Abstract
Background:
Although patients with cancer are often accompanied by a relative during breaking bad news (BBN) consultations, little is known regarding the efficacy of training programmes designed to teach residents the communication skills needed to break bad news in a triadic consultation.
Methods:
Residents were randomly assigned to a 40-h dyadic and triadic communication skills training programme (n=48) or a waiting list (n=47). A simulated BBN triadic consultation was audiotaped at baseline, and after training for the training group, and 8 months after baseline for the waiting list group. Transcripts were analysed using content analysis software (LaComm). A coder determined the moment of bad news delivery and the relative’s first turn of speech regarding the bad news. A generalised estimating equation was used to evaluate residents’ communication skills, BBN timing, and the relative’s inclusion in the consultation.
Results:
Ninety-five residents were included. After training, the duration of the pre-delivery phase was found to be longer for the trained residents (relative risk (RR)=3.04; P<0.001). The simulated relative’s first turn of speech about the bad news came more often during the pre-delivery phase (RR=6.68; P=0.008), and was more often initiated by the trained residents (RR=19.17; P<0.001). Trained residents also used more assessment (RR=1.83; P<0.001) and supportive utterances (RR=1.58; P<0.001).
Conclusion:
This study demonstrates that a training programme that focuses on the practice of dyadic and triadic communication skills can improve the communication skills of the participating residents in a BBN triadic consultation. Such a training should be included in resident curriculum.
Similar content being viewed by others
Main
Frequently, a patient’s relatives, who may also represent the patient’s primary caregivers, accompany a patient to breaking bad news (BBN) consultations in order to provide support, or to serve as the patient’s advocate (Eggly et al, 2006a; Figg et al, 2010). Therefore, a BBN consultation may impact the emotional state of both a patient (Fallowfield and Jenkins, 2004; Schmid Mast et al, 2005; Lienard et al, 2006) and their relatives (Lienard et al, 2008). In addition, the presence of a relative during BBN consultations often introduces certain complexities as physicians need to deal with two persons who have different needs, knowledge, concerns, distress levels, and expectations (Street and Gordon, 2008). This situation represents a challenge for the physician who needs to assess, inform, and support both the patient and their relatives adequately (Lang et al, 2002; Delvaux et al, 2005; Baile et al, 2006; Eggly et al, 2006a, 2006b).
Although several authors have recognised the need to adjust communication skills to accommodate the concerns of both patients and relatives during triadic BBN consultations (Delvaux et al, 2005; Baile et al, 2006; Eggly et al, 2006a, 2006b), guidelines and recommendations have mainly focused on providing effective dyadic consultations (which include only the patient; Girgis and Sanson-Fisher, 1995; Baile et al, 2000; Fallowfield and Jenkins, 2004). For example, BBN in dyadic consultation is considered as a three-phase process involving different tasks (Lienard et al, 2010a). An adaptation of this three-phase process to a triadic consultation, while also addressing BBN guidelines and recommendations to facilitate effective communication with relatives (Lang et al, 2002; Delvaux et al, 2005), would include the following phases. The first phase would be devoted to preparing the patient and his/her relative for the delivery of bad news by assessing what they know, understand, and feel about the current situation. This would be referred to as the ‘pre-delivery phase’. The second phase, the ‘delivery phase’, would be devoted to delivering the bad news precisely and concisely. Finally, the third phase, the ‘post-delivery’ phase, would be devoted to providing emotional support and additional information to both the patient and their relatives. Completing these three phases represents a complex task that requires the use of specific communication skills for which physicians in general, and residents in particular, have not been sufficiently trained.
Very few studies have been conducted to evaluate communication skills training on BBN. In two randomised controlled studies, communication skills training was found to be effective in improving BBN dyadic consultations (Razavi et al, 2003; Lienard et al, 2010a). Additional results to study by Razavi et al have shown that physicians, following training, used communication skills that reflected a greater openness towards the concerns and needs of patients and their relatives during BBN triadic consultations (Delvaux et al, 2005). Given the limited training provided to physicians for these types of consultations, the efficacy of training programmes focused on BBN training in a triadic setting, needs to be evaluated.
