Abstract
Background/Objectives:
Postprandial hyperlipidemia, which is exaggerated and prolonged in insulin-resistant individuals, has been associated with cardiovascular disease. The objective of this study was to investigate whether and how the composition, size and function of high-density lipoprotein (HDL) and low-density lipoprotein (LDL) particles are affected in the postprandial state among males with the metabolic syndrome (MetS) or type 2 diabetes (T2DM), compared with controls.
Subjects/Methods:
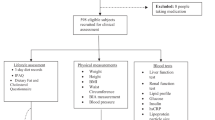
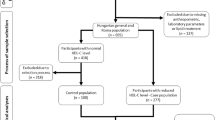
A total of 14 males with T2DM, 14 with the MetS and 14 age-matched controls were given three standardized high-fat mixed meals (900 kcal; 50-g fat, 75-g carbohydrate and 35-g protein) as breakfast, lunch and dinner. Blood sampling was performed just before each meal, and 4 and 8 h after the last meal. HDL and LDL were isolated by ultracentrifugation and analyzed for their composition, particle diameter and functional properties.
Results:
Postprandial triglycerides levels in plasma, HDL and LDL particles increased significantly in all groups (P<0.01). Compared with the control subjects, patients with T2DM had smaller LDL particles, and in agreement, a lower cholesterol-to-protein content in both fasting and postprandial samples. A prolonged increase in susceptibility of LDL to oxidation was found in all subjects, but was most evident in T2DM. The postprandial effect on LDL oxidation was associated with an increase in LDL triglyceride (r=0.29, P<0.05). In T2DM the anti-oxidative capacity of HDL trended to impairment after the third meal.
Conclusions:
Postprandial increases in triglycerides, especially in T2DM, are accompanied by pro-atherosclerotic functional changes in HDL and LDL particles.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Bansal S, Buring JE, Rifai N, Mora S, Sacks FM, Ridker PM (2007). Fasting compared with nonfasting triglycerides and risk of cardiovascular events in women. JAMA 298, 309–316.
Blackburn P, Cote M, Lamarche B, Couillard C, Pascot A, Tremblay A et al. (2003). Impact of postprandial variation in triglyceridemia on low-density lipoprotein particle size. Metabolism 52, 1379–1386.
Bowen PE, Borthakur G (2004). Postprandial lipid oxidation and cardiovascular disease risk. Curr Atheroscler Rep 6, 477–484.
Cardona F, Tunez I, Tasset I, Garrido-Sanchez L, Collantes E, Tinahones FJ (2008). Circulating antioxidant defences are decreased in healthy people after a high-fat meal. Br J Nutr 100, 312–316.
Ceriello A, Quagliaro L, Piconi L, Assaloni R, Da Ros R, Maier A et al. (2004). Effect of postprandial hypertriglyceridemia and hyperglycemia on circulating adhesion molecules and oxidative stress generation and the possible role of simvastatin treatment. Diabetes 53, 701–710.
Cleeman JI (2001). Executive summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 285, 2486–2497.
Diwadkar VA, Anderson JW, Bridges SR, Gowri MS, Oelgten PR (1999). Postprandial low-density lipoproteins in type 2 diabetes are oxidized more extensively than fasting diabetes and control samples. Proc Soc Exp Biol Med 222, 178–184.
Foger B, Trobinger G, Ritsch A, Lechleitner M, Hopferwieser T, Menzel HJ et al. (1995). Treatment of primary mixed hyperlipidemia with etophylline clofibrate: effects on lipoprotein-modifying enzymes, postprandial lipoprotein metabolism, and lipoprotein distribution and composition. Atherosclerosis 117, 253–261.
Friedewald WT, Levy RI, Fredrickson DS (1972). Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18, 499–502.
Graner M, Kahri J, Nakano T, Sarna SJ, Nieminen MS, Syvanne M et al. (2006). Impact of postprandial lipaemia on low-density lipoprotein (LDL) size and oxidized LDL in patients with coronary artery disease. Eur J Clin Invest 36, 764–770.
Hajer GR, Dallinga-Thie GM, van Vark-van der Zee LC, Visseren FL (2009). The effect of statin alone or in combination with ezetimibe on postprandial lipoprotein composition in obese metabolic syndrome patients. Atherosclerosis 202, 216–224.
Hiramatsu K, Arimori S (1988). Increased superoxide production by mononuclear cells of patients with hypertriglyceridemia and diabetes. Diabetes 37, 832–837.
Koba S, Tsunoda F, Hirano T, Iso Y, Suzuki H, Geshi E et al. (2005). Postprandial changes in LDL phenotypes in patients with myocardial infarction. Eur J Clin Invest 35, 171–179.
Lopez-Miranda J, Williams C, Lairon D (2007). Dietary, physiological, genetic and pathological influences on postprandial lipid metabolism. Br J Nutr 98, 458–473.
