Abstract
Perforin is a pore-forming protein engaged mainly in mediating target T cell death and is employed by cytotoxic T lymphocytes (CTLs) and natural killer cells. However, whether it also plays a role in conventional CD4+ T cell function remains unclear. Here we report that in perforin-deficient (PKO) mice, CD4+ T cells are hyperproliferative in response to T cell receptor (TCR) stimulation. This feature of hyperproliferation is accompanied by the enhancement both in cell division and in IL-2 secretion. It seems that the perforin deficiency does not influence T cell development in thymus spleen and lymph node. In vivo, perforin deficiency results in increased antigen-specific T cell proliferation and antibody production. Furthermore, PKO mice are more susceptible to experimental autoimmune uveitis. To address the molecular mechanism, we found that after TCR stimulation, CD4+ T cells from PKO mice display an increased intracellular calcium flux and subsequently enhance activation of transcription factor NFAT1. Our results indicate that perforin plays a negative role in regulating CD4+ T cell activation and immune response by affecting TCR-dependent Ca2+ signaling.
Similar content being viewed by others
Introduction
Antigenic stimulation of T lymphocytes by the T cells receptor (TCR) in combination with costimulatory molecules initiates the activation program. The activated tyrosine kinase, Lck, induced by TCR, can phosphorylate subunits of the TCR complex and the syk family kinase, ZAP-70. In turn, ZAP-70 phosphorylates tyrosine residues in the cytoplasmic portion of the transmembrane adaptor, LAT, which acts as docking sites for the assembly of a multimolecular signaling complex. These "signalosomes" trigger several downstream cascades 1, 2. Among those, calcium signaling plays critical and specific roles in T cell activation. A typical calcium response occurs in two distinct steps. Initially, activated phospholipase C-γ (PLC-γ) in the signalosomes can cleave phosphatidylinositol 4,5-bisphosphate (PIP2) to inositol 1,4,5-triphosphate (IP3) and diacylglycerol (DAG) 3. IP3 binds IP3 receptors on the endoplasmic reticulum (ER), which can drain intracellular stores of Ca2+ to the cytoplasm. Then the decrease in ER calcium triggers extracellular calcium influx by activating store-operated calcium (SOC) channels in the plasma membrane, thus leading to a sustained increase in intracellular calcium 4. The enhanced calcium signal activates the serine-threonine phosphatase calcineurin. NFAT proteins are then dephosphorylated, translocated to the nucleus and bind genes such as IL-2 to induce cell activation and proliferation 5.
Precise execution of the program is critical for proper function of the adaptive immune response. Positive and negative regulatory feedback loops influence the primary stimulation threshold and the persistence of signals in various phases of the response 6. Indeed, defects in negative regulatory molecules could lead to the accumulation of activated T lymphocytes and the development of autoimmune diseases in mice and humans 7, 8, 9.
Perforin is a pore-forming protein of approximately 67 kDa expressed mainly in activated cytotoxic T lymphocyte (CTL) and natural killer (NK) cells, and stored in cytoplasmic granules. Based on the membranolytic properties of perforin, it can help the delivery of granzymes to target cells to provoke target cell death upon formation of immune cell contacts. Studies in perforin-deficient (PKO) mice demonstrate that perforin has an important role in clearance of virus and elimination of tumor cells executed mainly by CD8+ T cells and NK cells 10. In humans, mutations in the perforin gene result in familial hemophagocytic lymphohistiocytosis (FHL) 11, 12, 13 caused by the inability of activated CTLs to clear antigen-presenting targets. In FHL patients, CD8+ T cells and macrophages become uncontrolled and expansive and release increased levels of pro-inflammatory cytokines (IFN-γ, TNF-α, and IL-12) into the blood. This ultimately leads to destruction of tissues and failure in infection control. The patients would die within a few months of the onset of symptoms if not treated appropriately. Extensive studies have revealed that perforin can down-regulate T cells-mediated immune responses in lupus 14 and Theiler's virus-induced demyelinating disease 15. In addition to its cytotoxic function in CD8+ T cells, these results suggest that perforin may play other roles in T cells function during different types of immune responses, and that it is more than just an effector molecule in the immune response 16.
As compared with its role in CD8+ T cells, the function of perforin in CD4+ T cells is rarely investigated. Recent studies demonstrate that human regulatory T cells can cause autologous target cell death through the perforin/granzyme pathway 17. However, the role of perforin in conventional CD4+ T cells function is not well understood. In the present study, we demonstrate that CD4+ T cells from PKO mice exhibit exaggerated responsiveness to TCR stimulation, such as hyperproliferation, accelerated cell division, and greater cytokine production. These results are consistent with the enhanced calcium signaling and NFAT1 nuclear translocation observed in PKO CD4+ T cells. Furthermore, PKO mice are shown to be more susceptible to experimental autoimmune uveitis (EAU). These observations suggest that perforin plays a crucial role in down-regulation of CD4+ T cells function and immune response through affecting calcium signaling.