A 40-h dyadic and triadic communication skills training programme has been designed for residents specialising in various disciplines (the Belgian Interuniversity Curriculum—Communication Skills Training (BIC-CST); Bragard et al, 2006). BIC-CST is learner-centred, skills-focused, practice-oriented, and tailored to address a participant’s individual needs (Fallowfield et al, 2002; Razavi et al, 2003; Roter, 2003). Moreover, 10 h of this training programme specifically focus on triadic communication. It should also be noted that this study was part of a larger study that assessed the efficacy of the BIC-CST programme. Although previous reports have described improvements in the communication skills of trained residents in a simulated BBN dyadic consultation (Lienard et al, 2010a), as well as in residents’ daily practice (Lienard et al, 2010b), the aim of the present study was to assess the communication skills of residents in a simulated BBN triadic consultation.
Specifically, this study was designed to evaluate three hypotheses. The first is that the BIC-CST programme will lead to an improvement in the time allocated to each of the three phases of the BBN process, including a longer pre-delivery phase and a shorter delivery phase, in a simulated BBN triadic consultation. The second hypothesis is that residents will include the simulated relative sooner over the course of the consultation and will generally promote his or her participation, especially response to the bad news, following training. Third, trained residents will have acquired assessment and supportive skills that will help them to be more focused on both the simulated patient and the simulated relative during a BBN consultation. As a result, the simulated patient and simulated relative would be expected to more readily express their concerns.
Materials and Methods
Subjects
Inclusion criteria for this study included the ability to speak French and a willingness to participate in the training programme and its assessment procedure. In addition, the enrolled physicians must have had experience, or will be gaining experience, working with cancer patients (part or full time). Residents already participating in another psychological training programme during the assessment and training periods were excluded.
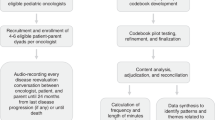
Study design and assessment procedure
The efficacy of the BIC-CST programme was assessed by assigning medical residents who completed an initial assessment to either a 40-h training programme group (training group) or a waiting list (waiting list group), according to a computer generated randomisation list. Assessments were made before randomisation for both groups, after completion of the training programme for the training group and 8 months after the first assessment for the waiting list group. For each assessment, a BBN triadic consultation was conducted with a simulated patient and a simulated relative.
Training programme
The BIC-CST programme included 30 h of communication skills training and 10 h of stress management training (Bragard et al, 2006). Sessions were spread over an 8 months period, with bimonthly small group sessions (including up to seven participants). The communication skills training module consisted of a 17-h communication skills training programme that focused on dyadic consultations, and included six sessions (one 1-h, one 4-h, and four 3-h sessions). In addition, a 10-h communication skills training programme focusing on triadic consultations (i.e., when a relative accompanies a patient) included three sessions (one 4-h and two 3-h sessions), as well as a final 3-h session promoting integration of learned communication and stress management skills. During training, residents were invited to practice communication skills in role play sessions. The residents then received immediate feedback based on the communication skills demonstrated. During the course, the facilitator also gradually introduced the three phases of the BBN process.
Based on previous research on triadic consultations (Delvaux et al, 2005), a specific 10-h training programme was developed, which focuses on triadic interviewing skills in general, with a specific emphasis on BBN skills. This training programme was designed to improve assessment, informative, and supportive skills in triadic consultations, with the goal of providing a specific actual role for both the patient and the relative.
It should be noted that physicians were not specifically instructed to increase the pre-delivery phase and decrease the delivery phase. Changes in the time allocated to each of the three phases were expected to result from changes in the BBN process. In contrast, residents were specifically instructed to include the relative in the BBN process from the start of the consultation by clarifying, as appropriate, the needs, concerns, and expectations of the relative.