Markwell MAK, Haas SM, Tolbert NE, Bieber LL (1981). Protein determination in membrane and lipoprotein samples: manual and automated procedures. Methods Enzymol 72, 296–303.
Mora S, Rifai N, Buring JE, Ridker PM (2008). Fasting compared with nonfasting lipids and apolipoproteins for predicting incident cardiovascular events. Circulation 118, 993–1001.
Navab M, Hama SY, Hough GP, Subbanagounder G, Reddy ST, Fogelman AM (2001). A cell-free assay for detecting HDL that is dysfunctional in preventing the formation of or inactivating oxidized phospholipids. J Lipid Res 42, 1308–1317.
Nicholls SJ, Lundman P, Harmer JA, Cutri B, Griffiths KA, Rye KA et al. (2006). Consumption of saturated fat impairs the anti-inflammatory properties of high-density lipoproteins and endothelial function. J Am Coll Cardiol 48, 715–720.
Nordestgaard BG, Benn M, Schnohr P, Tybjaerg-Hansen A (2007). Nonfasting triglycerides and risk of myocardial infarction, ischemic heart disease, and death in men and women. JAMA 298, 299–308.
Noto D, Rizzo M, Barbagallo CM, Cefalu AB, Verde AL, Fayer F et al. (2006). Low-density lipoproteins generated during an oral fat load in mild hypertriglyceridemic and healthy subjects are smaller, denser, and have an increased low-density lipoprotein receptor binding affinity. Metabolism 55, 1308–1316.
O’Keefe JH, Bell DSH (2007). Postprandial hyperglycemia/hyperlipidemia (postprandial dysmetabolism) is a cardiovascular risk factor. Am J Cardiol 100, 899–904.
Patel S, Puranik R, Nakhla S, Lundman P, Stocker R, Wang XS et al. (2009). Acute hypertriglyceridaemia in humans increases the triglyceride content and decreases the anti-inflammatory capacity of high density lipoproteins. Atherosclerosis 204, 424–428.
Pronai L, Hiramatsu K, Saigusa Y, Nakazawa H (1991). Low superoxide scavenging activity associated with enhanced superoxide generation by monocytes from male hypertriglyceridemia with and without diabetes. Atherosclerosis 90, 39–47.
Scheffer PG, Bakker SJL, Heine RJ, Teerlink T (1997). Measurement of low-density lipoprotein particle size by high-performance gel-filtration chromatography. Clin Chem 43, 1904–1912.
Scheffer PG, Bos G, Volwater HG, Dekker JM, Heine RJ, Teerlink T (2003). Associations of LDL size with in vitro oxidizability and plasma levels of in vivo oxidized LDL in type 2 diabetic patients. Diabet Med 20, 563–567.
Scheffer PG, Teerlink T, Heine RJ (2005). Clinical significance of the physicochemical properties of LDL in type 2 diabetes. Diabetologia 48, 808–816.
Schindhelm RK, Alssema M, Diamant M, Teerlink T, Dekker JM, Kok A et al. (2008). Comparison of two consecutive fat-rich and carbohydrate-rich meals on postprandial myeloperoxidase response in women with and without type 2 diabetes mellitus. Metabolism 57, 262–267.
Tushuizen ME, Nieuwland R, Rustemeijer C, Hensgens BE, Sturk A, Heine RJ et al. (2007). Elevated endothelial microparticles following consecutive meals are associated with vascular edothelial dysfunction in type 2 diabetes. Diabetes Care 30, 728–730.
Ursini F, Sevanian A (2002). Postprandial oxidative stress. Biol Chem 383, 599–605.
Vakkilainen J, Mero N, Schweizer A, Foley JE, Taskinen MR (2002). Effects of nateglinide and glibenclamide on postprandial lipid and glucose metabolism in type 2 diabetes. Diabetes Metab Res Rev 18, 484–490.
Van Oostrom AJ, Sijmonsma TP, Verseyden C, Jansen EH, de Koning EJ, Rabelink TJ et al. (2003). Postprandial recruitment of neutrophils may contribute to endothelial dysfunction. J Lipid Res 44, 576–583.
Acknowledgements
This study was supported by a grant from the Dutch Diabetes Foundation (Grant number 2000.00.025). McDonald's, the Netherlands, is gratefully acknowledged for providing the test meals. We gratefully acknowledge Bert Volwater for technical support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Scheffer, P., Tushuizen, M., Vermue, H. et al. Effect of three consecutive meals on the physicochemical properties of HDL and LDL in individuals with the metabolic syndrome and patients with type 2 diabetes. Eur J Clin Nutr 65, 1242–1249 (2011). https://doi.org/10.1038/ejcn.2011.114
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2011.114
Keywords
This article is cited by
-
Consumption of a high-fat breakfast on consecutive days alters preclinical biomarkers for atherosclerosis
European Journal of Clinical Nutrition (2017)
-
Phenotypic flexibility as a measure of health: the optimal nutritional stress response test
Genes & Nutrition (2015)