success after 9 months postoperatively. Some factors shown to be associated with successful surgery are smaller corneal diameter,33, 34, 35 and shorter axial lengths (<24 mm).31, 36 We did not measure axial lengths in our study, therefore we are unable to relate this to our results.
All eyes operated on in our study had corneal oedema at presentation and 90% had clear cornea postoperatively. Mandal12 reported that 84.7% of the patients with developmental glaucoma operated on within the first 6 months of life had significant corneal oedema preoperatively, but subsequently 62.4% had clear cornea postoperatively. Other studies by Mandal and colleagues, and others from the Middle East have also noted that majority of patients with PCG had significant corneal oedema at presentation.9, 12, 30
Of 15, 4 (27%) eyes that achieved surgical success had flat and scarred blebs. This success probably may be due to the dual outflow pathway provided by CTT as emphasized by Elder,11 and Mandal et al.13
Most of the complications encountered in our patients were minor. However, one eye developed seclusio pupillae and cataract postoperatively. Mandal and colleagues12, 13, 14, 15, 18, 30 have reported only minor postoperative complications in their previous studies. Al-Hazmi et al16 have reported more complications including exudative retinal detachment. Their high complication rates were probably due to the use of mitomycin C.
The paucity of data on CTT alone or CTT compared with conventional procedure from the African continent especially sub-Saharan Africa makes it impossible for any meaningful comparison.
This study would have had an added advantage by comparing the results with a control group of trabeculectomy alone, but this was not possible because records on trabeculectomy procedure alone were largely unavailable and recordings were non-standardized. This is because the procedure was carried out by different doctors before the establishment of the paediatric ophthalmology unit in the year 2004. In addition, one of the objectives of the study was to establish a baseline data with the use of CTT alone, which could help with further prospective study in future hence the present study design.
We acknowledge other limitations of our study: the retrospective nature, small number of patients studied, and the limited documentation of: optic disc assessment, refraction results and visual acuity findings.
In conclusion, the overall success rate for CTT in Ghanaian children with PCG was 79%. The probability of success reduces from over 66% in the first 9 months postoperatively to below 45% after 1 year.

References
Ho CL, Walton DS . Primary congenital glaucoma: 2004. J Pediatr Ophthalmol Strabismus 2004; 41: 271–288.
Papadopoulos M, Khaw PT . Childhood glaucoma. In: Taylor D, Hoyt CS (eds). Pediatric Ophthalmology Strabismus. Elsevier Saunders: Philadelphia, 2005, pp 458–471.
Papadopoulos M, Khaw PT . Advances in the management of paediatric glaucoma. Eye 2007; 21 (10): 1319–1325.
Allingham RR . Medical and surgical treatment of childhood glaucoma. In: Shields's Textbook of Glaucoma, 5th edn. Lippincott Williams and Wilkins: Philadelphia, 2005, p 626.
deLuise VP, Anderson DR . Primary infantile glaucoma (congenital glaucoma). Surv Ophthalmol 1983; 28: 1–19.
Russell-Eggitt IM, Rice NS, Jay B, Wyse RK . Relapse following goniotomy for congenital glaucoma due to trabecular dysgenesis. Eye 1992; 6: 197–200.
Agarwal HC, Sood NN, Kalra BR . Clinical presentation of congenital glaucoma. Indian J Ophthalmol 1983; 31: 619–622.
Mullaney PB, Selleck C, Al-Award A, Al-Mesfer S, Zwaan J . Combined trabeculotomy and trabeculectomy as initial procedure in uncomplicated congenital glaucoma. Arch Ophthalmol 1999; 117: 457–460.
Luntz MH . The advantages of trabeculotomy over goniotomy. J Pediatr Ophthalmol Strabismus 1984; 21: 150–153.
McPherson Jr SD, Berry DP . Goniotomy vs external trabeculotomy for developmental glaucoma. Am J Ophthalmol 1983; 95: 427–431.
Elder MJ . Combined trabeculotomy–trabeculectomy compared with primary trabeculectomy for congenital glaucoma. Br J Ophthalmol 1994; 78: 745–748.
Mandal AK . Long-term surgical and visual outcomes in Indian children with developmental glaucoma operated on within 6 months of birth. Ophthalmology 2004; 111: 283–290.
Mandal AK, Naduvilath TJ, Jayagandhan A . Surgical results of combined trabeculotomy–trabeculectomy for developmental glaucoma. Ophthalmology 1998; 105: 974–982.
Mandal AK, Bhatia PG, Gothwal VK, Reddy VM, Sriramulu P, Prasad MS et al. Safety and efficacy of simultaneous bilateral primary combined trabeculotomy–trabeculectomy for developmental glaucoma in India. Indian J Ophthalmol 2002; 50: 13–19.
Mandal AK, Gothwal V, Bagga H, Nutheti R, Mansoori T . Outcome of surgery on infants younger than 1 month with congenital glaucoma. Ophthalmology 2003; 110: 1909–1915.
