Abstract
Little is known about the psychosocial consequences of testing newborns for genetic susceptibility to multifactorial diseases. This study reports quantitative psychosocial evaluations of parents and children 12 years after screening for type 1 diabetes (T1D). Two parent-child cohorts participated: children at increased genetic risk of T1D and children at low genetic risk. T1D risk status was determined at birth as part of a prospective study investigating potential environmental triggers of autoimmunity. Parent measures included ratings of children’s emotional, behavioural and social functioning (Child Behaviour Checklist) and parenting style (Alabama Parenting Questionnaire). Child self-concept was assessed using the self-description questionnaire (SDQ1). Statistical analyses were conducted to test for differences between the groups. Twelve years after testing there was no evidence that knowledge of a child’s increased genetic risk of T1D adversely affected parental ratings of their child’s emotional, behavioural or social functioning, or impacted upon parenting style. There was no adverse effect upon the child’s assessment of their self-concept. This study provides important preliminary data concerning longer-term psychosocial effects of incorporating tests for genetic risk of complex disorders into NBS panels. While it is reassuring that no significant adverse effects have been detected, more data will be required to adequately inform policy.
Similar content being viewed by others
Introduction
WGS is rapidly being integrated into clinical care. Recently, there have been suggestions that ‘genomic newborn screening’ could expand and improve upon existing newborn health care through early diagnosis or prediction of multiple conditions at the very start of life.1, 2 This would represent a considerable departure from existing NBS paradigms. For example, NBS currently focuses predominantly on early detection of rare autosomal recessive metabolic disorders, whereas with WGS it could potentially include reporting of carrier status, non-metabolic single gene disorders and disease susceptibilities for common complex disorders.3 Many scientific questions remain concerning these potential developments, but there is also debate about whether offering such comprehensive genetic testing services in childhood is ethically and/or socially appropriate.4 While there are many issues to consider (including the child’s future autonomy, confidentiality of medical data and informed consent), understanding the potential impact that knowledge of genetic disorders and health risks might have on the psychosocial wellbeing of parents and children is a key element of such discussions.4, 5 This latter issue is amenable to empirical investigation and although relatively under-researched, two recent systematic reviews have assessed the available evidence.6, 7 These early data, largely confined to effects of testing for carrier status or predicting single gene disorders, suggest that serious impacts on traditional psychological parameters such as anxiety and depression are uncommon. However, both reviews highlighted the constrained nature of the data and significant methodological limitations of many studies. They suggest an urgent need to broaden the scope of research through addressing responses to ‘genomic’ or ‘susceptibility’ tests, and to explore some of the more subtle and longer-term effects that genetic testing may produce in children. These effects may include potential disruptions to children’s developing identities, and complex family or social impacts that might initially be best explored using mixed methods approaches.6, 7
The study reported here aims to begin to address some of these issues in the context of genomic NBS, by providing 12-year follow-up data for a cohort of children tested at birth for genetic susceptibility to a single condition, type 1 diabetes (T1D). T1D represents a useful disease model, both for studying the complex genetic and environmental interactions underlying multifactorial disease development and for investigating psychological reaction to newborn testing. It has been the subject of several large-scale longitudinal studies.8, 9 The present study builds upon our previous reports of maternal psychological reactions in the first year after testing,10 at child age 3 years11 and a recent qualitative report of parents experiences after 12 years.12 We report here the quantitative psychological evaluation of two mother-child groups (increased and low genetic risk) designed to investigate the potentially complex and time-varying interactions between: parental perceptions of their child’s risk of T1D, parental concern regarding their child’s genetic risk, parental rating of their child’s behaviour, parenting style and the child’s own evaluation of self-concept.
