Abstract
Purpose
To compare the effect of dorzolamide hydrochloride 2%, timolol maleate 0.5%, and their fixed combination on intraocular pressure (IOP) and retinal and optic nerve head haemodynamics in primary open-angle glaucoma patients.
Methods
Twenty-eight patients with early-moderate glaucomatous damage treated with β-blockers (>6 months) with IOP values ranging from 18 to 22 mmHg at trough participated in this trial. After a 4-week washout period, patients were randomized in two groups: group I started with dorzolamide 2% monotherapy and group II with timolol 0.50% monotherapy for 4 weeks. After this period, both groups switched to dorzolamide/timolol fixed combination for 4 weeks. IOP, ocular diastolic perfusion pressure (ODPP), heart rate, and Scanning Laser Doppler Flowmetry measurements at the peripapillary retina and neuroretinal rim were taken at T0 (enrolment), T1 (wash out), T2 (monotherapy), and T3 (dorzolamide/timolol). Data were compared between different study times. Statistical analysis was conducted using a paired t-test.
Results
Between T1 and T3, IOP decreased significantly in group I (−21.40%) (P<0.001) and in group II (−21.25%) (P<0.001). At the same time intervals, blood flow increased significantly at rim level for group I (+30.03%) (P<0.05) and also when all patients were considered (rim +17.99%) (P<0.05). Between T1 and T3, we also observed a significant increase of ODPP in group I (+7.24%) (P<0.01) and in group II (+6.08%) (P<0.05) and when all patients were considered (+8.43%) (P<0.01).
Conclusions
Dorzolamide/timolol fixed combination increased blood flow significantly at the neuroretinal rim showing a combination of hypotensive and haemodynamic effects.
Similar content being viewed by others
Introduction
Glaucoma is a multifactorial, progressive optic neuropathy characterized by an acquired loss of retinal ganglion cells and optic nerve atrophy, which results in characteristic visual field defects. The aetiology of glaucomatous damage has not yet been fully defined. Increased intraocular pressure (IOP) is the most recognized and thoroughly studied risk factor for glaucomatous optic neuropathy; however, the progression of glaucomatous damage in patients with lowered IOP and normal tension glaucoma (NTG) suggests the existence of risk factors other than IOP.1, 2, 3 Ischaemia has been suggested to play a major role in the pathogenesis of primary open-angle glaucoma (POAG).4, 5, 6
In POAG and NTG patients, ONH and retinal tissue perfusion are chronically reduced.7, 8 This reduction is greater in patients with lower mean arterial pressure (MAP), and in POAG, ONH flow correlates directly with MAP. Therefore, every reduction in ocular perfusion due to variations in IOP or MAP could reduce ONH perfusion.9 In a previous study on asymmetric POAG patients, we observed statistically significant reductions of volume and flow in eyes with greater functional and structural damage.10, 11
Given the increasing importance of vascular factors in the pathogenesis of glaucomatous damage, it is of great experimental and clinical interest that current antiglaucomatous therapies be tested for their vascular activity.
By using non-invasive technologies such as Scanning Laser Doppler Flowmetry (SLDF) and analysis softwares that produce highly reproducible intrasession and intersession results such as the Automatic Full Field Perfusion Image Analyzer software (AFFPIA-SLDF 3.3, G Michelson, Erlangen, Germany),12, 13, 14, 15, 16, 17, 18 it is possible to accurately assess the haemodynamic effects of antiglaucomatous drugs.