Simulated triadic consultation
The communication skills of each resident were evaluated using a simulated BBN triadic consultation, which has been shown to be a valid method for the study of communication style (Roter et al, 1995). Consultations were audiotaped. The simulated triadic consultation consisted of a 20-min first medical encounter with an actress playing a 37-year-old female patient and an actor playing her 40-year-old spouse. During this consultation, residents had to deliver a breast cancer diagnosis and to discuss treatment (i.e., surgery, chemotherapy, and radiotherapy). Before the simulated triadic consultation, residents had sufficient time to learn the case description and the aim of the consultation. Audiotapes of the simulated triadic consultations were transcripted.
Breaking bad news (BBN) process analysis
The three phases of the BBN process – pre-delivery, delivery, and post-delivery – are relevant for the analysis of communication skills training (Lienard et al, 2010a). To evaluate these phases, the precise moment when residents presented the cancer diagnosis was identified in the transcripts of the simulated consultations. This would include when the word ‘cancer’ was used, or when residents confirmed the diagnosis of cancer following a question asked by the simulated patient or relative. Thus, the ‘pre-delivery phase’ represents the period from the beginning of the consultation to the beginning of the utterance used to deliver the cancer diagnosis. Next, the ‘delivery phase’ is the period that consists of the turn of speech where residents deliver the cancer diagnosis. Then, the ‘post-delivery phase’ is the period that spreads from the beginning of the first utterance following the diagnosis delivery to the end of the simulated patient consultation.
Efficacy of the training programme was assessed based on the time allocated to each of the three phases, which was analysed in seconds.
Relative’s inclusion analysis
Transcripts were also analysed to evaluate the efficacy of the training programme for providing inclusion of the relative in the simulated BBN consultation. Thus, for the 20-min BBN consultation, every turn of speech by the relative was tagged and analysed. An investigator then assessed whether these turns of speech were initiated by the resident or not. Turns of speech regarding the bad news included those when the relative expressed his opinions, concerns, needs, or questions about the medical situation of the patient. In particular, the relative’s first turn of speech regarding the bad news presented was analysed with respect to: the initiator of the first turn of speech (i.e., initiated by the resident or not), the phase of the first turn of speech (i.e., during the pre- or post-delivery phase), and the timing of the first turn of speech (in seconds). The investigator was blinded to time assessment and group assignment data.
Communication content analysis
Transcripts of the simulated triadic consultations were analysed by a French communication content analysis software, LaComm (Centre de Psycho-oncologie, Brussels, Belgium). This software analyses verbal communication used (in medicine in general, and in oncology in particular) utterance by utterance, and identifies turns of speech, as well as the type and content of utterances. The explanation of how this software works has been detailed in a previously published paper (Lienard et al, 2010a). Utterances were categorised into three main types: assessment, support, and information, and were only analysed for residents. Regarding utterance content, three dictionaries were constructed: medical, emotional, and social. LaComm provided counts of turns of speech, utterance types, and content.
Statistical analyses
As the participation type, level and rate are directly related to training outcomes, and to avoid to inflate the benefit of the CST tested in this study, it was decided to perform an ‘intention to treat’ analysis instead to test the training effect. Therefore, all data from physicians that had attended at least 1 h of communication skills training were analysed. Eight residents were not included in the BBN process analyses (three in the training group and five in the waiting list group) as they did not explicitly communicate the cancer diagnosis in the simulated triadic consultation. They were of course included in all the other analyses done for this study.
Dependent variables that were analysed included: utterance types and utterance contents (generated by LaComm), the number of turns of speech by residents and actors (generated by LaComm), the three-phase BBN process (in seconds), and the simulated relative’s inclusion analysis (analysed by a blinded investigator). To evaluate the training effect, group-by-time effects were assessed using generalised estimating equation (GEE) regression models. Dependent variables were identified as normal, binomial, Poisson, or binomial negative distributions as appropriate. All tests were two-tailed, and alpha was set at 0.05. Analyses were performed using SPSS Version 16.0 for PC (SPSS Inc, Chicago, IL, USA).
