Abstract
Purpose
To report the long-term sequential morphological and functional results in eyes with metamorphopsia after retinal detachment (RD) repair.
Patients and methods
In six eyes of six patients aged 58.7±11.0 years with metamorphopsia after successful buckling surgery for macula-off RD, best-corrected visual acuity (BCVA), fundus biomicroscopy, Amsler grid test, time-domain optical coherence tomography (TD-OCT) and central 12° microperimetry (MP-1) were performed at months 1, 3, 6, 12, and 18. At 5 to 6 years after surgery all patients underwent also spectral domain (SD)-OCT.
Results
Three eyes slowly recovered pre-RD BCVA. In the remaining three eyes—with good final BCVA—the interrupted junction line between photoreceptor cell inner and outer segments (IS/OS) was progressively less evident after RD surgery; and the external limiting membrane was preserved on SD-OCT examination. In all eyes post-operative metamorphopsia faded with time, but fully disappeared in 6 years only in two eyes without photoreceptor abnormalities. One of the two eyes with subretinal fluid up to 6 months and IS/OS disruption had central dense scotoma with relatively unstable fixation on MP-1 and persistent metamorphopsia. Macular sensitivity (MS) increased from 9.7±7.1 at month 1 to 13.5±5.6 dB at the final check, and was weakly (r=0.33) correlated with post-operative BCVA and OCT abnormalities.
Conclusion
Long-standing metamorphopsia can occur after successful macula-off RD repair even without detectable photoreceptor disruption on OCT. Post-operative BCVA recovery weakly correlates with increasing MS, and late restoration of the photoreceptor layer may be observed
Similar content being viewed by others
Introduction
Scleral-buckling procedure is the most commonly used surgical treatment of rhegmatogenous retinal detachment (RD), with or without intravitreal gas injection. This technique is still preferred by many surgeons, whereas others prefer to treat uncomplicated cases with primary pars plana vitrectomy, especially in pseudophakic or aphakic eyes.1 After scleral-buckling procedure, visual recovery is related to the pre-operative and post-operative macular condition. A poor functional outcome is common because of post-operative complications, such as persistent subfoveal fluid, even in a pre-operatively uninvolved macula,2 epiretinal membranes, and cystoid macular oedema.3, 4
Three important predictors of visual recovery are pre-operative visual acuity, shorter duration of RD, and younger age.5 However, some patients with an apparently normal macula after an uncomplicated and timely scleral-buckling procedure may experience incomplete visual recovery and persistent metamorphopsia.6
The aim of this paper was to perform a prospective study of the anatomical and functional findings of a series of eyes which underwent successful RD surgery, but showed post-operative metamorphopsia and slow visual acuity recovery.
Materials and methods
Inclusion criteria were: (1) patients with post-operative Snellen best-corrected visual acuity (BCVA) not exceeding 0.5 and complaining of metamorphopsia 1 month after successful unilateral macula-off RD repair; (2) surgical procedure performed by the same surgeon within 7 days from RD onset; (3) BCVA before RD onset exceeding 0.7, regardless of the refractive error.
Exclusion criteria were: (1) patients with history of uveitis, glaucoma or trauma, (2) patients with previous intraocular surgery and post-operative epiretinal membranes or cystoid macular oedema.
Six phakic eyes of six (four men and two women) patients (mean age 58.7±11.0, range 44–70 years), who met the inclusion/exclusion criteria and underwent one conventional scleral buckling procedure in 2003–2004, were enroled.
In all eyes after a 360° limbal peritomy and retinal break localization, a circumferential scleral buckling was sutured to the sclera and subretinal fluid (SRF) was completely removed before the injection of gas mixture (20% SF6 and 80% air). One or more silicone implants were placed under scleral buckling. The retina was completely flattened at the end of surgery and there were no intra-operative or post-operative complications.
At 1, 3, 6, 12, and 18 months after surgery, all patients underwent slit-lamp biomicroscopy, indirect ophthalmoscopy, BCVA evaluation, Goldmann applanation tonometry, Amsler grid (AG) test, optical coherence tomography (Stratus OCT-3 Carl Zeiss, Jena, Germany), and microperimetry (MP-1 Microperimeter, Nidek Technologies, Gamagori, Japan). At 5 to 6 years post-operatively, we reviewed the patients’ charts, and performed the same thorough evaluation, including spectral domain (SD) 3D OCT-1000 (Topcon Medical Systems, Paramus, NJ, USA) examination and Pelli–Robson contrast sensitivity chart test. Time domain (TD) and SD-OCT were performed in the same day in each patient. Horizontal and vertical scans centred in the fovea were acquired both with TD-OCT and SD-OCT by two experienced scientific staff members. Radial scans of 6 mm in size were compared between TD-OCT and the 50 times faster SD-OCT. Axial resolution was ∼10 and 5 μm for TD-OCT and SD-OCT, respectively.