Topical β-blockers are the most commonly prescribed initial therapy for the treatment of elevated IOP in patients with glaucoma. A number of studies have addressed the role of β-blockers on ocular blood flow (OBF).19, 20, 21, 22 Reports on the effect of timolol, a non-selective, topical β-blocker that lowers IOP through the reduction of aqueous humour production on OBF, are contradictory.21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51
Almost half of the patients treated with timolol require combination therapy to control IOP and glaucomatous damage.23 Dorzolamide is one of the most commonly used molecules in combination therapy (D/T) with timolol. This drug lowers IOP by inhibiting carbonic anhydrase isoenzymes II and IV in the ciliary processes24, 25 with minimal systemic and ocular side effects.23 Dorzolamide could have a positive effect on retinal and peripapillary haemodynamics owing to its ability to induce local metabolic acidosis and consequently relax arteriolar pericytes.26, 27
Evidence in literature on the effects of dorzolamide on OBF is contrasting. In normal eyes, it improved central visual function during hyper- and hypocapnia conditions.28 Using colour Doppler imaging, Martinez et al29 found that most haemodynamic parameters of intraocular and periocular vessels improve after application of topical dorzolamide in both normal and glaucomatous eyes. In newly diagnosed POAG patients, Galassi et al30 observed a significant reduction of resistivity index at the temporal short posterior ciliary artery. Dorzolamide has also been shown to significantly increase pulsatile ocular blood flow (POBF) in glaucoma patients.31, 32 In NTG patients, dorzolamide significantly reduced arteriovenous passage (AVP) time in the superior temporal retina and improved contrast sensitivity at both 3 and 6 cycles/degree.33, 34 Other studies on retrobulbar vessels35 and at the retinal level36 did not find any significant effect of dorzolamide instillation on OBF in healthy subjects. The fixed combination of timolol and dorzolamide (D/T) has been proven to be as effective in lowering IOP as the concomitant use of the two molecules and more effective than either in monotherapy.23, 37, 38, 39, 40 Additionally, it has been reported that AVP time (superior temporal artery) was significantly accelerated using D/T as compared to timolol in glaucoma patients40 and that the D/T fixed combination significantly increased POBF in POAG patients.41
The aim of the present study was to evaluate the effect of dorzolamide 2% and timolol 0.5% in monotherapy and dorzolamide/timolol fixed combination on IOP and on retinal and ONH blood flow in early and moderate POAG patients to better define the therapeutic potential of these drugs.
Methods
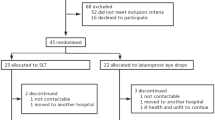
This was a comparative, randomized, open label clinical study.
We enrolled 28 patients (28 eyes) (11 men, 17 women; mean age 58.31±5.12 years) (Table 1) with POAG and early-moderate glaucomatous damage. All patients had previous treatment with β-blockers (at least 6 months), with IOP values ranging from 18 to 22 mmHg at trough and were screened at the Glaucoma Center of the University of Torino Eye Clinic.
The screening visit included case history, biomicroscopy, gonioscopy, fundus examination, IOP measurement, and automatic static perimetry using the Octopus 500 (program G1). Patients were classified as glaucomatous if they had a repeatable abnormal visual field (three consecutive). According to the Hodapp grading scale (1993),42 18 patients (64.3%) were classified as having early visual field defects and 10 (35.7%) moderate defects. Other inclusion criteria were a best-corrected visual acuity of 0.5 or better, ametropia <5 D, good dioptric transparency.
Patients were excluded if they had any of the following: cardiovascular and/or metabolic diseases (known to affect blood flow, as diabetes and polycythaemia); visual field defects other than glaucoma; use of vasoactive and/or antihypertensive drugs; systemic use of acetazolamide; hypersensibility to any of the molecules studied; previous ocular surgery; and pregnant or nursing women.
The research followed the tenets of the Declaration of Helsinki and informed consent was obtained from all enrolled patients. The study was approved by the Institutional Review Board.
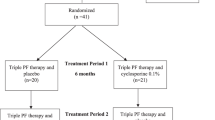
Testing occurred over a period of approximately 12 weeks.
At enrolment (T0), one eye per patient was randomly selected. All patients underwent a complete ophthalmological examination, IOP (Goldmann applanation tonometry), blood pressure (BP) and ocular diastolic perfusion pressure (ODPP=arterial diastolic pressure−IOP), heart rate (HR) measurements, and evaluation of retinal and ONH blood flow between 0800 and 1000 hours at trough (12 h after the antiglaucomatous treatment). All qualifying patients underwent a 4-week washout period. At the end of the washout period, all measurements were repeated (T1) and patients were randomly divided into two 14-patient groups assigned to receive either dorzolamide 2% t.i.d. (group I) or timolol 0.50% b.i.d. (group II) for 4 weeks (Table 2). All measurements were repeated and then both groups switched to a 4-week fixed combination (D/T) run-in followed by a new set of measurements.
Evaluations of brachial artery pressure and radial pulse were obtained in a sitting position after 5 min of rest. Brachial artery pressures were measured using a BP cuff and a stethoscope. HR was determined manually using a stopwatch. Systolic and diastolic BP were taken before ocular perfusion measurements.
Retinal and ONH blood flow were measured non-invasively with SLDF using the Heidelberg Retina Flowmeter (HRF; Heidelberg Laboratories, Germany).