Materials and methods
Recruitment
Participants were drawn from the Dunedin (New Zealand)-based Key Environmental Aspects of T1D study (the KEA study) investigating the natural history of T1D. In the KEA study, 41 infants, 8.2% of those screened, were found to be at increased risk on the basis of T1D susceptibility genes at HLA-DRB.10 Increased risk results were disseminated by letter to parents stating that their child was at ‘increased risk of developing diabetes…with a one in 16 risk [6.25%]…compared to the general population risk of one in 300 [~0.3%]’. Families were also provided with verbal and written information concerning T1D, including its management, and that there were no known preventive measures at the time. The issue of if and when to advise their children of the test results was not discussed. A full description of the KEA study protocol has been published elsewhere.10 The KEA study itself ran for 3 years and at this stage all families of children at increased genetic risk were offered annual antibody surveillance (appearance of diabetes-related autoantibodies in genetically susceptible young children is highly predictive of future development of T1D13). One child subsequently developed single-antibody positivity and was entered into TrialNet (http://www.diabetestrialnet.org/). No children have developed T1D to date. (There is a small peak in incidence of T1D for boys at age 5 years and then a larger one for both sexes around puberty, 10-14yrs. However, 50% of cases present after age 20 years.)
For the study reported here, two of the original mother-child groups in the cohort (increased genetic risk of T1D and low risk) involved in the quantitative assessment of maternal mental state up to one year after testing10 were invited to participate. (The initial control group who had not undergone any genetic testing for T1D was not included.) Questionnaires were administered to mothers and children during home visits or by post, depending upon participant preference. Nonresponse prompted a follow-up telephone call after 2 weeks.
Study design
The study consisted of a single questionnaire administered to a primary caregiver of the child (usually the mother, but the father in n=2 cases) and a separate questionnaire for the child to complete at age 12 years±15 months. Questionnaires were completed simultaneously. In all, 35 of 38 (92%) possible participants in the increased genetic risk group completed the study, and 65/76 (86%) in the low risk group.
Questionnaires/measures
Parent measures
The parent survey consisted of six sections. Sections 2 and 3 (below) formed part of the previous survey administered to these cohorts at child age 1 year allowing evaluation of changes over time.
Demographic data
This included age, ethnicity, self-reported health status (indicated health status on scale from 1 to 5 with 1 being excellent and 5 very poor) and the presence of any current health problems for both parents. Family history of diabetes (type 1 or type 2) was recorded and whether the index child had a first-degree relative with T1D.
Perception of child’s risk of developing T1D
Parents recorded how they viewed their child’s risk of developing T1D on a 5-point rating scale ranging from ‘no risk at all’ (1) to ‘certain to develop diabetes’ (5) with an option for ‘uncertain’.
Subjective rating of level of concern about T1D genetic susceptibility test result
Assessed using two questions concerning how much the parent (1) thinks and (2) worries about the child’s genetic test result recorded on a 7-point scale from ‘not at all’ (0) to ‘all the time’ (6).
Disclosure of the genetic test result to the child
Investigated using two questions concerning (1) whether the child is aware of their genetic test result (including an option for unsure) and (2) what age the child was told the result (years).
The Child Behavior Checklist (CBCL/6-18)
The CBCL/6-1814 is a widely used parent-completed checklist assessing children’s emotional, behavioural and social functioning. It is frequently used as a diagnostic tool for behavioural and emotional problems such as attention deficit hyperactive disorder, conduct disorder and childhood depression, and has also been used extensively in a research context.15, 16 It is designed for use with children aged 6-18 and the syndrome profile utilised in this study consists of 113 questions about child functioning, scored on a 3-point ordinal scale (0=absent, 1=occurs sometimes, 2=occurs often). The time frame for item responses is the past six months. The 2001 revision of the CBCL/6-18 is made up of eight syndrome scales: anxious/depressed (minimum score 0–maximum score 26); depressed (0–16); somatic complaints (0–22); social problems (0–22); thought problems (0–30); attention problems (0–20); rule-breaking behaviour (0–34); aggressive behaviour (0–36). Additionally, a total problem score can be calculated. Raw scores were used in statistical analysis for this study.