MP-1 examination features in a darkened room were: electronic eye tracking system, 12° in diameter grid with 45 points, starting attenuation set at 10 dB, Goldmann III stimulus size, and fixation target ring 1° in diameter. Fixation was regarded as stable if more than 75% of fixation points were inside the 2° diameter circle; relatively unstable if less than 75% fixation points were inside 2° diameter, but more than 75% were inside 4°diameter circle; and unstable if less than 75% of fixation points were inside the 4° diameter circle. A correlation between mean macular sensitivity (MS) as produced by the MP-1 software 1.7 and BCVA was performed by pooling together all data from six different checks of six patients.
For statistical tests, SPSS version 13.0 (Chicago, IL, USA) and Microsoft office Excel 2003 (Redmond, WA, USA) were used. Measurements were analysed using paired t-test and Pearson's correlation coefficient. P-values of <0.05 were considered to be of statistical significance.
Results
Spheroequivalent refraction before RD onset ranged from +2 to −12 D (mean −3.67±5.0 D, with four out of six eyes within +2 and −1 D (Table 1). Post-operative BCVA slowly improved (Figure 1) and peaked at 12 months in three eyes, at 18 months in two eyes, and after 6 years in one eye (Table 1). Patients 3 and 5 had the slowest visual recovery and reached 0.6 and 0.7 BCVA only at 12- and 18-month checks, respectively. Mean final BCVA (0.75±0.15) in our patients was slightly lower compared with pre-RD BCVA (0.87±0.10). Three (50%) eyes (patients 1, 2, and 6) recovered the pre-RD BCVA. At the last follow-up in the other three eyes, BCVA ranged from 0.6 to 0.7 (Table 1) and all eyes had normal contrast sensitivity (log 1.20–1.35), clear media, and normal intraocular pressure.
All patients complained of unsatisfactory quality of vision because of metamorphopsia, which faded with time but persisted in four out of six eyes at 5 to 6 years after RD surgery. The AG test showed distorted lines in 100% of patients, and no central scotoma, but in patient 3 up to the 6-month check. Patient 1 complained both of distorted grid through a yellowish halo and slightly moving letters at the visual acuity testing.
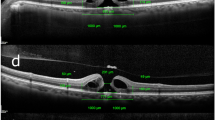
Post-operatively in three eyes (patients 3, 4, and 5), TD-OCT evidenced an interrupted junction line between photoreceptor cell inner and outer segments (IS/OS) (Table 2). The mild disruption of the IS/OS junction line evidenced by TD-OCT at both 12 and 18 months after RD surgery in patients 3 and 4 was apparently undetectable at the last check, when all patients underwent both TD- and SD-OCT examination. Also in patient 5 (Figure 2), the disruption of IS/OS junction line on TD-OCT was less evident over time and it was no longer detectable on SD-OCT 70 months post-operatively. In all eyes, IS/OS junction was better detectable on high resolution SD-OCT than on TD-OCT and preservation of the back-reflection line from the external limiting membrane (ELM) could be detected on SD-OCT examination.
Patient 5. Microperimetry (MP-1) (left column) and time (TD) and spectral domain (SD) optical coherence tomography (OCT) (right column) after RD surgery. MP-1 shows central fixation and increased foveal sensitivity after 12 months (b) as compared with the 6-month check (a). Mean macular sensitivity was normal and remained stable at all examinations (a, c, and e). The disruption of photoreceptor IS/OS junction (arrow) on TD-OCT is more evident at (b) 6- than at (d) 12-month examination. At 70 months after RD repair, apparently normal IS/OS junction (arrow) and preserved ELM (arrowhead) are better detected on SD-OCT (g) than TD-OCT (f).
Residual SRF found in two eyes (patients 3 and 6) was no longer detectable on TD-OCT at the 12-month check, and some photoreceptor IS/OS disruption was evident in patient 3 only (Table 2). OCT never revealed abnormal findings in two eyes (patients 1 and 2) during the entire follow-up.