Three scans of the peripapillary retina and ONH were acquired for each eye using a 10° × 2.5° measurement box. We selected three regions of interest:
-
superior peripapillary retina
-
inferior peripapillary retina
-
central peripapillary retina and the neuroretinal rim at the temporal side.
All scans were performed by the same operator.
The Automatic Full Field Perfusion Image Analyzer software (AFFPIA-SLDF 3.3; G Michelson, Erlangen, Germany) was then used on each scan. This software enhances the computations generated by the HRF by excluding pixels with incorrect brightness, marking saccades that lead to erroneous perfusion data, and eliminates pixels of retinal vessels with a diameter greater than 30 μm. The analysis is based on the average of all valid image points with the perfusion map divided into neuroretinal rim area, temporal peripapillary retinal area, and nasal peripapillary retinal area. Each area is analysed separately. It was demonstrated recently that AFFPIA analysis produces highly reproducible intrasession and intersession measurements of ONH and peripapillary retinal blood flow.43
As a result of the AFFPIA analysis, for every scan we had separate data relative to average temporal, nasal, and rim flow. All the data were grouped by retinal area (temporal, nasal, rim), study group (group I, group II, global), and study time (T0, T1, T2, T3).
The main study outcomes of our study were IOP, ODPP, and retinal blood flow.
The power to detect differences between groups for the main study comparisons was calculated on the basis of t-test. P<0.05 was considered significant.
ANOVA between groups for IOP, BP, HR, ODPP, and flow was used at baseline. P<0.05 was considered significant.
Statistical analysis was conducted using the paired t-test. We compared data measured at different study times. P-values <0.05 were considered statistically significant. The percentage variation was intended as [(x1−x2)/x2] × 100, where x is the mean data at study time Ti. For every study variable, the analysis was conducted separately for the two groups and considering all patients.
Analysis of covariance was performed between ODPP and flow using ODPP as a covariate.
Results
ANOVA between groups showed no difference in IOP, BP, HR, ODPP, and flow at baseline (T0).
Patient's demographic characteristics are shown in Table 1. IOP, HR, and systolic and diastolic BP mean values measured at T0 are also illustrated.
The mean values and standard deviation for IOP, ODPP, HR, systolic and diastolic BP, and HRF flow parameters in the study groups at various study times are reported in Table 2. The percentage variations of mean IOP, ODPP, HR, systolic and diastolic BP, and HRF flow parameter values in the study groups at various study times are reported in Table 3.
Intraocular pressure
From the analysis of IOP data, we observed a significative increase of IOP in all groups between T0 and T1 (P<0.001); a significant decrease of IOP between T1 and T2 in group I (−12.03%) (P<0.001) and in group II (−13.70%) (P<0.001); a significant decrease of IOP between T1 and T3 in group I (−21.40%) (P<0.001) and in group II (−21.25%) (P<0.001); a significant decrease of IOP between T2 and T3 in group I (−10.60%) (P<0.001) and in group II (−8.80%) (P<0.001).
Ocular diastolic perfusion pressure
From the analysis of ODPP data, we observed a significant decrease of ODPP between T0 and T1 in group I (−6.18%) (P<0.05) and when all patients were considered together (−5.42%) (P<0.01); a significant increase of ODPP between T1 and T3 in group I (+7.24%) (P<0.01), in group II (+6.08%) (P<0.05), and in both groups globally (+6.71%) (P<0.001); a significant increase of ODPP between T2 and T3 when both groups were considered together (+2.60%) (P<0.01).
Heart rate and blood pressure
No statistically significant variations in HR and BP values were observed in any of the study groups.
Flow parameters
Analysis of covariance was performed between ODPP and flow using ODPP as a covariate. We observed an increase of flow values between T1 and T3 at rim level in group I (+30.03%) (P<0.05) and when all patients were considered globally (+20.81%) (P<0.05).
Discussion
This study indicates that in POAG eyes treatment with D/T fixed combination lowers IOP values, increases blood flow at the neuroretinal rim, and enhances diastolic perfusion pressure.
Our results are in agreement with recent studies52, 53 that showed a beneficial vascular effect of D/T fixed combination on retrobulbar haemodynamics in patients with OAG.