Results
CD4+ T cells of PKO mice exhibit enhanced responses upon TCR activation
To investigate whether perforin plays a role in regulating CD4+ T cells activation, perforin expression was initially detected by western-blot analysis in CD4+ T cells stimulated with anti-CD3 antibody. The perforin expression was low but detectable at 72 h after activation (Figure 1A). In order to confirm the expression of perforin in CD4+ T cells, we performed confocal microscopy analysis as described in Materials and Methods. As shown in Figure 1B, we can detect perforin protein expression in activated CD4+ T cells by confocal microscopy. Subsequently, CD4+ T cells from WT and PKO mice were isolated and T cells proliferation was measured by thymidine incorporation. The data reveal that T cells from PKO mice displayed an enhanced proliferation in response to anti-CD3 (Figure 1C) or anti-CD3 plus CD28 stimulation (data not shown). T cells numbers in PKO mice were also increased following anti-CD3 stimulation (Figure 1D). However, proliferation induced by phorbol 12-myristate 13-acetate (PMA) and ionomycin, which bypass the proximal TCR signaling events and directly activate protein kinase C (PKC) and Ras GTPase, was similar (Figure 1E). This result suggests that the enhanced proliferation of PKO CD4+ T cells is due to a specific proximal TCR signaling event. In order to exclude the potential confounding influence of pre-activated or memory T cells, naïve CD4+CD62L+ T cells were isolated and analyzed. As shown in Figure 1F, CD4+CD62L+ T cells from PKO mice also displayed an enhanced proliferation upon anti-CD3 stimulation. Taken together, these results indicate that CD4+ T cells from PKO mice displayed a hyperproliferation phenotype upon TCR activation.
CD4+ T cells of PKO mice are hyperproliferative to TCR stimulation. (A) Perforin expression as stimulated by 1 μg/ml anti-CD3 in CD4+ T cells of WT mice underwent immunoblot analysis. (B) DIC image of perforin expression in WT and PKO CD4+ T cells. Localization of CD4 (red) and perforin (green) are shown. CD4+ T cells were purified from spleens of WT and PKO mice and cell proliferation response to different stimuli was measured at 48 h by [3H]thymidine incorporation. (C) CD4+ T cells were stimulated with anti-CD3. (D) CD4+ T cells were stimulated with anti-CD3 and cell numbers were determined on different days. (E) CD4+ T cells were stimulated with PMA plus ionomycin (P + I). (F) Naïve CD4+CD62L+ T cells were stimulated with anti-CD3. Data are representative of three independent experiments. *p < 0.05.
Cell division of CD4+ T cells is enhanced in PKO mice
In general, T cells proliferation is influenced mainly by cell division and apoptosis. To explore the potential mechanisms of the hyperproliferation of PKO CD4+ T cells, WT and PKO CD4+ T cells were labeled with CFSE, and T cells division was analyzed by flow cytometry. As shown in Figure 2A, after 24 h of activation, T cells have not divided yet, and there is no difference of cell division between these two groups. However, upon 68 h of TCR activation, T cells from PKO mice divided more than those from WT mice (73.3% vs 54.5%). These data indicate that cell division was increased in PKO mice. The spontaneous apoptosis remained comparable between WT- and PKO-T cells upon anti-CD3 stimulation at all tested time points (Figure 2B). It is remarkable that there was no significant difference between the two groups in activation-induced cell death (AICD) for activated T cells (Figure 2C). These data suggest that the hyperproliferation of PKO T cells is related to enhanced cell division.
PKO CD4+ T cells have an enhanced cell division but normal cell apoptosis. (A) Purified CD4+ T cells of WT and PKO mice were labeled with 10 μM CFSE and stimulated with anti-CD3 for 24 or 68 h, and cell division was analyzed using flow cytometry. The numbers present the percentage of divided CD4+ T cells in total CD4+ T cells. (B) CD4+ T cells of WT and PKO mice were cultured for different time periods and double-stained with Annexin V and 7-AAD to determine the percentages of apoptotic cells. (C) CD4+ T cells were initially stimulated for 48 h, and the cells harvested and restimulated with anti-CD3 for 16 h. AICD was analyzed. Data are representative of three independent experiments.
T cells development is normal in PKO mice
Since cell division rate was increased in PKO mice, we wondered whether T cells development in PKO mice was abnormal. However, experimental results showed that the distributions of CD4+ and CD8+ cells were similar in thymus, spleen, and lymph nodes between WT and PKO mice (Figure 3A). Since memory T cells are more easily activated than naïve T cells, a different ratio of memory T cells to naïve T cells may also contribute to the hyperproliferation phenotype of PKO T cells. To check this possibility, we analyzed CD62L+ and CD44+ expression by flow cytometry. The data indicated that there was no difference in the percentages of CD62L−CD44+ (memory/activated) and CD62L+CD44− (naïve) cells between PKO and WT mice (Figure 3B). These results exclude the possibility that hyperproliferation was due to altered memory/activated T cells ratio in PKO mice.
T-cell development and TCR down-modulation in PKO mice are normal. (A) Single-cell suspensions of the thymus, spleen, and peripheral lymph nodes isolated from WT and PKO mice were stained with anti-CD4 and anti-CD8. (B) Stained with CD44 and CD62L in CD4+ T cells of spleen and lymph nodes isolated from WT and PKO mice. (C) Splenocytes of WT (upper) and PKO (lower) mice were stained with anti-CD4 and anti-TCR, stimulated with anti-CD3 (bold line) for 6 h, and analyzed for TCR surface expression. TCR expression level on unstimulated cells is shown as control (thin line). (D) The kinetics of TCR down-modulation on WT and PKO CD4+ T cells were measured after stimulation with anti-CD3. The results are representative of three independent experiments.
Normal TCR down-modulation in PKO T cells
The induction of T cells activation is directly correlated with the number of TCR molecules on the cell surface and its subsequent down-modulation. T cells hyperproliferation has recently been linked to impaired CD3/TCR down-modulation. Therefore we studied TCR down-modulation in PKO and WT CD4+ T cells upon CD3-TCR engagement. Without TCR stimulation, PKO and WT CD4+ T cells expressed comparable levels of surface TCR (Figure 3C). Moreover, the kinetic change in down-modulation of TCR was quite similar between PKO and WT T cells following CD3-TCR stimulation (Figure 3D), suggesting that TCR down-modulation in PKO mice is normal.