Studies have reported good internal consistency (Cronbach’s alpha coefficients from 0.71 to 0.97), good inter-interviewer and test re-test reliabilities (supported by intraclass correlation coefficients of 0.93 to 1.00 for the mean item scores obtained by different interviewers and reports by parents on two occasions seven days apart)14, 17 Further evidence for construct validity is extensive, and includes correlations from 0.59 to 0.88 with the Conner’s Parent Questionnaire (1973) and the Revised Behavior Problem Checklist (Quay 1983).18
The Alabama Parenting Questionnaire (APQ)
The APQ is designed to assess parenting practices across a number of domains. This study employed the parent measure consisting of 42 items presented with a 5-point Likert-type endorsement scale. The items are divided into five subscales: Involvement (minimum score 10–maximum score 50), Positive Parenting (6–30), Poor Monitoring/Supervision (10–50), Inconsistent Discipline (6–30), Corporal Punishment (4–20). Other Discipline Practices is not a scale, but provides information on an item-by-item basis. Internal consistency of subscales has generally been reported as adequate to good (alphas of 0.54–0.83) although is lower for corporal punishment (<0.4–0.59). Reported test-retest reliability coefficients vary from 0.66-0.89.19, 20
Child measures
Demographic data
Age (years), sex (M/F), height (cm), weight (kg) and ethnicity were recorded.
The child measure consisted of a single questionnaire:
The Self-Description-Questionnaire 1 (SDQ1)
The Self-Description-Questionnaire 1 (SDQ1)21 is a measure of pre-adolescent self-concept based on Shavelson’s multidimensional hierarchical model.22 It consists of 76 items designed to measure self-perceptions relative to four non-academic areas (physical ability, physical appearance, peer relations and parent relations) and three academic areas (reading, mathematics and school in general) as well as a global perception of self. Of the 76 items, 12 negatively worded items are included to reduce positive response bias, but these are not included in the final self-concept scores as young children have difficulty with items of this type.21 As a result, the SDQ1 score is based on 64 items all measured using 5-point Likert-type responses (false, mostly false, sometimes false/sometimes true, mostly true, true). Scores are reported as total non-academic (sum of the first four factors), total academic (sum of the next three factors), total self (sum of the seven factors) and the general self-subscale is reported separately. The scale has been used extensively and has excellent internal consistency (coefficient alphas from 0.81 to 0.94 for the individual scales and 0.94 for the total scores) and relative stability over time (individual scales mean r 0.61; total scores mean r =0.65).21
Ethical approval
The study was approved by the Central Health and Disability Ethics Committee (ref 13/CEN/195).
Statistical analysis
Appropriate summary statistics are presented for all measures of interest: means and standard deviations for approximately normally distributed continuous measurements, medians and Interquartile Ranges (IQRs) for non-normally distributed continuous measurements, and frequencies and percentages for categorical measurements. As children in the high- and low-risk groups were approximately matched on age and sex whenever possible, they were not compared in terms of these two variables but other child and parent characteristics were compared between the groups using t-tests where values were normally distributed, Mann-Whitney-Wilcoxon where values were not normally distributed, and Chi-squared or Fisher’s Exact tests for categorical variables (Fisher’s exact being used where 20% or more of the cells had expected counts below 5). The matching (a mixture of 1:1 and 1:2) was not incorporated into these comparisons of baseline characteristics. Scales and subscales were assessed for internal consistency in this population using Cronbach’s alphas with values ≥0.7 considered desirable.
Low- and high-risk children were then compared with regard to follow-up measures using mixed models, with a random effect for the matching, in terms of perceived risk (modelled using mixed ordinal logistic regression), frequency of thinking and worrying about results (both modelled using mixed linear regression), whether child was informed (modelled using mixed logistic regression) and if so, the age child was informed (modelled using mixed linear regression).
CBCL and Alabama scores were compared between the two groups using mixed linear regression models (with a random effect for the matching) following a natural logarithmic transformation after adding one due to zeros. SDQ1 scores were compared in the same way but on the original scale. All mixed models included child age and child sex as covariates to account for possible residual confounding from the imperfect matching. Model diagnostics included examining model residuals for evidence of heteroscedasticity and/or non-normality and this informed the use of logarithmic transformations. All analyses were conducted using Stata 13.1 and (two-sided whenever possible) P<0.05 was considered statistically significant in each case.
Results
Population characteristics
There was no evidence of statistically significant differences between the two cohorts (all P≥0.108) and the observed differences were not considered of practical importance. These data are displayed in table 1.
Questionnaire scores
Parental perception of risk
Data concerning how parents perceived their child’s risk of developing T1D are displayed in table 2. Eleven per cent of parents with children in the low risk group and 41% in the increased risk group underestimated their child’s risk of developing T1D.