In a recent study54 on the effect of dorzolamide and timolol on OBF, 140 patients with POAG and OHT were treated for 6 months with either dorzolamide or timolol. SLDF was used to assess blood flow in the temporal neuroretinal rim and cup of the ONH. Dorzolamide, but not timolol, increased blood flow in the temporal neuroretinal rim and cup of the ONH.
We found no significant effect of dorzolamide on the retinal blood flow. Flow values after dorzolamide monotherapy showed an increase (+11.89% at rim level), but this increase was not significant. This could be due to the fact that the group size was too small.
When we compared monotherapy data with D/T data, we found no significant increase in flow parameters after the switch from monotherapy to D/T. These results are in contrast with some clinical studies40 but agree with those reported in a previous study39 conducted by our group on the haemodynamic effects of timolol monotherapy vs fixed combination D/T in POAG patients, where we observed a nonsignificant increase in HRF parameter values at the peripapillary retina and neuroretinal rim after the switch from timolol monotherapy to D/T.
When we compared washout with fixed combination, only patients who were previously treated with dorzolamide and then switched to fixed combination showed increased blood flow. This suggests that the possible positive haemodynamic effect of dorzolamide may be maintained and enhanced by a further reduction in IOP values caused by timolol addition.
D/T fixed combination produced a significant ODPP increase.
In a recent study55 comparing the short-term effects of timolol 0.5%, brimonidine 0.2%, dorzolamide 2%, and latanoprost 0.005% on ODPP, only dorzolamide and latanoprost significantly increased mean 24 h ODPP in newly diagnosed POAG.
In timolol-treated eyes, despite a significant reduction in IOP values (−13.7%), ODPP did not show a significant increase. This may confirm the hypothesis that dorzolamide increases blood flow through a direct vasodilator mechanism and not only through IOP lowering. In addition, the analysis of covariance between ODPP and flow showed that after removing the influence of ODPP, the flow increase at rim level is still significant.
The clinical relevance of our results in glaucoma treatment depends on whether reduced optic nerve head blood flow contributes to glaucoma disease pathogenesis (onset and progression). In POAG and NTG patients, ONH and retinal tissue perfusion are chronically reduced,7, 8 and there is increasing evidence that reduced blood flow is directly associated with progression of visual field loss.56 A significant correlation between ONH blood volume, as assessed by SLDF, and visual field loss in POAG was reported in a recent longitudinal study by Zink et al.57
The HRF technique used for the assessment of blood flow has limitations. The sampling depth within the retinal tissue is not known and reproducibility is a problem,58, 59 particularly in glaucoma patients compared with healthy control subjects.
In conclusion, in POAG eyes, D/T fixed combination produces further IOP reduction and increases blood flow, showing a combination of hypotensive and haemodynamic effects. The addition of a β-blocking agent to dorzolamide-treated eyes could provide a better therapeutic approach in the protection of ONH fibres from glaucomatous damage.
References
Flammer J . The vascular concept in glaucoma. Surv Ophthalmol 1994; 38: 3–6.
Flammer J, Orgul S . Optic nerve blood-flow abnormalities in glaucoma. Prog Retin Eye Res 1998; 17 (2): 267–289. Review.
Drance S, Anderson DR, Schulzer M . Risk factors for progression of visual field abnormalities in normal tension glaucoma. Am J Ophthalmol 2001; 131: 699–708.
Drance SM (ed). A comparison of the effects of betaxolol and timolol on the corrected loss variance in patients with open-angle glaucoma. In: Vascular Risk Factors and Neuroprotection in Glaucoma—Update 1996. Kugler Publications: Amsterdam/New York, 1997, pp 221–226.
Grunwald JE, Sinclair SH, Riva CE . Autoregulation of the retinal circulation in response to decrease of intraocular pressure below normal. Invest Ophthalmol 1982; 23: 124–129.
Galassi F, Nuzzaci G, Sodi A, Casi P, Capelli S, Vielmo A . Possible correlation of ocular blood flow parameters with intraocular pressure and visual field alterations in glaucoma. A study by means of color Doppler imaging. Ophthalmologica 1994; 208: 304–308.
Michelson G, Langhans MJ, Harazny J . Visual field defect and perfusion of the juxtapapillary retina and the neuroretinal rim area in primary open-angle glaucoma. Graefes Arch Clin Exp Ophthalmol 1998; 236 (2): 80–85.
Chung HS, Harris A, Evans DW, Kagemann L, Garzozi HJ . Vascular aspects in the pathophysiology of glaucomatous optic neuropathy. Surv Ophthalmol 1999; 43 (Suppl): S43–S50. Review.