Cytokine production is increased in PKO T cells
IL-2 production is a hallmark of T cells activation. Early IL-2 production can render T cells to proliferate and divide more efficiently and faster. Therefore, we next determined the effect of the loss of perforin on IL-2 synthesis. Similar to the T cells proliferative response, the production of IL-2 was enhanced in PKO T cells with anti-CD3 stimulation at a very early time point (24 h) (Figure 4A), while the expression of CD25 (IL-2R) on T cells appeared unaltered between these two groups (Figure 4B). To assess whether the different abilities of T cells proliferation is due to the different amounts of IL-2 production in PKO and WT cells, two experiments were performed. First, we added exogenous IL-2 to the cultured WT and PKO CD4+ T cells activated with anti-CD3 and measured T cells proliferation. The results showed that the murine recombinant IL-2 was able to enhance T cells proliferation and to diminish the difference of proliferation between PKO and WT CD4+ T cells (Figure 4C). Second, anti-IL-2 antibody was used to neutralize the activity of IL-2. This treatment diminished T cells proliferation and led to equalized proliferation between WT and PKO T cell groups (Figure 4D). Also, production of other cytokines, such as IFN-γ and IL-4, was enhanced in PKO CD4+ T cells (Supplementary information, Figure S1), suggesting that there is no Th1/Th2 bias in PKO mice. These results demonstrate that perforin plays a critical role in negative regulation of T cells proliferation through modulation of IL-2 production.
IL-2 secretion and its effect on CD4+ T-cell proliferation in PKO mice. (A) IL-2 production in supernatants of T cells from WT and PKO mice activated by 1 μg/ml anti-CD3. (B) CD25 surface expression of non-activated (upper panel) or activated (lower panel) CD4+ T cells by anti-CD3 (1 μg/ml) from WT or PKO mice was determined as described above. CD4+ T cells from WT or PKO mice were stimulated with 1 μg/ml of anti-CD3 antibody in the absence or in the presence of increasing concentrations of recombinant murine IL-2 (rmIL-2) (C) or anti-IL-2 (D) for 48 h and analyzed by [3H]thymidine incorporation. Data are representative of three (A) or two (B–D) independent experiments. *p < 0.05.
Increased Ag-specific T cells activation in vivo in PKO mice
To examine whether negative regulation of CD4+ T cells by perforin has any important immune function in vivo, C57BL/6 WT and PKO mice were immunized with KLH protein emulsified in complete Freund's adjuvant (CFA). Eight days after immunization, these mice were killed and KLH-specific T cells proliferation, IL-2 production, and anti-KLH IgM and IgG antibodies were measured. The results showed that perforin deficiency led to greater anti-KLH IgM and IgG production (Figure 5A), indicating that a stronger humoral immune response was generated in PKO mice in vivo. The spleen cells from immunized mice were also collected and restimulated in vitro with KLH. The data showed that cells from PKO mice consistently exhibited greater KLH-specific-proliferation and IL-2 production than those of WT mice (Figure 5B and 5C), suggesting that stronger T cells priming occurred in vivo in PKO mice. In order to rule out the potential confounding effects of other cell types, such as CD8+ T cells and B cells, in PKO mice, and further confirm the role of CD4+ T cells in this process, Rag1−/− mice were transferred with naïve CD4+CD62L+ T cells from WT and PKO mice and then immunized with KLH protein. Eight days after immunization, the percentage of CD4+ T cells in the spleen of Rag1−/− mice transferred with PKO CD4+ T cells was almost twice that of the mice transferred with WT CD4+ T cells (Figure 5D). Similarly, spleen cells from Rag1−/− mice transferred with PKO CD4+ T cells exhibited an enhanced proliferation compared with that from Rag1−/− mice transferred with WT CD4+ T cells when stimulated with KLH in vitro (Figure 5E). These data indicate that CD4+CD62L+ T cells from PKO mice did contribute to mounting a stronger immune response.
Perforin down-regulates T-cell-dependent immune responses and EAU disease in vivo. Mice (n=5) were immunized with KLH for 8 days and then killed. (A) Anti-KLH serum IgM and IgG (total) was measured individually by ELISA and averaged for each group. Spleen cells from each immunized mouse were restimulated in vitro with or without KLH to analyze the T-cell proliferation (B) and IL-2 production (C). Rag−/− mice were transferred with naïve CD4+ T cells from WT and PKO mice and immunized with KLH. On day 8, the percentage of CD4+ T cells in spleen (D) and the KLH-specific proliferation of spleen cells (E) were analyzed (five mice of each group). WT and PKO mice were immunized with IRBP to induce EAU. (F)The scoring of EAU disease in these mice was analyzed as described in Materials and Methods. EAU scores at all points differ significantly between WT and PKO mice. Each symbol represents the pathology score for one mouse (average of both eyes). The average EAU score of each group is denoted by the horizontal bar. (G) Proliferation of splenic T cells from IRBP immunized WT and PKO mice, restimulated with different concentrations of IRBP, and analyzed using [3H]thymidine incorporation. (H) The production of interferon-γ and IL-2 was measured by ELISA in splenocytes restimulated with IRBP in vitro for 48 and 24 h.
