Abstract
This prospective, observer-masked, randomized clinical trial was conducted between December 2018 and June 2021 at Eye Hospital, China Academy of Chinese Medical Sciences. A total of 45 glaucoma patients from Beijing, China, were enrolled in this clinical trial to compare the short-term efficacy of primary single-selective laser trabeculoplasty (SLT) to 0.005% latanoprost eye drops for the treatment of 24-h intraocular pressure (IOP) in patients with newly diagnosed primary open angle glaucoma (POAG) and ocular hypertension (OHT). Both SLT and latanoprost significantly decreased mean 24-h IOP and peak IOP, although the latanoprost group effect was more potent when compared to the SLT group (both Ps < 0.05). Compared with the SLT group, the latanoprost group had a significant and stable decrease in IOP after treatment. The latanoprost group had a more pronounced reduction in IOP at weeks 4 and 12 (P < 0.05) but had no difference at week 1 (P = 0.097). As a first-line treatment, both SLT and latanoprost eye drops are effective in newly diagnosed POAG and OHT patients. However, the latanoprost eye drops may be better in decreasing mean and peak 24-h IOP and thus controlling 24-h IOP fluctuation compared to SLT.
Similar content being viewed by others
Introduction
Glaucoma is the most common cause of irreversible blindness and the second most common cause of irreversible moderate and severe vision impairment worldwide1. Primary open-angle glaucoma (POAG) is the most common type, with a prevalence of 0.5–3.9% in Asia2. In China, there were 13.12 million people with glaucoma in 2015 (accounting for 2.58% of the total Chinese population), and the number is expected to increase to 25.16 million by 20503. Intraocular pressure (IOP) is the only modifiable risk factor for glaucoma onset and progression. IOP normally has a circadian rhythm (varying through 24 h), and previous studies have suggested that elevated IOP4,5, peak IOP6,7, and IOP fluctuation8,9,10,11 are possibly more specific risk factors for glaucomatous development and progression.
The choice of initial IOP-reducing therapy is essential for affecting the long-term outcome of glaucoma treatment. Prostaglandin analogue (PGA) monotherapy is often utilized as an initial treatment choice for POAG and ocular hypertension (OHT) because it is the most effective class of IOP-lowering drugs12. Meanwhile, selective laser trabeculoplasty (SLT) of the trabecular meshwork (TM) has been recently recommended as a safe and effective first-line treatment for POAG or OHT patients because of comparable IOP reduction, less ocular side effects, and the advantage of a single treatment that may mitigate the need for life-long compliant drop use by the patient13,14,15. Recently, the British National Institute for Health and Care Excellence (NICE) updated guidelines recognizing SLT as a first-line treatment option for patients with newly diagnosed POAG or OHT. However, the majority of participants were Caucasian in those studies. Additionally, the general limitation of SLT research is that most SLT studies evaluate patients during office hours (less is known about 24-h and nighttime efficacy16). Only a few studies have directly compared the effects of SLT to PGA drops as initial glaucoma treatment17,18,19,20, and even less research has been done regarding a direct 24-h efficacy comparison21.
Therefore, in this study, we perform a prospective comparison between SLT and 0.005% latanoprost eye drops as first-line therapy in treatment-naïve POAG and OHT patients in a Chinese population. We hypothesize that primary 360° SLT will demonstrate a comparable 24-h IOP-lowering effect using latanoprost eye drops monotherapy as initial IOP-reducing therapy.
Methods
Study design
This single-center, prospective, randomized clinical trial was conducted between December 2018 and June 2021. All measurements (visual field, optic disc imaging, and IOP) were made by research team members masked to treatment allocation. Clinicians and patients were not masked in treatment allocation. Using a web-based system, we randomly assigned patients (1:1) to either SLT or 0.005% latanoprost as first-line treatment (www.sealedenvelope.com). This trial was approved by the ethical committees of the Eye Hospital, China Academy of Chinese Medical Sciences. All participants provided informed consent before study enrollment. The study was registered at www.chictr.org.cn (registration number ChiCTR2200056850) and complied with the principles outlined in the Declaration of Helsinki22.