Data concerning parents’ subjective rating of their concern about their child’s genetic risk of T1D are reported in table 3.
Parental ‘thinking about test result’
Parents of children in the increased risk group reported thinking (P<0.001) about the genetic test result significantly more than parents with children in the low-risk group.
Parental ‘worrying about test result’
Parents of children in the increased risk group also reported worrying (P<0.001) about the genetic test result significantly more than parents with children in the low-risk group.
Disclosure of test result to child
Data concerning disclosure of the genetic test result to the child are also included in table 3. Parents reported that children in the increased risk group (79%) were significantly more likely to be aware of their genetic risk compared to the low-risk group (43%) (P<0.003) and had been informed at a younger age (9.86 years, 11.03 years, P<0.008).
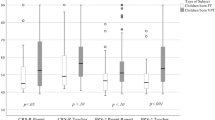
Child behaviour checklist
Data concerning parental reports of their child’s emotional, behavioural and social functioning (CBCL) are displayed in table 4. Statistically significant differences between the increased risk and low-risk groups were found in 1 subscale (aggressive behaviour) (P<0.029) and the total score (p <0.047) with those at increased risk reported to be exhibiting less externalising (aggressive) behaviour than those at low risk of T1D.
In addition, a difference between the two groups on the anxious/depressed subscale was almost statistically significant (P<0.052) with the increased risk group again having lower scores than the low-risk group on this domain.
Alabama parenting questionnaire
Data about parenting style (APQ) are reported in Table 5 and demonstrate no differences between the two groups of parents on any of the five subscales.
Child self-concept
Data concerning child self-concept (SDQ1) is reported in Table 6. Statistically significant differences between the increased risk and low-risk group exist on the reading subscale (P<0.010) and the composite total academic scale (P<0.048) with the children at increased risk rating their abilities more favourably than those at low risk.
Discussion
While there is considerable enthusiasm for incorporating NGS into clinical practices such as NBS there remain many unanswered questions. One of the most important gaps in the literature concerns the potential impact that knowledge of genetic health risks or susceptibilities might have on the psychosocial wellbeing of children and families, particularly in the longer term. This study provides preliminary empirical evidence through quantitative psychological analysis of increased and low genetic risk parent-child cohorts 12 years after NBS for genetic risk of T1D.
The key findings are that 12 years after testing there was no evidence that knowledge of a child’s increased genetic risk of T1D adversely affected parental ratings of their child’s emotional, behavioural or social functioning, or impacted upon their parenting style. In addition such knowledge did not adversely affect the child’s assessment of their self-concept. This may at least partially be explained by the finding that half of the parents with children in the increased risk group either underestimated or were uncertain of their child’s risk of developing T1D.
Perception of risk
Parental perception of risk has changed over time, with only 50% of the increased genetic risk group considering their children to be at ‘greater risk than most people’ at this 12-year analysis compared to 92% in our previous assessment at 1 year.10 Underestimation of risk occurred in both the increased risk and low-risk groups with 11% of parents in the low-risk group believing their child to be at no risk of T1D and 41% of parents in the increased risk group believing their child to be at the same risk as most people or lower.