Results
Socio-demographic data of residents
A total of 113 residents registered for the BIC-CST programme (Figure 1), and 95 residents completed simulated BBN triadic consultations. A comparison of the included and excluded residents showed no statistically significant differences in resident age, gender, or year and residency specialty. In regard to socio-demographic and socio-professional characteristics, there were also no statistically significant differences found at baseline between residents of the training group vs the waiting list group, except for family situation and residency specialty: participants in the waiting list group lived with a partner more often than the training group participants (P=0.06), and were more often residents in oncology (P=0.027).
Residents in the training group had a mean age of 28 years (s.d.=3 years), 67% were female, 38% lived alone, and 35% lived with a partner. In addition, most residents in the training group were in their third year of residency (s.d.=1.3 years). Specialties of the training group residents included oncology (including oncology, haematology, and radiotherapy; 6%), gynaecology (31%), and other specialties (63%). Only five residents in the training group had attended a very brief and informal communication skills training in the last year.
Residents in the waiting list group had a mean age of 28 years (s.d.=2.2 years), 60% were female, 26% lived alone, and 60% lived with a partner. In addition, on average the participants were in their third year of residency (s.d.=1.2 years), with 26% being residents in oncology, 21% in gynaecology, and 53% in other specialties. None of the waiting list residents had attended a brief communication skills training workshop in the last year.
Trained residents participated in an average of 25 h of training (s.d.=7.9), with an average of 8 h of training spent in the 10-h stress management skills module (s.d.=2.4), 17 h in the 30-h communication skills module (s.d.=6.6), and 7 h in the 10-h triadic consultation training of the communication skills module (s.d.=3.3).
Training effects on the three phases of the BBN process
Time allocated to each of the three phases of the BBN process were analysed using a GEE regression model. As shown in Table 1 and Figure 2, regression analyses showed significant changes in the duration of the ‘pre-delivery phase’ (relative risk (RR)=3.04; P<0.001) and the ‘post-delivery phase’ (RR=0.93; P<0.001) between the training group and the waiting list group. Moreover, the ‘pre-delivery phase’ lasted longer and the ‘post-delivery phase’ was shorter for trained residents compared with untrained residents.
Training effects on simulated relative’s inclusion
In general, analysis using a GEE identified significant differences in the initiation of turns of speech by the simulated relative between the two groups (Table 2). A significant increase in the number of turns of speech by the simulated relative initiated by trained residents was observed (RR=2.74; P<0.001). In addition, after training, the simulated relative’s first turn of speech regarding the bad news delivered was more frequently initiated by residents (RR=19.17; P<0.001) and occurred more frequently during the pre-delivery phase (RR=6.68; P=0.008) according to GEE analysis (Table 3 and Figure 2). A significant decrease in the timing of the first turn of speech among trained residents was observed (RR=0.56; P=0.014).
Training effects on the utterance types used by residents
GEE analysis also detected significant differences between the two groups of residents in the number of utterance types used (Table 2). Regression analyses showed a significant increase in the rate of open directive questions (RR=2.14; P=0.001), checking questions (RR=1.66; P=0.034), ‘other types of questions’ (RR=2.06; P<0.001), and total assessment types (RR=1.83; P<0.001) used by trained residents compared with untrained residents. A significant increase in the rate of acknowledgement utterances (RR=1.59; P<0.001) and total support utterances (RR=1.58; P<0.001) were also observed for the trained residents. In contrast, GEE analyses identified a significant decrease in the rate of procedural information utterances used by trained residents (RR=0.83; P=0.047).
Training effects on turns of speech by residents and the simulated patient and relative
Attendance in the BIC-CST programme was associated with a significant increase in the number of utterances used by residents and the simulated patient and relative according to GEE analysis (Table 2). When the second assessment was compared with baseline, a significant increase in the number of turns of speech identified for residents (RR=1.25; P<0.001), the simulated patient (RR=1.25; P=0.012), and the simulated relative (RR=1.25; P=0.001) were observed for the training group compared with the waiting list group.
