Abstract
Background/objectives:
Although previous studies reported that calcium supplementation can effectively improve bone mineral density in postmenopausal women, some studies showed the reverse conclusion. One of the reasons was that most of the studies did not take into full consideration the information of noncompliers, which seriously influenced the precision of conclusion. The aim of this paper was to investigate the effect of calcium supplementation on bone mineral density with correcting impact of noncompliance using the complier average causal effect (CACE).
Subjects/methods:
A randomized controlled trial was designed to investigate the effect of high-calcium milk powder on bone mineral density. One hundred and forty-one postmenopausal women were randomly assigned to either a control group (n=72) or a milk powder supplementation group (n=69). The participants in the intervention group took 50 g of high-calcium milk powder containing 450 mg of elemental calcium and 400 IU vitamin D every morning and evening, respectively. The effects of the intervention on the primary outcome, bone mineral density, were assessed using the CACE model and intention-to-treat (ITT) and per-protocol (PP) analyses.
Results:
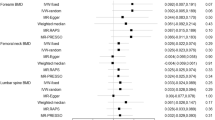
Using the CACE model, the calcium supplementation was found to significantly reduce the bone loss at the lumbar spine compared with the control group at 24 months when adjusting the covariates (effect size 1.170, 95% confidence interval (CI) 0.376~1.964, P=0.0040). At the hip site, there was no significant difference between the calcium group and the control group. Compared with the control group, no significant weight gain was found in the calcium group over 24 months. However, the calcium group had less height loss at 24 months (effect size 1.040, 95% CI 0.012~2.066, P=0.0470) than the control group. High-density lipoprotein was significantly increased in the calcium group at 12 months (effect size 0.120, 95% CI 0.009~0.232, P=0.0340). Serum total cholesterol, triglyceride and low-density lipoprotein were not affected over 24 months. The estimates of complier average causal effect of latent ignorability model with missing data assumption of latent ignorability were consistent with the CACE estimates.
Conclusion:
Consumption of high-calcium milk powder is effective in reducing the bone loss at the lumbar spine among healthy postmenopausal women. Supplementing with high-calcium milk powder had additional benefits of reducing height loss.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Lau EM, Cooper C . The epidemiology of osteoporosis. The oriental perspective in a world context. Clin Orthop Relat Res 1996; 323: 65–74.
Chee W, Suriah A, Chan S, Zaitun Y, Chan Y . The effect of milk supplementation on bone mineral density in postmenopausal Chinese women in Malaysia. Osteoporos Intl 2003; 14: 828–834.
Cooper L, Clifton-Bligh PB, Nery ML, Figtree G, Twigg S, Hibbert E et al. Vitamin D supplementation and bone mineral density in early postmenopausal women. Am J Clin Nutr 2003; 77: 1324–1329.
Price PA . Vitamin K nutrition and postmenopausal osteoporosis. J Clin investig 1993; 91: 1268.
Binkley NC, Suttie JW . Vitamin K nutrition and osteoporosis. J Nutr 1995; 125: 1812–1821.
Imbens GW, Rubin DB . Bayesian inference for causal effects in randomized experiments with noncompliance. Ann Stat 1997; 5: 305–327.
Frangakis CE, Rubin DB . Addressing complications of intention-to-treat analysis in the combined presence of all-or-none treatment-noncompliance and subsequent missing outcomes. Biometrika 1999; 86: 365–379.
Cheng J, Small DS . Bounds on causal effects in three‐arm trials with non‐compliance. J R Stat Soc 2006; 68: 815–836.
Peng Y, Little RJ, Raghunathan TE . An extended general location model for causal inferences from data subject to noncompliance and missing values. Biometrics 2004; 60: 598–607.
Jo B . Model misspecification sensitivity analysis in estimating causal effects of interventions with non‐compliance. Stat Med 2002; 21: 3161–3181.
Little RJ, Long Q, Lin X . A comparison of methods for estimating the causal effect of a treatment in randomized clinical trials subject to noncompliance. Biometrics 2009; 65: 640–649.
Hirano K, Imbens GW, Rubin DB, Zhou X-H . Assessing the effect of an influenza vaccine in an encouragement design. Biostatistics 2000; 1: 69–88.
Welsh AW . Randomised controlled trials and clinical maternity care: moving on from intention-to-treat and other simplistic analyses of efficacy. BMC Pregnancy Childbirth 2013; 13: 15.