To assess the potential regulatory role of perforin in T cells-mediated autoimmune diseases, C57BL/6 WT and PKO mice were immunized with IRBP protein as described previously 18, 19 and EAU disease was induced. As shown in Figure 5F, the incidence and mean severity of EAU were significantly higher in PKO mice than in WT mice. We also collected spleen cells from immunized mice and restimulated them in vitro with IRBP. The cells from PKO mice exhibited greater proliferation (Figure 5G) and cytokine production (IFN-γ and IL-2) than those from WT control mice (Figure 5H). Taken together, our data suggest that perforin negatively regulates T cells activation and that the deficiency of perforin in mice results in an enhanced susceptibility to autoimmune diseases, such as EAU.
Enhanced TCR-dependent Ca2+ signaling in PKO mice
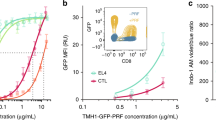
The enhanced T cells proliferation in PKO mice indicates that T cells signaling may be augmented in the absence of perforin. To probe the potential mechanism, firstly, the level of total tyrosine phosphorylation, which reflects the major proximal TCR event after stimulation, was examined. The results showed no significant difference between WT and PKO CD4+ T cells groups (Figure 6A). Because MAPK activation is essential in T cells proliferation, we then investigated whether perforin could regulate T cells proliferation and function through MAPK signaling. We found that TCR-induced activation of p38, Erk, and Jnk was also unaffected in naïve PKO T cells (data not shown). Intriguingly, TCR-induced intracellular Ca2+ influx was prominently increased in PKO CD4+ T cells after streptavidin crosslinking (Figure 6B). These results suggest that perforin could regulate the TCR-dependent calcium-signaling pathway. Because phosphorylation of PLC-γ1 induced by TCR stimulation can up-regulate calcium signaling, we then investigated whether deficiency of perforin could enhance the activation of PLC-γ1. The results show that anti-CD3-induced PLC-γ1 phosphorylation was comparable between these two groups (Figure 6C). It has been reported that increased free intracellular calcium concentration can lead to NFAT dephosphorylation and nuclear translocation, which in turn promotes IL-2 production and T cells activation 5. To assess NFAT1 expression and localization, CD4+ T cells from WT and PKO mice were stimulated with plate-bound anti-CD3, and nuclear and cytoplasmic fractions were analyzed by immunoblot assay. Consistent with the increase in calcium flux, the dephosphorylated form of NFAT1 was readily detected in the nuclear fraction of PKO CD4+ T cells, but not in WT CD4+ T cells, after 30 min of TCR stimulation. Furthermore, at 16 h after stimulation, more dephosphorylated NFAT1 was detected in the nuclear fraction of PKO CD4+ T cells. In the cytosol, NFAT1 appeared mainly in its phosphorylated forms in WT CD4+ T cells before stimulation, but dephosphorylated NFAT1 could be detected in PKO CD4+ T cells even before stimulation. At 0.5 h after stimulation, more dephosphorylated NFAT1 was detected in PKO CD4+ T cells, but the signal was relatively weaker in WT mice. It became obvious that dephosphorylated NFAT1 was decreased at 16 h after stimulation in PKO CD4+ T cells (Figure 6D). The results indicate that NFAT1 was dephosphorylated and then translocated into the nucleus in PKO CD4+ T cells after stimulation. Using gel shift assay, similar results were observed. NFAT DNA binding was significantly increased in PKO CD4+ T cells (Figure 6E). To test whether the enhanced proliferation in PKO CD4+ T cells is induced mainly by the increased calcium influx, we treated T cells with the Ca2+ ionophore ionomycin (which mediates high calcium flux through the plasma membrane and increases intracellular calcium concentration). The results showed that in the presence of ionomycin, TCR stimulation resulted in a higher T cells proliferation in WT mice, and that the difference in proliferation between PKO and WT T cells was eliminated (Figure 6F).
Enhanced calcium signaling in PKO mice. (A) Immunoblot of lysates of purified CD4+ T cells stimulated for different time periods with biotin-anti-CD3 (1 μg/ml) and streptavidin, analyzed with a phosphotyrosine-specific antibody (4G10). (B) CD4+ T cells were labeled with calcium indicator Fluo-3, stimulated with biotin-conjugated anti-CD3 (1 μg/ml), and the calcium flux analyzed using flow cytometry. (C) Immunoprecipitation (IP) of lysates of anti-CD3-stimulated (1 μg/ml), purified CD4+ T cells with anti-PLC-γ1, followed by immunoblot with anti-phosphotyrosine; the blot was then reprobed with anti-PLC-γ1. (D) CD4+ T cells were stimulated with anti-CD3 (1 μg/ml) for the indicated times. Nuclear localization of NFAT1 was examined by immunoblot analysis of nuclear or cytoplasmic extracts. β-actin was used as internal control. (E) DNA binding of NFAT was examined in nuclear extracts from WT and PKO CD4+ T cells. (F) WT and PKO CD4+ T cells were stimulated with anti-CD3 (1 μg/ml) with or without ionomycin (62.5 pg/ml) and the cell proliferation determined. *p < 0.05.
Discussion
Perforin is a powerful effector in induction of target cell death. It is expressed mainly in CTL and NK cells and has recently been shown to be related to immune regulation. Although perforin is known to regulate CD8+ T cells homeostasis 20, 21, the role of perforin in conventional CD4+ T cells function has not been well investigated. In this study, we found that loss of perforin leads to enhanced CD4+ T cells activation and immune function, and that the calcium-signaling pathway is involved in this process. These observations correlate with an elevated production of IL-2, a hallmark of T cells activation. Interestingly, loss of perforin does not affect the expression of CD25 (IL-2R), and perforin has no effect on T cells development. We also found that CD4+ T cells apoptosis and TCR down-modulation remain normal. It is likely that perforin is a negative modulator of the signaling pathways that control IL-2 synthesis and CD4+ T cells activation upon TCR stimulation.