Mean MS in the central 12° (MP-1) increased in all the eyes during the follow-up from 9.7±7.1 at month 1 to 16.7±5.0 dB at month 18, but decreased at the final check (13.5±5.7 dB) approaching the mean 6-month level (15.3±4.7 dB) (P=0.25, ns) (Figure 3). Regression analysis of the entire follow-up data showed that mean MS was weakly correlated with BCVA (r=0.33). Fixation was stable and central in five eyes (Figure 2). Fixation was poor central and relatively unstable in one (patient 3) eye with a dense central scotoma (Table 2), which disappeared during follow-up after SRF absorption; fixation remained central at 12-month check and infero-temporal shift of the central fixation was recorded 67 months post-operatively.
Discussion
Timing of surgery and younger age of patients with macula-off RD are important factors for final visual outcome.7 All our patients with a mean age of 58.7±11.0 years at surgery were operated with the same technique within 7 days from macula-off RD onset. In our patients, mean post-operative BCVA slowly improved and reached the same BCVA recorded before RD onset in two out of six cases. A total of 100% of our eyes regained at least 0.6 (Snellen BCVA), as compared with 44% of eyes in a review of 185 patients with macula-off RD.8
Conventional AG remains the most used test for the diagnosis of metamorphopsia, although other tests have been developed, such as the preferential hyperacuity perimeter9 and three-dimensional computer automated threshold AG testing.10 Metamorphopsia, a symptom of retinal distortion from intrinsic retinal disease because of poor orientation of photoreceptors, was found in the majority of patients studied up to 3 years after RD surgery.11 Recently metamorphopsia was reported in 67% of 31 eyes at 2 months after successful scleral buckling procedure for macula-off RD, and in 77% of these eyes TD-OCT showed an abnormal macular structure.6 Both metamorphopsia and deterioration of contrast sensitivity12 can disturb vision-related quality of life after RD surgery. In our six selected patients, AG evidenced different patterns of distorted lines that persisted up to 18 months. At 5 to 6 years after RD surgery, four patients still complained of metamorphopsia, whereas all patients had normal contrast sensitivity at the last check.
Functional recovery after macula-off RD surgery is impaired by the metabolic dysfunction of the photoreceptor–RPE complex with shortening or loss of photoreceptor outer segments that are in close anatomical and functional relationship with their neighbour cells producing important intercellular mediators for cell survival.13 Both TD- and SD-OCT detected SRF, which impairs photoreceptor metabolism, in 12% of 17 eyes at 3–30 months after macula-off RD repair; however, SD-OCT detected better than TD-OCT photoreceptor disruption in 12 vs 76% of cases, respectively.14 Similarly SD-OCT detected distortion of the photoreceptor (IS/OS) junction in 82% of patients operated on for RD.15
The post-operative lack of junction line between photoreceptor cell (IS/OS) layer on TD-OCT after macula-off RD surgery was associated with poorer final visual acuity;16 three eyes of our series with such finding were the only ones that did not recover BCVA recorded before RD onset. Restoration of the photoreceptor cell layer has been progressively noted in these eyes. The back-reflection line from ELM was poorly defined on TD-OCT examination, whereas the integrity of ELM was evident in all eyes on SD-OCT. The ELM preservation presumably indicates that the morphological changes in the photoreceptor layer segments do not extend to cell bodies, and may predict the restoration of the photoreceptor layer in eyes with successful RD repair.17 Gradual recovery of the IS/OS line at the fovea after vitrectomy for RD was also seen in 18 eyes followed up for 6 months.18
Macular SRF persistence up to 6 months, detected with TD-OCT, was significantly associated with poor functional recovery after macula-off RD surgery.19 SRF was found up to 6 months in two (33%) of our cases, but only one eye (patient 3) had incomplete visual recovery with dense scotoma at MP-1 and abnormal photoreceptor IS/OS junction.