Grunwald JE, Piltz J . Optic nerve blood flow in glaucoma: effect of systemic hypertension. Am J Ophthalmol 1999; 127: 516–522.
Rolle T, Boggio Merlo S, Borasio E, Fornero A, Belli L, Vizzeri GM et al. Glaucoma primario ad angolo aperto ad evoluzione asimmetrica:studio delle alterazioni morfologiche ed emodinamiche. Boll Ocul 2002; 81: 63–67.
Rolle T, Brogliatti B, Fea A, Borasio E, Fornero A, Belli L et al. Structural glaucomatous damage vs visual field defects: longitudinal study in patients with ocular hypertension or early primary open-angle glaucoma. Acta Ophthalmol Scand 2002; 236 (Suppl): 45–46.
Michelson G, Schmauss B . Two dimensional mapping of the perfusion of the retina and optic nerve head. Br J Ophthalmol 1995; 79: 1126–1132.
Michelson G, Schmauss B, Langhans MJ, Harazny J, Groh MJM . Principle, validity and reliability of scanning laser Doppler flowmetry. J Glaucoma 1996; 5: 99–105.
Michelson G, Welzenbach J, Pal I . Automatic full field analysis of perfusion images gained by scanning laser Doppler flowmetry. Br J Ophthalmol 1998; 82: 1294–1300.
Chauhan BC, Smith FM . Confocal scanning laser Doppler flowmetry: experiments in a model flow system. J Glaucoma 1997; 6 (4): 237–245.
Lietz A, Hendrickson P, Flammer J, Orgül S, Haefliger IO . Effect of carbogen, oxygen and intraocular pressure on Heidelberg retina flowmeter parameter ‘flow’ measured at the papilla. Ophthalmologica 1998; 212: 149–152.
Nicolela MT, Hnik P, Schulzer M, Drance SM . Reproducibility of retinal and optic nerve head blood flow measurements with scanning laser Doppler flowmetry. J Glaucoma 1997; 6: 157–164.
Iester M, Altieri M, Michelson G, Vittone P, Calabria G, Traverso CE . Intraobserver reproducibility of a two-dimensional mapping of the optic nerve head perfusion. J Glaucoma 2002; 11: 488–492.
Harris A, Spaeth GL, Sergott RC, Katz LJ, Cantor LB, Martin BJ . Retrobulbar arterial hemodynamic effects of betaxolol and timolol in normal tension glaucoma. Am J Ophthalmol 1995; 120: 168–175.
Arend O, Harris A, Arend S, Remky A, Martin BJ . The acute effect of topical beta-adrenoceptor blocking agents on retinal and optic nerve head circulation. Acta Ophtalmol Scand 1998; 76 (1): 43–49.
Lubeck P, Orgul S, Gugleta K, Gherghel D, Gekkieva M, Flammer J . Effect of timolol on anterior optic nerve blood flow in patients with primary open-angle glaucoma as assessed by the Heidelberg retina flowmeter. J Glaucoma 2001; 10 (1): 13–17.
Haefliger IO, Lietz A, Griesser SM, Ulrich A, Schotzau A, Hendrickson P et al. Modulation of Heidelberg retinal flowmeter parameter flow at the papilla of healthy subjects: effect of carbogen, oxygen, high intraocular pressure, and beta-blockers. Surv Ophthalmol 1999; 43 (Suppl 1): S59–S65.
Clineschmidt CM, Williams RD, Snyder E, Admson IA . A randomized trial in patients inadequately controlled with timolol alone comparing the dorzolamide–timolol combination to monotherapy with timolol or dorzolamide. Dorzolamide–timolol Combination Study Group. Ophthalmology 1998; 105 (10): 1952–1959.
Sugrue MF . Pharmacological and ocular hypotensive properties of topical carbonic anhydrase inhibitors. Prog Retin Eye Res 2000; 19: 87–112.
Maren TH, Conroy CW, Wynns GC, Levy NS . Ocular absorption, blood levels, and excretion of dorzolamide a topically active carbonic anhydrase inhibitor. J Ocul Pharmacol Ther 1997; 13: 23–30.
Reber F, Gersch U, Funk RW . Blockers of carbonic anhydrase can cause increase of retinal capillary diameter, decrease of extracellular and increase of intracellular pH in rat retinal organ culture. Graefes Arch Clin Exp Ophthalmol 2003; 241 (2): 140–148.