Al-Hazmi A, Awad A, Zwaan J, Al-Mesfer A S, Al-Jadaan I, Al-Mohammed A . Correlation between surgical success rate and severity of congenital glaucoma. Br J Ophthalmol 2005; 89: 449–453.
Adu-Darko M . Primary congenital glaucoma treated by modified trabeculectomy. GMJ 2002; 36: 72–75.
Mandal AK, Gothwal VK, Nutheti R . Surgical outcome of primary developmental glaucoma: a single surgeon's long-term experience from a tertiary eye care centre in India. Eye 2007; 21: 764–774.
Beauchamp GR, Parks MM . Filtering surgery in children: barriers to success. Ophthalmology 1979; 86: 170–180.
Gressel MG, Heuer DK, Parrish RK . Trabeculectomy in young patients. Ophthalmology 1984; 91: 1242–1246.
Onwesigue EN, Ezegui IR, Onwasigue CN, Aghaji AE . Management of primary congenital glaucoma by trabeculectomy in Nigeria. Annals Trop Paediatr 2008; 28: 49–52.
Broadway D, Murdoch I . Glaucoma in blacks. In: El Sayyad F (ed) The Refractory Glaucomas. Igaku-Shoin Medical Publishers: New York, 1995; pp31–54 (Chapter 2).
Egbert PR . Glaucoma in West Africa: a neglected problem. Br J Ophthalmol 2002; 86: 131–132.
Hanna YK, Egbert PR, Singh K . Long-term comparison of primary trabeculectomy with 5-fluorouracil versus mitomycin C in West Africa. J Glaucoma 2008; 17: 578–583.
Abraham LM, Selva D, Casson R, Leibovitch I . Mitomycin: clinical applications in ophthalmic practice. Drugs 2006; 66 (3): 321–340.
Smith S, D’Amore PA, Dreyer FB . Comparative toxicity of mitomycin C and 5-fluorouracil in vitro. Am J Ophthalmol 1994; 118 (3): 332–337.
Greenfield DS, Leibmann JM, Jee J, Ritch R . Late onset bleb after glaucoma filtering surgery. Arch Ophthalmol 1998; 116: 443–447.
Ticho U, Ophir A . Late complications after glaucoma filtering surgery with adjunctive 5-fluorouracil. Am J Ophthalmol 1993; 115: 506–510.
Abraham LM, Selva D, Casson R, Leibovitch I . The clinical applications of fluorouracil in ophthalmic practice. Drugs 2007; 67 (2): 237–255.
Mandal AK, Matalia JH, Nutheti R, Krishnaiah S . Combined trabeculotomy and trabeculectomy in advanced primary developmental glaucoma with corneal diameter of 14 mm or more. Eye 2006; 20: 135–143.
Yalvac IS, Satana B, Suveren A, Eksioglu U, Duman S . Success of trabeculotomy in patients with congenital glaucoma operated on within 3 months of birth. Eye 2007; 21: 459–464.
Dureau P, Dollfus H, Cassegrain C, Dufier JL . Long-term results of trabeculectomy for congenital glaucoma. J Pediatr Ophthalmol Strabismus 1998; 35: 198–202.
Anderson DR . Trabeculotomy compared to goniotomy for glaucoma in children. Ophthalmology 1983; 90: 805–806.
Song J, Stinnett SS, Whitson JT, Kooner KS . Ten-year surgical experience with childhood glaucoma. J Pediatr Ophthalmol Strabismus 2003; 40: 11–18.
Quigley HA . Childhood glaucoma: results with trabeculotomy and study of reversible cupping. Ophthalmology 1982; 89: 219–226.
Dietlein TS, Jacobi PC, Krieglstein GK . Prognosis of primary ab externo surgery for primary congenital glaucoma. Br J Ophthalmol 1999; 83: 317–322.
Acknowledgements
We thank Dorothy Fiadoyor and Ben Abaidoo who helped in diverse ways with the data compilation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Presented as e-poster at the 1st World Congress of Paediatric Ophthalmology and Strabismus in Barcelona, Spain, September 2009.
Rights and permissions
About this article
Cite this article
Essuman, V., Braimah, I., Ndanu, T. et al. Combined trabeculotomy and trabeculectomy: outcome for primary congenital glaucoma in a West African population. Eye 25, 77–83 (2011). https://doi.org/10.1038/eye.2010.156
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2010.156
Keywords
This article is cited by
-
Profile of primary childhood glaucoma at a child eye health tertiary facility in Malawi
BMC Ophthalmology (2022)
-
Combined trabeculotomy–trabeculectomy with and without augmentation in primary congenital glaucoma: triple-armed randomized controlled trial
International Ophthalmology (2022)
-
Ab externo 240-degree trabeculotomy versus trabeculotomy–trabeculectomy in primary congenital glaucoma
International Ophthalmology (2020)
-
Long-term outcome of combined trabeculotomy–trabeculectomy by a single surgeon in patients with primary congenital glaucoma
Eye (2018)
-
Combined trabeculotomy-trabeculectomy using the modified Safer Surgery System augmented with MMC: its long-term outcomes of glaucoma treatment in Asian children
Graefe's Archive for Clinical and Experimental Ophthalmology (2018)