For the increased risk group these findings may have been influenced by the fact that parents correctly recognised that many children with T1D would have presented by the time they reached age 12 years. However, as 50% of cases occur after age 20 years, these children remain at ‘higher risk than most people’ even though their absolute risk is small, and has diminished somewhat with time. Alternatively these findings may simply reflect a common phenomenon described in the genetic counselling literature: risk under-estimation occurs frequently, and may increase over time unless risk statistics are repeated.9, 23, 24, 25, 26 Such perceptions are likely to be reinforced by a child’s ‘normal’ appearance and apparent good health.12
Subjective ratings of concern
Despite these under-estimations of risk parents in the increased risk group reported thinking and worrying about their child’s genetic test result more than parents in the low-risk group. However, their level of concern was at the lower end of our Likert-type scale (median of 1 on a 6-point scale) and had diminished since our previous study at 1 year when mean rating for ‘worry’ in the increased risk group was 2.2.10 These results suggest that in general parents are not unduly concerned about their child’s risk of T1D, with support for this supposition coming from our recent interviews with parents in which they reported largely relegating their child’s genetic risk of T1D to the back of their minds, believing it had very little ongoing impact on their family lives.12
Disclosure of results to child
Twice as many parents in the increased risk group reported that their child was aware of the test result (79 versus 43%) and said that their children were informed at a significantly younger age (9.9 years versus 11.0 years) than the low-risk group. Interestingly, in our qualitative interview study conducted with a subset14 of the increased risk group parents at a similar time to this study, most parents reported not discussing the test result with their child until re-contacted for the study (ie, when the children were approximately 12 years old). However, the majority of these parents felt that their child had been aware of the information prior to this, and while they could not recall a specific discussion, felt that the information had ‘just always been talked about’.12 Parental responses to our question concerning what age the child was told the genetic test result in the study described here may be reflective of this phenomenon. This finding is consistent with data from other studies that acknowledge that children may learn about genetic information gradually as part of growing up, and that this may make the new information and its implications easier to cope with.27, 28 Such findings may have broader relevance to genetic testing in childhood, perhaps challenging traditionally cautious and restrictive genetic counselling views and practice guidelines.
Parent measures: child behaviour and parenting
Our CBCL data suggest that parents with children in the increased genetic risk group view them slightly more ‘positively’ than parents of children in the low-risk group. In particular, they report lower rates of ‘aggressive behaviour’ as well as lower total scores. However, while both of these findings are statistically significant without adjustment for multiple comparisons, neither would be significant under a Bonferroni adjustment for this set of comparisons, and all scores fall well below published borderline clinical cut-offs for aggressive behaviour12 and total score (60).14, 29 As such, the observed differences may be of limited clinical relevance. If these findings were to be confirmed in future studies, they could be related to the ‘double protection’ mechanism whereby a ‘positive illusion’ may result from children giving parents the impression they are doing fine to protect their parents from negative emotions.30
Although we detected subtle differences in parents’ ratings of their child’s behaviour they did not translate into any significant differences in parenting style between the groups. This is perhaps unsurprising as previous studies investigating parenting in the context of children with chronic physical illnesses have documented only small differences for some diseases and not for others.31 Overall, a meta-analysis concluded that most families adapt well to a child’s chronic illness and generally establish parenting behaviours that are as positive as they are in families with healthy children.31 Our data suggest this is also true for parenting in the context of genetic risk of T1D.
Child self-concept
Using a multi-dimensional measure of self-concept our data demonstrate no difference in total scores between the increased risk and low-risk children (P=0.085). In fact, children in the increased risk group perceived their reading abilities more positively than children in the low-risk group (P<0.010), a finding that was also reflected in the total academic score (P<0.048). Again these findings require replication before any firm conclusions can be drawn, but they could reflect a greater level of ‘academic confidence’ in these children. This confidence may be easier to maintain in a subject such as reading that is perhaps more subjective and less easily or obviously open to rigid external assessment than other academic areas such as mathematics.
The finding that knowledge of risk of T1D (a ‘genomic’ test) does not appear to adversely affect a child’s developing identity is important as the need for such data has recently been highlighted.6, 32 Previous research investigating the impact of testing children for single gene disorders has employed similar measures, and in general these studies also report no adverse effect of knowledge of genetic status upon concepts such as self-esteem.7 Similarly studies that have employed more general quality of life or wellbeing measures with children known to be at genetic risk of single gene disorders have generally identified no problems.6, 33
Limitations
This study provides preliminary evidence from exploratory analyses. The statistically significant results for the CBCL and SDQ1 outcomes would not be considered significant following Bonferroni adjustment, or the less conservative Holm-Bonferroni step-down procedure, applied separately for each set of measures and so replication is imperative prior to these results informing practice or policy. Secondly, although retention of participants was excellent for a longitudinal study of this nature, results may not be generalisable to other populations and replication in other settings is required. Third, the study reports on the impact of genetic testing for a single condition, T1D. Reactions to risk of this manageable disorder may be very different from those in relation to more severe or lethal disorders. Similarly future possibilities include the possibility of multiplex testing that may also provoke quite different responses. While this study addressed potential psychosocial effects upon both parents and children, it did not extend to children’s peers or other social contexts such as school. These factors become increasingly relevant as children mature and are worthy of inclusion in future studies.