Training effects on utterance content by residents and the simulated patient and relative
GEE analyses also detected significant effects on utterance content by residents, as well as the simulated patient and relative between the training group and waiting list group (Table 2). For residents, when the second assessment session was compared with baseline, regression analyses showed a significant decrease in the count of medical (RR=0.81; P<0.001) and social (RR=0.84; P=0.040) words used, and a downward trend in the count of emotional words used (RR=0.79; P=0.088) for the training group compared with the control group. For the simulated patient, regression analysis showed a significant increase in the use of medical (RR=1.55; P<0.001) and emotional (2.76; P<0.001) terms in the second assessment session compared with baseline for the training group compared with the control group. Similarly, the simulated relative also used a significantly greater number of medical words (RR=1.37; P=0.005), and a marginally greater number of emotional words (RR=2.04; P=0.075), in the second assessment session according to regression analyses performed for the training group and the waiting list group.
Discussion
The objective of the current study was to assess the efficacy of a communication skills programme that provided both dyadic and triadic communication training to residents in order to improve their skills for BBN consultations. For this study, the BIC-CST programme was applied (Bragard et al, 2006), and the skills taught were evaluated using a simulated triadic consultation. The results obtained demonstrate that the training programme did have a positive impact on the simulated BBN process, with residents exhibiting improved communication skills, improved inclusion of a simulated relative, and improved expression of the concerns by the simulated patient and relative.
Initially, it was hypothesised that the BIC-CST programme would modify the time allocated to each of the three phases of the BBN process. Specifically, the duration of the ‘pre-delivery phase’ would increase, whereas the duration of the ‘delivery phase’ would decrease. The results of the present study confirmed the former, yet not the latter, aspects of this hypothesis. The ‘pre-delivery phase’ lasted approximately 1 min before training, and lasted approximately 2 min after training. Although the overall duration of this phase remains short, it could still represent the time needed for the resident to assess what the patient and relative feel, know, and understand about their situation.
Regarding the simulated relative, it was hypothesised that the BIC-CST programme would affect inclusion of the relative during a consultation. More precisely, the residents would be trained to address the relative’s concerns during the consultation more often, particularly concerns related to the bad news. The results of this study confirm this hypothesis, with turns of speech by the simulated relative being initiated two and a half times more often by residents after training. Moreover, assessments of the relative’s concerns about cancer by residents also increased following training, with approximately 90% of trained residents addressing the simulated relative’s concerns regarding the bad news in a consultation compared with only 40% of residents before training. In addition, residents also addressed the concerns of the simulated relative more often in the ‘pre-delivery phase’ following training. Taken together, these results suggest that the ability of the residents to include the simulated relative in the BBN consultations was improved following training.
Regarding the residents’ communication skills, it was hypothesised that the BIC-CST programme would increase the use of assessment and supportive skills, and the results of this study confirm this hypothesis. Trained residents used more assessment and supportive utterances, as well as more open directives, checking questions, other type of questions, and acknowledgements compared with untrained residents. Based on these results, the BIC-CST programme appears to provide residents with communication skills that are more patient- and relative-centred. However, it should be noted that the number of information utterances by residents remained unchanged following training. Therefore, the global improvement in the communication skills of residents included in this study was not associated with a decrease in the number of information utterances provided.
For the same duration of consultation, it was observed that the number of turns of speech by residents, the simulated patient, and the simulated relative increased significantly, and in the same proportions (RR=1.25), following training. It is possible this reflects the use of shorter sentences, and therefore, may reflect a more interactive consultation. Furthermore, it should be noted that trained residents used less emotional, medical, and social words, whereas the simulated patient and relative expressed more emotional and medical words. These changes may be a consequence of the open assessment and supportive skills acquired by the residents with training. These skills do not necessarily require the use of many words, and they allow the simulated patient and relative to express a greater number of concerns. Thus, the results of the present study suggest that the training programme applied taught residents to accommodate expression of concerns by the patient and relative.
This study demonstrates that the BIC-CST programme improves management of the pre-delivery phase by increasing the time spent before delivering bad news, and by including the patient’s relative sooner and more often in the consultation. In addition, the results of the present study show that interactions during simulated BBN triadic consultations changed after training: residents learned to use specific skills more appropriate for BBN triadic consultations, and learned how to be more both patient- and relative-centred.