Cour M, Kiigard JK, Eystensson T, Wiencke AK, Bang K, Dollerup J et al. Optic nerve oxygen tension: effects of intraocular pressure and dorzolamide. Br J Ophthalmol 2000; 84: 1045–1049.
Harris A, Arend O, Arend S, Martin B . Effects of topical dorzolamide on retinal and retrobulbar haemodynamics. Acta Ophthalmol Scand 1996; 74: 569–572.
Martinez A, Gonzalez F, Capeans C, Perez R, Sanchez-Salorio M . Dorzolamide effect on ocular blood flow. Invest Ophtalmol Vis Sci 1999; 40 (6): 1270–1275.
Galassi F, Sodi A, Renieri G, Ucci F, Pieri B, Harris A et al. Effects of timolol and dorzolamide on retrobulbar haemodynamics in patients with newly diagnosed primary open angle glaucoma. Ophthalmologica 2002; 216 (2): 123–128.
Bernd AS, Pillunat LE, Bohm AG, Schmidt KG, Richard G . Ocular haemodynamics and visual field in glaucoma treatment with dorzolamide. Ophthalmologe 2001; 98: 451–455.
Schmidt KG, von Ruckmann A, Becker R, Pillunat LE . Ocular pulse amplitude, intraocular pressure and beta blocker/carbonic anhydrase inhibition in combined therapy of primary open angle glaucoma. Klin Monatsbl Augenheilkd 1999; 215: 361–366.
Harris A, Arend O, Kagemann L, Garrett M, Chung HS, Martin B . Dorzolamide, visual function and ocular hemodynamics in normal-tension glaucoma. J Ocul Pharmacol Ther 1999; 15: 189–197.
Harris A, Arend O, Chung HS, Kagemann L, Cantor L, Martin B . A comparative study of betaxolol and dorzolamide effect on ocular circulation in normal tension glaucoma patients. Ophthalmology 2000; 107: 430–434.
Grunwald JE, Mathur S, Dupont J . Effects of topical dorzolamide on retinal and retrobulbar hemodynamics. Acta Ophthalmol Scand 1997; 75: 236–238.
Pillunat LE, Bohm AG, Koller AU, Schmidt KG, Klemm M, Richard G . Effect of topical dorzolamide on optic nerve head blood flow. Graefes Arch Clin Exp Ophthalmol 1999; 237: 495–500.
Hutzelmann J, Owens S, Shedden A, Adamsons I, Vargas E . Comparison of the safety and efficacy of the fixed combination of dorzolamide/timolol and the concomitant administration of dorzolamide and timolol: a clinical equivalence study. International Clinical Equivalence Study Group. Br J Ophthalmol 1998; 82: 1249–1253.
Strohmaier K, Snyder E, Dubiner H, Adamsons I, The Dorzolamide–Timolol Study Group. The efficacy and safety of the dorzolamide–timolol combination vs concomitant administration of its components. Ophthalmology 1998; 105: 1936–1944.
Brogliatti B, Rolle T, Vizzeri GM, Cipullo D . Comparison of the efficacy on intraocular pressure and retinal blood flow of a beta-blocker (timolol maleate) against the fixed association of a topical carbonic anhydrase inhibitor (dorzolamide) and a beta-blocker (timolol maleate). Acta Ophthalmol Scand 2000; 78: 47–49.
Harris A, Jonescu-Cuypers CP, Kagemann L, Nowacki E, Garzozi H, Cole C et al. Effect of dorzolamide timolol combination vs timolol 0.5% on ocular blood flow in patients with primary open angle glaucoma. Am J Ophthalmol 2001; 132: 490–495.
Januleviciene I, Harris A, Kagemann L, Siesky B, McCranor L . Comparison of the effects of dorzolamide/timolol fixed combination vs latanoprost on intraocular pressure and pulsatile ocular blood flow in primary open-angle glaucoma patients. Acta Ophthalmol Scand 2004; 82: 730–737.
Hodapp E, Parrish II RK, Anderson DR . Clinical Decision in Glaucoma. The CV Mosby Company: St Louis, MO, 1993, pp 52–61.
Hafez AS, Bizzarro RL, Rivard M, Lesk MR . Changes in optic nerve head blood flow after therapeutic intraocular pressure reduction in glaucoma patients and ocular hypertensives. Ophthalmology 2003; 110 (1): 201–210.