The MS in normal subjects can range from 16 to 20 (mean 19.7±0.8 dB) using the MP-1.20 In healthy subjects aged 19–71 years, MS ranges from 13 to 19 (mean 18.3) dB with a linear decline in sensitivity with increasing age.21 In our patients, mean MS threshold slowly improved approaching normal levels at 3 or 6 months post-operatively except in patient 3. Interestingly the weak correlation between our post-operative MP-1 and BCVA results indicate that mean MS is a functional parameter relatively independent from BCVA after macula-off RD repair. Similarly also in clinically significant diabetic macular oedema no correlation was found between mean MS on MP-1 and BCVA.22 Using the same MP-1 unit at all visits, we recorded a 2.2 dB decrease in mean MS at 5 to 6 years after RD surgery, as compared with results at 18-month check. As test-retest variability of MS in patients with macular disease does not exceed 2 dB,23 other factors, including patients’ concentration during testing session should have had a role in MS decrease, especially in patient 4 with high myopia and a 9.5 dB reduction at the final visit.
Areas of abnormal sensitivity on MP-1 were found in six out of seven eyes with photoreceptor disruption or persistent SRF on SD-OCT, after superimposing the C-scan and MP-1 images.14 Conversely, only in one of our patients (patient 3), with SRF up to 6-month check and photoreceptor alteration, MS monitoring showed low values. In the other patients with (patients 4, 5, and 6) or without (patients 1 and 2) OCT abnormalities, MS was within normal limits from 6 months after RD surgery, except in patient 4 at the last check. One reason for this discrepancy is that areas of abnormal sensitivity and MS, which does not provide spatial information, are two different parameters investigated in Smith et al's and in our study, respectively.
We are unaware of other prospective long-term longitudinal morphological and functional detailed studies after RD surgery. The small number of our patients was because of strict selection of eyes without intra-operative complications and post-operative lesions, such as epiretinal membrane, macular hole or cystoid macular oedema that could have biased the results of the multiple scheduled examinations.
In conclusion, photoreceptor damage occurred in our patients with macula-off RD, even if they were successfully operated on within 7 days. Post-operative quality of vision was unsatisfactory because of long-standing metamorphopsia with or without detectable disruption of photoreceptor IS/OS junction, which was less evident with time on TD-OCT and undetectable on SD-OCT at the last follow-up examination, indicating restoration of the photoreceptor layer with integrity of ELM. Marked decrease in MS was found only in one eye with SRF and IS/OS junction photoreceptor disruption. In our patients, long-standing metamorphopsia gradually improved and mean MS increased, but was weakly correlated with BCVA recovery or OCT abnormalities.

References
Ahmadieh H, Moradian S, Faghihi H, Parvaresh MM, Ghanbari H, Mehryar M et al. Anatomic and visual outcomes of scleral buckling versus primary vitrectomy in pseudophakic and aphakic retinal detachment: six-month follow-up results of single operation. Report no. 1. Ophthalmology 2005; 112: 1421–1429.
Theodossiadis PG, Georgalas IG, Emfietzoglou J, Kyriaki TE, Pantelia E, Gogas PS et al. Optical coherence tomography findings in the macula after treatment of rhegmatogenous retinal detachments with spared macula preoperatively. Retina 2003; 23: 69–75.
Abouzeid H, Wolfensberger TJ . Macular recovery after retinal detachment. Acta Ophthalmol Scand 2006; 84: 597–605.
Rossetti A, Doro D . Retained intravitreal lens fragments after phacoemulsification : complications and visual outcome in vitrectomized and non vitrectomized eyes. J Cat Refr Surg 2002; 28: 310–315.
Ross W, Lavina A, Russell M, Maberley D . The correlation between height of macular detachment and visual outcome in macula-off retinal detachments of ≤7 days’ duration. Ophthalmology 2005; 112: 1231–1237.
Wang Y, Li SY, Zhu M, Chen SJ, Liu Y, Men XH et al. Metamorphopsia after successful retinal detachment surgery: an optical coherence tomography study. Acta Ophthalmol Scand 2005; 83: 168–717.
Ross WH . Visual recovery after macula-off retinal detachment. Eye 2002; 16: 440–446.
Doyle E, Herbert EN, Bunce C, Williamson TH, Laidlaw DA . How effective is macula-off retinal detachment surgery. Might good outcome be predicted? Eye 2007; 21: 534–540.
Kampmeier J, Zorn MM, Lang GK, Botros YT, Lang GE . Comparison of preferential hyperacuity perimeter (PHP) test and Amsler grid test in the diagnosis of different stages of age-related macular degeneration. Klin Monatsbl Augenheilkd 2006; 223: 752–756.