This study has several strengths. First, a three-phase BBN model was used as part of the training programme applied. Second, the training programme has been designed based on a former training programme, which was assessed for its efficacy with respect to training techniques and duration in a simulated BBN triadic consultation (Delvaux et al, 2005). Third, the facilitators involved were experienced and had been trained together in the perspective of this study. Fourth, a randomised controlled design was used to assess efficacy (Merckaert et al, 2005), whereas the use of a simulated BBN consultation setting using actresses and actors provided a high test–retest validity for the study with repeated measures. Finally, the use of a content analysis software to assess residents’ communication skills based on transcripts recorded during simulated BBN consultations avoided the potential for inter-rater variability.
As it has been underlined in our previous paper, this study has some limitations (Lienard et al, 2010a). In particular, this study has not assessed the transfer of learned triadic BBN skills to clinical practice. Methodologically, although the outcomes assessed in this study are valid given the scenario selected for the simulated consultation, they may not be valid for a study designed to assess the transfer of learned skills to clinical practice (Delvaux et al, 2005). To study the transfer of learned skills to clinical practice, the choice of the outcomes should be based on the clinical context studied. For example, a decrease of residents’ medical, social, and emotional utterances may be not positive, if information to be transmitted are highly complex. For example, also an increase of duration of the pre-delivery phase can be rated as being not beneficial for the patients, as it might be due to avoidant behaviour, if the resident has already met the patient and his relative. The usefulness of early and repeated inclusions of relatives should also be considered according the clinical context studied. A study focusing on the transfer of learned triadic BBN skills to clinical practice could therefore assess how the patient and his relative feel during triadic communication. Furthermore, those studies are needed before an intensive training programme can be included in the curriculum for residents.
Change history
12 November 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP (2000) SPIKES-A six-step protocol for delivering bad news: application to the patient with cancer. Oncologist 5: 302–311.
Baile WF, Buckman R, Schapira L, Parker PA (2006) Breaking bad news: more than just guidelines. J Clin Oncol 24: 3217.
Bragard I, Razavi D, Marchal S, Merckaert I, Delvaux N, Libert Y, Reynaert C, Boniver J, Klastersky J, Scalliet P, Etienne AM (2006) Teaching communication and stress management skills to junior physicians dealing with cancer patients: a Belgian Interuniversity Curriculum. Support Care Cancer 14: 454–461.
Delvaux N, Merckaert I, Marchal S, Libert Y, Conradt S, Boniver J, Etienne AM, Fontaine O, Janne P, Klastersky J, Melot C, Reynaert C, Scalliet P, Slachmuylder JL, Razavi D (2005) Physicians' communication with a cancer patient and a relative: a randomized study assessing the efficacy of consolidation workshops. Cancer 103: 2397–2411.
Eggly S, Penner L, Albrecht TL, Cline RJ, Foster T, Naughton M, Peterson A, Ruckdeschel JC (2006a) Discussing bad news in the outpatient oncology clinic: rethinking current communication guidelines. J Clin Oncol 24: 716–719.
Eggly S, Penner LA, Greene M, Harper FW, Ruckdeschel JC, Albrecht TL (2006b) Information seeking during "bad news" oncology interactions: Question asking by patients and their companions. Soc Sci Med 63: 2974–2985.
Fallowfield L, Jenkins V (2004) Communicating sad, bad, and difficult news in medicine. Lancet 363: 312–319.
Fallowfield L, Jenkins V, Farewell V, Saul J, Duffy A, Eves R (2002) Efficacy of a Cancer Research UK communication skills training model for oncologists: a randomised controlled trial. Lancet 359: 650–656.
Figg WD, Smith EK, Price DK, English BC, Thurman PW, Steinberg SM, Emanuel E (2010) Disclosing a diagnosis of cancer: where and how does it occur? J Clin Oncol 28: 3630–3635.
Girgis A, Sanson-Fisher RW (1995) Breaking bad news: consensus guidelines for medical practitioners. J Clin Oncol 13: 2449–2456.