T cells activation is associated with changes in calcium flux 22. Previous studies demonstrated that perforin has a tight relationship with Ca2+. Firstly, perforin contains Ca2+ binding sites in the C2 domain and its cytotoxic activity is regulated by Ca2+ 23. On the other hand, perforin can form calcium channels and lead to accumulation of Ca2+ in target cells 24. However, whether perforin can regulate calcium function in primary CD4+ T cells in a cell-intrinsic manner remains unclear. The proximal TCR signaling includes early tyrosine phosphorylation, a subsequent calcium influx, and MAPK activation. Here, we demonstrate that calcium flux is enhanced in PKO CD4+ T cells upon TCR stimulation. Although the Ca2+ elevation is not sufficient to activate T cells, the increased calcium flux in PKO CD4+ T cells could lead to a cascade of signaling transduction to ultimately enhance IL-2 production and cell proliferation.
In T cells, an increase in Ca2+ results in dephosphorylation and translocation of NFAT to the nucleus, which then induces IL-2 production 25. The NFAT subcellular localization is regulated by nuclear import and nuclear export 26. TCR stimulation of PKO CD4+ T cells results in more accumulation of dephosphorylated forms of NFAT1 in the nucleus, suggesting that the strength of TCR signaling is enhanced in PKO CD4+ T cells. These results are consistent with enhanced calcium influx. When ionomycin is added to the culture system, WT CD4+ T cells proliferation is enhanced and the difference between WT- and PKO-CD4+ T cells is eliminated. These results suggest that the enhanced TCR-dependent Ca2+ signaling, which is induced by perforin deficiency, contributes to hyperproliferation in PKO CD4+ T cells.
Calreticulin is a major Ca2+ binding protein found in the lumen of the ER 27 and is involved in several processes that comprise cellular Ca2+ homeostasis, including Ca2+ storage in the ER 28, Ca2+ release from the ER 28, 29, and activation of store-operated Ca2+ influx 30, 31, 32, 33. A deficiency of calreticulin in T cells can lead to hyperproliferation and enhanced IL-2 production through its effect on the intracellular calcium flux 34, an effect similar to that seen in PKO mice. Previous data suggest that perforin can colocalize and interact with calreticulin in CTLs 35, and our data demonstrate that perforin can also interact with calreticulin in primary CD4+ T cells (Supplementary information, Figure S2). Therefore, it is possible that perforin may regulate the Ca2+ dynamics in the ER through calreticulin. However, the exact mechanism remains to be elucidated.
Previous reports demonstrate that perforin can down-regulate some immune responses 13, 14, 15. The main mechanism for this effect is believed to be that CTLs can rapidly eliminate dendritic cells (DC) loaded with specific antigen, in a perforin-dependent manner, to restrict the immune response. Compared with control mice, PKO mice exhibit a progressive increase in the number of antigen-specific CD8+ T cells after repeated immunizations with DC 36, 37. Also, in perforin mutant FHL patients, CD8+ T cells are accumulated in the peripheral tissues 11, 12, 13. The second possible mechanism might be that perforin acts in a cell-intrinsic manner to regulate CTL numbers by limiting proliferation or by contributing to the AICD of CTL. Another possibility is that perforin may limit the proinflammatory activity of some granule components such as granzyme A 38. Recently, the role of perforin in the immune response has been related to regulatory T cells in human. However, our in vivo data (Figure 5) suggest that perforin has a direct role in conventional CD4+ T cells in the regulation of immune response. The enhanced proliferation of CD4+ T cells in PKO mice in vivo results in a higher antibody production and in exacerbated autoimmune disease.
Taken together, the present data demonstrate that perforin functions as a negative regulator of CD4+ T cells proliferation and IL-2 production. It also dampens T cells-mediated immunity and disease progression in vivo and its mechanism is related to the regulation of calcium flux in activated T cells. These results demonstrate the importance and complexity of perforin in regulating the immune system, and may help to further our understanding of the function of perforin in human disease.
Materials and methods
Materials
An Annexin-V-FLUOS staining kit was purchased from Roche (Mannheim, Germany). T cells isolation kits were obtained from Miltenyi Biotech (Auburn, CA). A BCA protein assay reagent kit and a Light Shift Chemiluminescent EMSA kit were purchased from Pierce (Rockford, IL). Purified Bordetella pertussis toxin (PTX) was purchased from Sigma Chemical (St Louis, MO) and CFA was obtained from Difco (Detroit, MI). IRBP was isolated from bovine retinas using Con A-Sepharose affinity chromatography and fast-performance liquid chromatography as described 39. IRBP preparations were stored at −70°C until used. Anti-perforin (CB5.4) from Alexis Biochemicals, anti-phosphotyrosine (4G10) from Upstate Biotechnology, anti-PLC-γ1 (1249) from Santa Cruz Biotechnology, anti-NFAT1 from ABR affinity BioReagents, anti-calreticulin from Abcam, and anti-phosphorylated p38 (p-P38), anti-phosphorylated Erk (p-Erk), anti-phosphorylated JNK (p-JNK) from Cell Signaling were also used.