Conclusion
New technologies are changing the landscape of genetic testing in childhood but psychosocial implications remain a key consideration. Studies investigating short-term psychological outcomes, largely related to testing for single gene disorders, have revealed few adverse outcomes. But it is widely acknowledged that evidence concerning newer ‘genomic’ tests, and longer-term psychological data, are lacking. This study has provided such preliminary data.
Twelve years after testing there was no evidence that knowledge of a child’s increased genetic risk of T1D adversely affected parental ratings of their child’s emotional, behavioural or social functioning, or impacted upon parenting style. There was also no adverse effect up on the child’s assessment of their self-concept. Our preliminary findings show that children in the increased risk group were rated slightly more favourably both by their parents, in relation to behaviour and by themselves with regard to academic self-concept.
While it is reassuring that no significant adverse effects have been detected, more data will be required to adequately inform policy. Future studies should also aim to capture and evaluate the potentially broad range of subtle psychosocial responses, both positive and negative, that may arise when conveying complex genetic information in childhood. In particular, as the pace of clinical implementation of genomic approaches increases, such research should focus on the appropriate balance between how parents, children and their peers perceive genetic risk, their psychosocial wellbeing and motivation for behaviour change.
References
Health NIo: NIH program explores the use of genomic sequencing in newborn healthcare. News release 2013.
Collins F : The language of life: DNA and the revolution in personalised medicine. New York: Harper perennial, 2010.
Hall AE, Chowdhury S, Pashayan N, Hallowell N, Pharoah P, Burton H : What ethical and legal principles should guide the genotyping of children as part of a personalised screening programme for common cancer? J Med Ethics 2014; 40: 163–167.
Knoppers BM, Senecal K, Borry P, Avard D : Whole-genome sequencing in newborn screening programs. Sci transl med 2014; 6: 229cm2.
Howard HC, Knoppers BM, Cornel MC et al: . Whole-genome sequencing in newborn screening? A statement on the continued importance of targeted approaches in newborn screening programmes. Eur J Hum Genet 2015; 23: 1593–1600.
Wakefield CE, Hanlon LV, Tucker KM et al: The psychological impact of genetic information on children: a systematic review. Genet Med 2016; 18: 755–762.
Wade CH, Wilfond BS, McBride CM : Effects of genetic risk information on children's psychosocial wellbeing: a systematic review of the literature. Genet med 2010; 12: 317–326.
Hagopian W, Erlich H, Lernmark A et al: The Environmental Determinants of Diabetes in the Young (TEDDY): genetic criteria and international diabetes risk screening of 421 000 infants. Pediatr Diabetes 2011; 12: 733–743.
Carmichael SK, Johnson SB, Baughcum A et al: Prospective assessment in newborns of diabetes autoimmunity (PANDA): maternal understanding of infant diabetes risk. Genet Med 2003; 5: 77–83.
Kerruish NJ, Campbell-Stokes PL, Gray A, Merriman TR, Robertson SP, Taylor BJ : Maternal psychological reaction to newborn genetic screening for type 1 diabetes. Pediatrics 2007; 120: e324–e335.
Kerruish NJ : Parents' experiences of newborn screening for genetic susceptibility to type 1 diabetes. J Med Ethics 2011; 37: 348–353.
Kerruish N : Parents' experiences 12 years after newborn screening for genetic susceptibility to type 1 diabetes and their attitudes to whole-genome sequencing in newborns. Genet Med 2015; 18: 249–258.
Devendra D, Liu E, Eisenbarth GS : Type 1 diabetes: recent developments. Bmj 2004; 328: 750–754.
Achenbach T, Rescoria L : Manual for the ASEBA school age forms and profiles. Burlington, VT: University of vermont, Research center for children, youth and families, 2001.
Bellina M, Brambilla P, Garzitto M, Negri GA, Molteni M, Nobile M : The ability of CBCL DSM-oriented scales to predict DSM-IV diagnoses in a referred sample of children and adolescents. Eur Child Adolesc Psychiatry 2013; 22: 235–246.