Lang F, Marvel K, Sanders D, Waxman D, Beine KL, Pfaffly C, Mccord E (2002) Interviewing when family members are present. Am Fam Physician 65: 1351–1354.
Lienard A, Merckaert I, Libert Y, Bragard I, Delvaux N, Etienne AM, Marchal S, Meunier J, Reynaert C, Slachmuylder JL, Razavi D (2010a) Is it possible to improve residents breaking bad news skills? A randomised study assessing the efficacy of a communication skills training program. Br J Cancer 103: 171–177.
Lienard A, Merckaert I, Libert Y, Bragard I, Delvaux N, Etienne AM, Marchal S, Meunier J, Reynaert C, Slachmuylder JL, Razavi D (2010b) Transfer of communication skills to the workplace during clinical rounds: impact of a program for residents. PLoS One 5: e12426.
Lienard A, Merckaert I, Libert Y, Delvaux N, Marchal S, Boniver J, Etienne AM, Klastersky J, Reynaert C, Scalliet P, Slachmuylder JL, Razavi D (2006) Factors that influence cancer patients' anxiety following a medical consultation: impact of a communication skills training programme for physicians. Ann Oncol 17: 1450–1458.
Lienard A, Merckaert I, Libert Y, Delvaux N, Marchal S, Boniver J, Etienne AM, Klastersky J, Reynaert C, Scalliet P, Slachmuylder JL, Razavi D (2008) Factors that influence cancer patients' and relatives' anxiety following a three-person medical consultation: impact of a communication skills training program for physicians. Psychooncology 17: 488–496.
Merckaert I, Libert Y, Razavi D (2005) Communication skills training in cancer care: where are we and where are we going? Curr Opin Oncol 17: 319–330.
Razavi D, Merckaert I, Marchal S, Libert Y, Conradt S, Boniver J, Etienne AM, Fontaine O, Janne P, Klastersky J, Reynaert C, Scalliet P, Slachmuylder JL, Delvaux N (2003) How to optimize physicians' communication skills in cancer care: results of a randomized study assessing the usefulness of posttraining consolidation workshops. J Clin Oncol 21: 3141–3149.
Roter DL (2003) Observations on methodological and measurement challenges in the assessment of communication during medical exchanges. Patient Educ Couns 50: 17–21.
Roter DL, Hall JA, Kern DE, Barker LR, Cole KA, Roca RP (1995) Improving physicians interviewing skills and reducing patients emotional distress - a randomized clinical-trial. Arch Intern Med 155: 1877–1884.
Schmid Mast M, Kindlimann A, Langewitz W (2005) Recipients' perspective on breaking bad news: how you put it really makes a difference. Patient Educ Couns 58: 244–251.
Street RL, Gordon HS (2008) Companion participation in cancer consultations. Psychooncology 17: 244–251.
Acknowledgements
This research programme was supported by the Fonds National de la Recherche Scientifique—Section Télévie of Belgium, and by the C.P.O. training and research group (Brussels, Belgium).
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Merckaert, I., Liénard, A., Libert, Y. et al. Is it possible to improve the breaking bad news skills of residents when a relative is present? A randomised study. Br J Cancer 109, 2507–2514 (2013). https://doi.org/10.1038/bjc.2013.615
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.615
Keywords
This article is cited by
-
Quality of breaking bad news to patients diagnosed with neoplasia of the uterine cervix
Journal of Cancer Research and Clinical Oncology (2023)
-
Neurologists’ current practice and perspectives on communicating the diagnosis of a motor neurodegenerative condition: a UK survey
BMC Neurology (2021)
-
Advance care planning in progressive neurological diseases: lessons from ALS
BMC Palliative Care (2019)
-
Schlechte Nachrichten besser übermitteln
Info Onkologie (2014)
-
L’intégration de la psycho-oncologie dans les formations en cancérologie. Les recommandations de la Société Française de Psycho-Oncologie (SFPO)
Psycho-Oncologie (2014)