Mice
Wild-type C57BL/6 mice and perforin−/− (PKO) mice with B6 background were obtained from the Jackson Laboratory (Bar Harbor, ME). Rag1−/− mice with B6 background were gifts from XL Liu. Animals were kept in a specific pathogen-free facility at the Chinese Academy of Sciences and only female mice (6–10 weeks) were used. Animal care and use were in compliance with institutional guidelines.
CD4+ T cells isolation
Spleens were removed from 4- to 8-week old mice. Red blood cells were lysed with an NH4Cl buffer. Afterwards, CD4+ T cells were negatively isolated using commercial kits (Miltenyi Biotec) according to the manufacturer's instructions. Naïve CD4+ CD62L+ T cells were sorted by FACS.
CD4+ T cells proliferation and apoptosis assay
Purified CD4+ T cells were cultured at 0.5-1×106/ml in 200 μl of medium per well and were stimulated in 96-well plates pre-coated with anti-CD3 antibody (clone 145-2C11). For co-stimulation of T cells, soluble anti-CD28 (clone 37.51) was also added at 1 μg/ml. Proliferation was assessed by the incorporation of [3H]thymidine added at 1 μCi/well during the last 12h of culture in triplicate wells. Cells were collected using a cell harvester and [3H]thymidine was quantified by scintillation counting.
Spontaneous apoptosis was determined using annexin V and PI staining at various time points. AICD was also determined by stimulating activated T cells with 1 μg/ml anti-CD3 antibody for 16h.
Flow cytometry
Lymph node, spleen and thymus cell suspensions were collected and erythrocytes were lysed. Cells were counted and stained with fluorochrome-conjugated antibodies specific for CD3, CD4, CD8, CD25, CD44, CD62L, CD69, and TCR (all from BD Pharmingen).
Cell division analysis
Purified CD4+ T cells were labeled with 10μM CSFE (Molecular Probes, Eugene, OR) in PBS with 0.1% BSA for 15 min at 37 °C. Cells were washed in complete RPMI 1640 and stimulated in 24-well plates (2×105 cells/well) coated with anti-CD3 antibody (1 μg/ml) and cell division was analyzed using flow cytometry.
TCR down-modulation
For the TCR down-modulation assay, spleen cells isolated from WT and PKO mice were incubated with 1 μg/ml of plate-bound anti-CD3 at 37 °C for various times. Collected cells were surface-stained with PE-conjugated anti-TCR (H57-597) and FITC-conjugated anti-CD4 (RM4-5) and analyzed on a FACS can flow cytometer. The percentage of TCR-CD3 down-modulation was determined using the formula Percentage of TCR down-modulation (at time t) =100 × [mean fluorescence intensity (MFI) of unstimulated T cells (at time t) - MFI of stimulated T cells (at time t) ]/MFI of unstimulated T cells (at t = 0) as described.
KLH immunization
Mice were immunized subcutaneously in both thighs with 50 μg KLH protein (Sigma Chemical Co.) emulsified in CFA. On day 8, the immunized mice were killed and analyzed for their immune responses. Splenocytes were restimulated with KLH to measure T cells proliferation and IL-2 expression. Anti-KLH IgM and anti-IgG antibodies in the serum of immunized mice were measured using ELISA.
Adoptive transfer
Naïve CD4+CD62L+ T cells were purified from WT and PKO mice by FACS. 1×107 CD4+ T cells were injected into Rag1−/− mice by the tail vein. Then mice were immunized subcutaneously with KLH protein. On day 8, the immunized mice were analyzed.
EAU induction and analysis
EAU was induced in WT and PKO mice with IRBP in CFA and PTX as described previously 18. Tissues (eyes and lymphoid organs) were collected on day 21 after immunization. Freshly enucleated eyes were fixed for 1 h in 4% phosphate-buffered glutaraldehyde and transferred into 10% phosphate-buffered formaldehyde until processing. Fixed and dehydrated tissue was embedded in methacrylate, and 4-6-μm sections, cut through the pupillary-optic nerve plane, were stained by standard H&E. The severity of EAU was scored on a scale of 0-4 in half-point increments, according to a semiquantitative system described previously 40. Splenocytes were restimulated with IRBP to measure T cells proliferation and cytokine expression.
Calcium flux
Splenocytes were labeled with 5 μM Fluo-3 in PBS containing 0.02% Pluronic F-127 (Molecular Probe) for 45 min at 37 °C. Cells were then washed twice, allowed to 'rest' for 20 min in the dark and subsequently incubated for 25 min on ice with 10μg/ml of biotin-conjugated anti-CD3 and PerCP-conjugated CD4 (Pharmingen). Labeled cells were washed, resuspended with prewarmed streptavidin, and analyzed by flow cytometry.
Electromobility shift assay
CD4+ T cells were stimulated with anti-CD3 for various times and harvested. Fractions of cytoplasmic and nuclear proteins were extracted as described previously 41. Oligonucleotides used as probe or competitor in EMSA assays were synthesized as follows: NFAT consensus, 5′-TCG AGC CCA AAG AGG AAA ATT TGT TTC ATG-3′, labeled or unlabeled at the 3′ end with biotin; NFAT consensus mutant, 5′-TCG AGC CCA AAG AGG ACC CTT TGT TTC ATG-3′. The altered nucleotides are underlined. The gel shift assay was performed using the LightShift Chemiluminescent electrophoretic mobility shift analysis kit (Pierce), following the manufacturer's instructions.
Immunoprecipitation and immunoblotting
Cell lysis, immunoprecipitation, and immunoblotting were performed as described previously 42.