Orgul S, Mansbrger S, Bacon DR, van Buskirk EM, Cioffi GA . Optic nerve vasomotor effects of topical beta adrenergic antagonists in rabbits. Am J Ophthalmol 1995; 120: 456–457.
Maren TH, Wynns GC, Wistrand PJ . Chemical properties of carbonic anhydrase IV the membrane bound enzyme. Mol Pharmacol 1993; 44: 901–905.
Lippa EA, Carlson LE, Ehinger B, Eriksson LO, Finnström K, Holmin C et al. Dose response and duration of action of dorzolamide, a topical carbonic anhydrase inhibitor. Arch Ophthalmol 1992; 110: 495–499.
Ehrenreich DL, Burns RA, Alman RW, Razekas JF . Influence of acetazolamide on cerebral blood flow. Arch Neurol 1961; 5: 125–130.
Rassam SL, Patel V, Kohner EM . The effect of acetazolamide on the retinal circulation. Eye 1993; 7: 697–702.
Arend O, Harris A, Wolter P, Remky A . Evaluation of retinal haemodynamics and retinal function after application of dorzolamide, timolol and latanoprost in newly diagnosed open-angle glaucoma patients. Acta Ophthalmol Scand 2003; 81 (5): 474–479.
Harris A, Migliardi R, Rechtman E, Cole CN, Yee AB, Garozzi HJ . Comparative analysis of the effects of dorzolamide and latanoprost on ocular hemodynamics in normal tension glaucoma patients. Eur J Ophtalmol 2003; 13 (1): 24–31.
Grunwald JE, Riva CE, Stone RA, Keates EU, Petrig BL . Retinal autoregulation in open angle glaucoma. Ophthalmology 1984; 91: 1690–1694.
Martinez A, Sanchez M . Retrobulbar haemodynamic effects of the latanoprost/timolol and the dorzolamide/timolol fixed combinations in newly diagnosed glaucoma patients. Int J Clin Pract 2007; 61 (5): 815–825.
Siesky B, Harris A, Sines D . A comparative analysis of the effects of the fixed combination of timolol and dorzolamide versus latanoprost plus timolol on ocular hemodynamics and visual function in patients with primary open-angle glaucoma. J Ocul Pharmacol Ther 2006; 22 (5): 353–361.
Fuchsjäger-Maryl G, Wally B, Rainer G, Buehl W, Aggermann T . Effect of dorzolamide and timolol on ocular blood flow in patients with primary open angle glaucoma and ocular hypertension. Br J Ophthalmol 2005; 89: 1293–1297.
Quaranta L, Gandolfo F, Turano R, Rovida F, Pizzolante T, Musig A et al. Effects of topical hypotensive drugs on circadian IOP, blood pressure, and calculated diastolic ocular perfusion pressure in patients with glaucoma. Invest Ophthalmol Vis Sci 2006; 47 (7): 2917–2923.
Yamaaki Y, Drance SM . The relationship between progression of visual field defects and retrobulbar circulation in patients with glaucoma. Am J Ophthalmol 1997; 124: 287–295.
Zink JM, Grunwald JE, Piltz-Seymour J, Staii A, Dupont J . Association between lower optic nerve laser Doppler blood flow measurements and glaucomatous visual field progression. Br J Ophthalmol 2003; 87: 1487–1491.
Nicolela MT, Hnik P, Drance SM . Scanning laser Doppler flowmetry study on retinal and optic disk blood flow in glaucomatous patients. Am J Ophthalmol 1996; 122: 775–783.
Strenn K, Menapace R, Rainer G, Findl O, Wolzt M, Schmetterer L . Reproducibility and sensitivity of scanning laser Doppler flowmetry during graded changes in pO2 . Br J Ophthalmol 1997; 81: 360–364.
Acknowledgements
This study was supported by a medical school grant of Merck Sharp & Dohme Inc., NJ, USA.
Author information
Authors and Affiliations
Corresponding author
Additional information
Financial interest: None
Rights and permissions
About this article
Cite this article
Rolle, T., Tofani, F., Brogliatti, B. et al. The effects of dorzolamide 2% and dorzolamide/timolol fixed combination on retinal and optic nerve head blood flow in primary open-angle glaucoma patients. Eye 22, 1172–1179 (2008). https://doi.org/10.1038/sj.eye.6703071
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6703071