Dodd S, White IR, Williamson P . Nonadherence to treatment protocol in published randomised controlled trials: a review. Trials 2012; 13: 84.
Schwartz S, Li F, Reiter JP . Sensitivity analysis for unmeasured confounding in principal stratification settings with binary variables. Stat Med 2012; 31: 949–962.
Angrist JD, Imbens GW, Rubin DB . Identification of causal effects using instrumental variables. J Am Stat Assoc 1996; 91: 444–455.
Rubin DB . Causal inference through potential outcomes and principal stratification: application to studies with ‘censoring’ due to death. Stat Sci 2006; 21: 299–309.
Jo B, Ginexi EM, Ialongo NS . Handling missing data in randomized experiments with noncompliance. Prev Sci 2010; 11: 384–396.
Knox CR, Lall R, Hansen Z, Lamb SE . Treatment compliance and effectiveness of a cognitive behavioural intervention for low back pain: a complier average causal effect approach to the BeST data set. BMC Musculoskelet Disord 2014; 15: 17.
Dunn G, Maracy M, Dowrick C, Ayuso-Mateos JL, Dalgard OS, Page H et al. Estimating psychological treatment effects from a randomised controlled trial with both non-compliance and loss to follow-up. Br J Psychiatry 2003; 183: 323–331.
Little RJ, Yau LH . Statistical techniques for analyzing data from prevention trials: treatment of no-shows using Rubin's causal model. Psychol Methods 1998; 3: 147.
Heckman J, Smith J, Taber C . Accounting for dropouts in evaluations of social programs. Rev Economics Stat 1998; 80: 1–14.
Donato A, Wija VS, Tom A, Francois B, Steven B, Juliet C et al. Report on osteoporosis in the European Community: action for prevention. Luxembourg: Office for Official Publications of the European Communities: Directorate-General for Employment, Industrial Relations and Social Affairs Directorate V/F.2 1998.
Skrondal A, Rabe-Hesketh S . Some applications of generalized linear latent and mixed models in epidemiology: repeated measures, measurement error and multilevel modeling. Norsk Epidemiol 2003; 13: 265–278.
Kruger M, Ha P, Todd J, Kuhn-Sherlock B, Schollum L, Ma J et al. High-calcium, vitamin D fortified milk is effective in improving bone turnover markers and vitamin D status in healthy postmenopausal Chinese women. Eur J Clin Nutr 2012; 66: 856–861.
Prince R, Devine A, Dick I, Criddle A, Kerr D, Kent N et al. The effects of calcium supplementation (milk powder or tablets) and exercise on bone density in postmenopausal women. J Bone Miner Res 1995; 10: 1068–1075.
Storm D, REES Porter, Musgrave K, Vereault D, Patton C, Kessenich C et al. Calcium Supplementation Prevents Seasonal Bone Loss and Changes in Biochemical Markers of Bone Turnover in Elderly New England Women: A Randomized Placebo-Controlled Trial 1. J Clin Endocrinol Metab 1998; 83: 3817–3825.
Chee WS, Suriah AR, Chan SP, Zaitun Y, Chan YM . The effect of milk supplementation on bone mineral density in postmenopausal Chinese women in Malaysia. Osteoporos Int 2003; 14: 828–834.
Dunn G, Maracy M, Tomenson B . Estimating treatment effects from randomized clinical trials with noncompliance and loss to follow-up: the role of instrumental variable methods. Stat Methods Med Res 2005; 14: 369–395.
Li S, Na L, Li Y, Gong L, Yuan F, Niu Y et al. Long-term calcium supplementation may have adverse effects on serum cholesterol and carotid intima-media thickness in postmenopausal women: a double-blind, randomized, placebo-controlled trial. Am J Clin Nutr 2013; 98: 1353–1359.
Acknowledgements
We thank Zhiqiang Wang and Yang Yang for their help with the language and constructive suggestions. This study was funded by the National Key Technology R&D Program of China (2011BAI09B02).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Chen, Y., Zhang, Q., Wang, Y. et al. Estimating the causal effect of milk powder supplementation on bone mineral density: a randomized controlled trial with both non-compliance and loss to follow-up. Eur J Clin Nutr 69, 824–830 (2015). https://doi.org/10.1038/ejcn.2015.3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2015.3
This article is cited by
-
Dairy products and bone health
Aging Clinical and Experimental Research (2021)
-
The effect of milk consumption on bone and fracture incidence, an update
Aging Clinical and Experimental Research (2019)