Retroviral transduction
The full-length perforin cDNA was subcloned into a bicistronic retroviral vector pMSCV-internal ribosome entry site (IRES)/green fluorescence protein (GFP). Retrovirus preparation and cell infection were described previously 43.
Immunofluorescence confocal microscopy
Primary CD4+ T cells were transferred onto slides coated with L-lysine, fixed with 4% paraformaldehyde, and permeabilized with 0.1% Triton X-100 in PBS.
For detection of perforin in CD4+ T cells, cells were stained with PE-anti-CD4 and rat-anti-perforin. FITC-goat-anti-rat IgG secondary antibody was used to visualize the primary antibody. For detection of perforin and calreticulin, cells were stained with rat-anti-perforin and rabbit-anti-calreticulin, and then visualized with Cy5-goat-anti-rat and Cy3-goat-anti-rabbit secondary antibodies. Fluorescent images were captured with a Leica TCS SP2 laser confocal microscope.
Statistical analyses and reproducibility
Experiments were repeated at least twice, and usually three or more times. Figures show data compiled from several experiments, or from a representative experiment, as specified. Results represent the mean ± SD where applicable. Statistical analyses for parametric data were performed using the independent t-test. For non-parametric data (EAU scores) analyses were performed using the Snedecor and Cochran's test for linear trends in proportions.
( Supplementary information is linked to the online version of the paper on the Cell Research website.)
References
Huang Y, Wange RL . T cell receptor signaling: beyond complex complexes. J Biol Chem 2004; 279:28827–28830.
Inngjerdingen M, Torgersen KM, Maghazachi AA . Lck is required for stromal cell-derived factor 1 alpha (CXCL12)-induced lymphoid cell chemotaxis. Blood 2002; 99:4318–4325.
Imboden JB, Stobo JD . Transmembrane signalling by the T cell antigen receptor. Perturbation of the T3-antigen receptor complex generates inositol phosphates and releases calcium ions from intracellular stores. J Exp Med 1985; 161:446–456.
Hoth M, Penner R . Depletion of intracellular calcium stores activates a calcium current in mast cells. Nature 1992; 355:353–356.
Tomida T, Hirose K, Takizawa A, Shibasaki F, Iino M . NFAT functions as a working memory of Ca2+ signals in decoding Ca2+ oscillation. EMBO J 2003; 22:3825–3832.
Veillette A, Latour S, Davidson D . Negative regulation of immunoreceptor signaling. Annu Rev Immunol 2002; 20:669–707.
Greenwald RJ, Freeman GJ, Sharpe AH . The B7 family revisited. Annu Rev Immunol 2005; 23:515–548.
Lin L, Spoor MS, Gerth AJ, Brody SL, Peng SL . Modulation of Th1 activation and inflammation by the NF-kappaB repressor Foxj1. Science 2004; 303:1017–1020.
Shui JW, Boomer JS, Han J, et al. Hematopoietic progenitor kinase 1 negatively regulates T cell receptor signaling and T cell-mediated immune responses. Nat Immunol 2007; 8:84–91.
Kagi D, Ledermann B, Burki K, et al. Cytotoxicity mediated by T cells and natural killer cells is greatly impaired in perforin-deficient mice. Nature 1994; 369:31–37.
Feldmann J, Menasche G, Callebaut I, et al. Severe and progressive encephalitis as a presenting manifestation of a novel missense perforin mutation and impaired cytolytic activity. Blood 2005; 105:2658–2663.
Katano H, Cohen JI . Perforin and lymphohistiocytic proliferative disorders. Br J Haematol 2005; 128:739–750.
Stepp SE, Dufourcq-Lagelouse R, Le Deist F, et al. Perforin gene defects in familial hemophagocytic lymphohistiocytosis. Science 1999; 286:1957–1959.
Peng SL, Moslehi J, Robert ME, Craft J . Perforin protects against autoimmunity in lupus-prone mice. J Immunol 1998; 160:652–660.
Palma JP, Lee HG, Mohindru M, et al. Enhanced susceptibility to Theiler's virus-induced demyelinating disease in perforin-deficient mice. J Neuroimmunol 2001; 116:125–135.
Stepp SE, Mathew PA, Bennett M, de Saint Basile G, Kumar V . Perforin: more than just an effector molecule. Immunol Today 2000; 21:254–256.
Grossman WJ, Verbsky JW, Barchet W, et al. Human T regulatory cells can use the perforin pathway to cause autologous target cell death. Immunity 2004; 21:589–601.
Hou W, Wu Y, Sun S, et al. Pertussis toxin enhances Th1 responses by stimulation of dendritic cells. J Immunol 2003; 170:1728–1736.
Wu X, Hou W, Sun S, et al. Novel function of IFN-gamma: negative regulation of dendritic cell migration and T cell priming. J Immunol 2006; 177:934–943.
Badovinac VP, Tvinnereim AR, Harty JT . Regulation of antigen-specific CD8+ T cell homeostasis by perforin and interferon-gamma. Science 2000; 290:1354–1358.
Kagi D, Odermatt B, Mak TW . Homeostatic regulation of CD8+ T cells by perforin. Eur J Immunol 1999; 29:3262–3272.
Tsien RY, Pozzan T, Rink TJ . T cells mitogens cause early changes in cytoplasmic free Ca2+ and membrane potential in lymphocytes. Nature 1982; 295:68–71.
Liu CC, Walsh CM, Young JD . Perforin: structure and function. Immunol Today 1995; 16:194–201.