Pesenti-Gritti P, Scaini S, D'Ippolito C, Fagnani C, Battaglia M : A genetically informed study of the covariation between the CBCL/6-18 DSM-oriented problem scales and the competence scales. Behav genet 2011; 41: 522–532.
Nakamura B, Ebesutani C, Bernstein A, Chorpita B : A psychometric analysis of the child behavior checklist DSM-oriented scales. J Psychopathol Behav Assess 2009; 31: 178–189.
Mazefsky C, Anderson RR, Conner C, Minshew N : Child behaviour checklist scores for school aged children with autism: preliminary evidence of patterns suggesting the need for referral. J psychopathol Behav assess 2011; 33: 31–37.
Shelton K, Frick P, Wootoa J : Assessment of parenting practices in families of elementary school age children. J clin child psychol 1996; 25: 317–329.
Dadds M, Maujean A, Fraser J : Parenting and conduct problems in children: Australian data and psychometric properties of the Alabama parenting Questionnaire. Aust psychol 38: 238–241.
Marsh H (ed): Self Description Questionnaire (SDQ) 1: A Theoretical and Empirical Basis for Measurement of Multiple Dimensions of Preadolescent self concept: An interim Test Manual and Research Monograph. Macarthur: Faculty of education, University of western Sydney, 1992.
Shavelson R, Hubner J, Stanton G : Self concept: validation of construct interpretations of test scores. Rev educ Res 1976; 46: 407–441.
McBride CM, Koehly LM, Sanderson SC, Kaphingst KA : The behavioral response to personalized genetic information: will genetic risk profiles motivate individuals and families to choose more healthful behaviors? Annu Rev Public Health 31: 89–103.
Hopwood P : Breast cancer risk perception: what do we know and understand? Breast Cancer Res 2000; 2: 387–391.
Heshka JT, Palleschi C, Howley H, Wilson B, Wells PS : A systematic review of perceived risks, psychological and behavioral impacts of genetic testing. Genet Med 2008; 10: 19–32.
Hood KK, Johnson SB, Baughcum AE, She JX, Schatz DA : Maternal understanding of infant diabetes risk: differential effects of maternal anxiety and depression. Genet Med 2006; 8: 665–670.
Metcalfe A, Coad J, Plumridge GM, Gill P, Farndon P : Family communication between children and their parents about inherited genetic conditions: a meta-synthesis of the research. Eur J Hum Genet 2008; 16: 1193–1200.
Metcalfe A, Plumridge G, Coad J, Shanks A, Gill P : Parents' and children's communication about genetic risk: a qualitative study, learning from families' experiences. Eur J Hum Genet 2011; 19: 640–646.
Nolan TM, Bond L, Adler R et al: Child Behaviour Checklist classification of behaviour disorder. J Paediatr Child Health. 1996; 32: 405–411.
Grootenhuis M, Last B, van Der Wel M, de Graaf-Nikerk J : Parents' attribution of positive characteristics to their child with cancer. Psychol Health 1998; 13.
Pinquart M : Do the parent–child relationship and parenting behaviors differ between families with a child with and without chronic illness? A meta analysis. J Pediatr Psychol 2013; 38: 708–721.
Wilfond BS, Diekema DS : Engaging children in genomics research: decoding the meaning of assent in research. Genet med 2012; 14: 437–443.
Smets EM, Stam MM, Meulenkamp TM et al: Health-related quality of life of children with a positive carrier status for inherited cardiovascular diseases. Am j med genet. Part A 2008; 146A: 700–707.
Acknowledgements
This study was funded by a University of Otago Research Grant. The authors are grateful to Jane Columb and Shirley Jones (research nurses) for assistance with data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kerruish, N., Healey, D. & Gray, A. Psychosocial effects in parents and children 12 years after newborn genetic screening for type 1 diabetes. Eur J Hum Genet 25, 397–403 (2017). https://doi.org/10.1038/ejhg.2016.190
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejhg.2016.190
This article is cited by
-
Früherkennungsuntersuchungen zum Typ-1-Diabetes
Der Diabetologe (2018)