Jivrajka RV, Kim JK, Fink W, Sadun AA, Sebag J . Quantitative analysis of central visual defects in macular edema using three-dimensional computer–automated threshold Amsler grid testing. Graefes Arch Clin Exp Ophthalmol 2009; 247: 165–170.
Anderson C, Sjöstrand J . Contrast sensitivity and central vision in reattached macula. Acta Ophthalmol (Copenh) 1981; 59: 161–169.
Okamoto F, Okamoto Y, Hiraoka T, Oshika T . Vision-related quality of life and visual function after retinal detachment surgery. Am J Ophthalmol 2008; 146: 85–90.
Kubay OV, Charteris DG, Newland HS, Raymond G . Retinal detachment neuropathology and potential strategies for neuroprotection. Surv Ophthalmol 2005; 50: 463–475.
Smith AJ, Telander DG, Zawadzski RJ, Choi SS, Morse LS, Werner JS et al. High-resolution fourier-domain optical coherence tomography and microperimetric findings after macula-off retinal detachment repair. Ophthalmology 2008; 115: 1923–1929.
Shocket LS, Witkin AJ, Fujimoto JG, Ko TH, Schuman JS, Rogers AH et al. Ultra-high resolution optical coherence tomography in patients with decreased visual acuity after retinal detachment repair. Ophthalmology 2006; 113: 666–672.
Lecleire-Collet A, Muraine M, Ménard JF, Brasseur G . Evaluation of macular changes before and after successful retinal detachment surgery using Stratus optical coherence tomography. Am J Ophthalmol 2006; 142: 176–179.
Wakabayashi T, Oshima Y, Fujimoto H, Murakami Y, Sakaguchi H, Kusaka S et al. Foveal microstructure and visual acuity after retinal detachment repair imaging analysis by Fourier-domain optical coherence tomography. Ophthalmology 2009; 116: 519–528.
Shimoda Y, Sano M, Hashimoto H, Yokota Y, Kishi S . Restoration of photoreceptor outer segment after vitrectomy for retinal detachment. Am J Ophthalmol 2010; 149: 284–290.
Cavallini GM, Masini C, Volante V, Pupino A, Campi L, Pelloni S . Visual recovery after scleral buckling for macula-off retinal detachment: an optical coherence tomography study. Eur J Ophthalmol 2007; 17: 790–796.
Midena E, Radin PP, Convento E, Cavarzeran F . Macular automatic fundus perimetry threshold versus standard perimetry threshold. Eur J Ophthalmol 2007; 17: 63–68.
Shah VA, Chalam KV . Values for macular perimetry using the MP-1 microperimeter in normal subjects. Ophthalmic Res 2009; 41: 9–13.
Vujosevic S, Midena E, Pilotto E, Radin PP, Chiesa L, Cavarzeran F . Diabetic macular edema: correlation between microperimetry and optical coherence tomography findings. Invest Ophthalmol Vis Sci 2006; 47: 3044–3051.
Chen FK, Patel PJ, Xing W, Bunce C, Egan C, Tufail AT et al. Test-retest variability of microperimetry using the Nidek MP1 in patients with macular disease. Invest Ophthalmol Vis Sci 2009; 50: 3464–3472.
Acknowledgements
We thank Dr Fabiano Cavarzeran and Dr Luigi Spedicato for their support in preparing the article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Rossetti, A., Doro, D., Manfrè, A. et al. Long-term follow-up with optical coherence tomography and microperimetry in eyes with metamorphopsia after macula-off retinal detachment repair. Eye 24, 1808–1813 (2010). https://doi.org/10.1038/eye.2010.138
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2010.138
Keywords
This article is cited by
-
Evaluation of retinal structural and functional changes after silicone oil removal in patients with rhegmatogenous retinal detachment: a retrospective study
International Journal of Retina and Vitreous (2024)
-
Characteristics of patients with complete visual acuity recovery after vitrectomy for macula-off retinal detachment
Eye (2021)
-
Multimodal imaging for detecting metamorphopsia after successful retinal detachment repair
Graefe's Archive for Clinical and Experimental Ophthalmology (2020)
-
Functional and morphological results of treatment of macula-on and macula-off rhegmatogenous retinal detachment with pars plana vitrectomy and sulfur hexafluoride gas tamponade
BMC Ophthalmology (2019)
-
Quantitative assessment of outer retinal folds on enface optical coherence tomography after vitrectomy for rhegmatogenous retinal detachment
Scientific Reports (2019)