Binah O, Liu CC, Young JD, Berke G . Channel formation and [Ca2+]i accumulation induced by perforin N-terminus peptides: comparison with purified perforin and whole lytic granules. Biochem Biophys Res Commun 1997; 240:647–650.
Crabtree GR, Olson EN . NFAT signaling: choreographing the social lives of cells. Cell 2002; 109 Suppl:S67–S79.
Neilson J, Stankunas K, Crabtree GR . Monitoring the duration of antigen-receptor occupancy by calcineurin/glycogen-synthase-kinase-3 control of NFAT nuclear shuttling. Curr Opin Immunol 2001; 13:346–350.
Michalak M, Corbett EF, Mesaeli N, Nakamura K, Opas M . Calreticulin: one protein, one gene, many functions. Biochem J 1999; 344 Part 2:281–292.
Nakamura K, Zuppini A, Arnaudeau S et al. Functional specialization of calreticulin domains. J Cell Biol 2001; 154:961–972.
Mesaeli N, Nakamura K, Zvaritch E, et al. Calreticulin is essential for cardiac development. J Cell Biol 1999; 144:857–868.
Arnaudeau S, Frieden M, Nakamura K, et al. Calreticulin differentially modulates calcium uptake and release in the endoplasmic reticulum and mitochondria. J Biol Chem 2002; 277:46696–46705.
Bastianutto C, Clementi E, Codazzi F, et al. Overexpression of calreticulin increases the Ca2+ capacity of rapidly exchanging Ca2+ stores and reveals aspects of their lumenal microenvironment and function. J Cell Biol 1995; 130:847–855.
Fasolato C, Pizzo P, Pozzan T . Delayed activation of the store-operated calcium current induced by calreticulin overexpression in RBL-1 cells. Mol Biol Cell 1998; 9:1513–1522.
Xu W, Longo FJ, Wintermantel MR, et al. Calreticulin modulates capacitative Ca2+ influx by controlling the extent of inositol 1,4,5-trisphosphate-induced Ca2+ store depletion. J Biol Chem 2000; 275:36676–36682.
Porcellini S, Traggiai E, Schenk U, et al. Regulation of peripheral T cell activation by calreticulin. J Exp Med 2006; 203:461–471.
Andrin C, Pinkoski MJ, Burns K, et al. Interaction between a Ca2+-binding protein calreticulin and perforin, a component of the cytotoxic T cells granules. Biochemistry 1998; 37:10386–10394.
Hermans IF, Ritchie DS, Yang J, Roberts JM, Ronchese F . CD8+ T cell-dependent elimination of dendritic cells in vivo limits the induction of antitumor immunity. J Immunol 2000; 164:3095–3101.
Yang J, Huck SP, McHugh RS, Hermans IF, Ronchese F . Perforin-dependent elimination of dendritic cells regulates the expansion of antigen-specific CD8+ T cells in vivo. Proc Natl Acad Sci USA 2006; 103:147–152.
Sower LE, Klimpel GR, Hanna W, Froelich CJ . Extracellular activities of human granzymes. I. Granzyme A induces IL6 and IL8 production in fibroblast and epithelial cell lines. Cell Immunol 1996; 171:159–163.
Pepperberg DR, Okajima TL, Wiggert B, et al. Interphotoreceptor retinoid-binding protein (IRBP). Molecular biology and physiological role in the visual cycle of rhodopsin. Mol Neurobiol 1993; 7:61–85.
Chan CC, Caspi RR, Ni M, et al. Pathology of experimental autoimmune uveoretinitis in mice. J Autoimmun 1990; 3:247–255.
Huang C, Bi E, Hu Y, et al. A novel NF-kappaB binding site controls human granzyme B gene transcription. J Immunol 2006; 176:4173–4181.
Shi M, Deng W, Bi E, et al. TRIM30 alpha negatively regulates TLR-mediated NF-kappa B activation by targeting TAB2 and TAB3 for degradation. Nat Immunol 2008; 9:369–377.
Lin Y, Tang YJ, Zhong HL, et al. Cyclin G associated kinase interacts with interleukin 12 receptor beta2 and suppresses interleukin 12 induced IFN-gamma production. FEBS Lett 2007; 581:5151–5157.
Acknowledgements
We thank Drs Hua Gu (Columbia University, USA), Weiguo Zhang (Duke University Medical Center, USA), and Youhai H Chen (University of Pennsylvania, USA) for reviewing the manuscript and for suggestions, and Dr Ilia Voskoboinik (Peter MacCallum Cancer Centre, Australia) for providing the mouse perforin cDNA in pKS(+) Bluescript. Rag1−/− mice were gifts from Xiaolong Liu (Shanghai Institutes for Biological Sciences, China). This work was supported by grants from the National Natural Science Foundation of China (30325018, 30530700, 30623003, and 30421005) and CAS project (KSCX1-YW-R-43), grants from the National Key Project 973 (2006CB504300 and 2007CB512404), grants from the Technology Commission of Shanghai Municipality (04DZ14902, 04DZ19108, 06DZ22032, 04DZ19112, 07XD14033, and 07DZ22916), 863 key project (2006AA02A247), and a grant from the E-institutes of Shanghai Universities Immunology Division.
Author information
Authors and Affiliations
Corresponding author
Supplementary information
Rights and permissions
About this article
Cite this article
Bi, E., Huang, C., Hu, Y. et al. Novel function of perforin in negatively regulating CD4+ T cell activation by affecting calcium signaling. Cell Res 19, 816–827 (2009). https://doi.org/10.1038/cr.2009.32
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cr.2009.32