Participants
Patients seen at the glaucoma department of the Eye Hospital, China Academy of Chinese Medical Sciences, were screened for eligibility. POAG was defined as angles open on the gonioscopy and optic disc or retinal nerve fiber layer (RNFL) structural abnormalities corresponding to visual field (VF) loss without secondary causes. OHT was defined as an IOP of more than 21 mm Hg without glaucomatous optic nerve structural and functional changes. POAG was classified as high-tension glaucoma (HTG) and normal-tension glaucoma (NTG). Both types exhibited open angles, but HTG was characterized by an IOP higher than 21 mm Hg without treatment, while NTG had an IOP lower than 21 mm Hg on multiple clinic visits or peak measurements before treatment23. Glaucoma severity stratification (mild, moderate, or severe) was determined using visual field mean deviation (VF MD) at baseline, according to Mills et al.24. The values of VF MD in mild, moderate, and severe POAG were more than − 6 decibels (dB), − 6 to − 12 dB, and lower than − 12 dB, respectively. Inclusion and exclusion criteria were adopted to improve diagnosis accuracy and reduce potential bias induced by confounding factors. Inclusion criteria included: (a) patients newly diagnosed with OHT, mild POAG, or moderate POAG; (b) VF MD better than − 12 dB in the study eye; (c) age ≥ 18 years; (d) no history of glaucoma medications use in either eye for ≥ four weeks; and (e) willingness to undergo SLT versus latanoprost eye drops treatment. Exclusion criteria included: (a) VF MD worse than − 12 dB in the study eye; (b) patients with narrow angles or secondary glaucoma; (c) those with very high IOP who need immediate treatment (IOP > 30 mm Hg, initially or after washout); (d) any ocular condition precluding visualization of the TM; (e) previous anterior segment surgery or glaucoma laser; and (f) pregnancy. When both of a patient's eyes met the inclusion and exclusion criteria, they were given either SLT or latanoprost therapy. However, only the data from the right eye was considered for analysis25.
Procedures
Ophthalmic and medical history were obtained in all patients. Visual acuity testing, IOP measurements over 24 h, automated VF testing [Humphrey Field Analyzer (Carl Zeiss Meditec, Inc., Dublin, CA, USA) SITA Standard 24-2], gonioscopy, slit lamp examination, optical coherence tomography (OCT), optic disc imaging (Model 5000, Carl Zeiss Meditec, Inc., Dublin, CA, USA), refractive error assessment, central corneal thickness (CCT) determination, and fundus imaging were acquired at baseline. To analyze the 24-h IOP curves, the patients were hospitalized in the morning (~ 9 am). IOP was acquired at 7:00, 10:00, 14:00, 18:00, 22:00, 2:00 and 5:00. At each time point, IOP was measured three times in the sitting position with a calibrated Goldmann applanation tonometer (GAT). The mean value was used for analysis in this study. For nocturnal IOP measurements, patients were gently awakened and asked to walk 5–30 m for the examination. One certified ophthalmic technician (W.W.), masked to the treatment regimens, performed all IOP measurements using the same tonometer on each patient at all visits. Eye-specific target IOP was set for each subject based on a percentage reduction from the untreated baseline IOP and an absolute threshold according to the Asia Pacific Glaucoma Guidelines26 and the Canadian Target IOP Workshop27. The target IOP was set as follows: IOP reduction of more than 20% from baseline and a value less than 25 mm Hg for OHT; IOP reduction of more than 20% from baseline and a value less than 21 mm Hg for mild POAG; IOP reduction more than 30% from baseline and a value less than 18 mm Hg for moderate POAG. The TM pigmentation was graded: 0 = none, 1 = light, 2 = medium, 3 = dark brown, and 4 = almost black based on the Scheie's system of grading angle pigmentation28. After completing the baseline assessment and enrollment, participants were randomized 1:1 to the SLT treatment arm or the latanoprost treatment arm. The SLT group received a single standardized SLT treatment via a frequency-doubled Q-switched Nd: YAG laser (Ellex Medical Lasers Ltd, Adelaide, Australia) with a spot size of 400 microns and a 3-ns pulse duration. The laser energy started at 0.6 mJ and increased by 0.1 mJ until “champagne bubbles” were observed. Approximately 100 non-overlapping laser spots (25 per quadrant) were applied to cover 360° of the TM using a Latina SLT Gonio laser lens with a methylcellulose coupling agent by a single glaucoma specialist (X.X.). Following the SLT procedure, patients were not prescribed non-steroidal anti-inflammatory drugs or steroid therapy during their subsequent visits. Any complications that resulted from SLT treatment, such as inflammation and IOP spikes, were documented. An increase of more than 2 mm Hg above the average IOP values prior to treatment was considered as an IOP spike, as recorded one hour after the SLT procedure29. The latanoprost group received 0.005% latanoprost eye drops (Xalatan, Pfizer, New York, USA) once daily (every evening at 9 pm). Follow-up evaluations were performed on weeks 1, 4, and 12 post-laser or after the first latanoprost dose. 24-h IOP acquisition was performed at each visit using the same methods as at baseline. At each visit, patients were asked to report any adverse reactions to the treatment, the vision was measured, and slit lamp examination was performed. At 12 weeks, patients also underwent VF testing, optic nerve OCT, and fundus imaging. If the target IOP was not reached, a stepped regime of increasing topical medications was followed, including the addition of beta-adrenergic antagonists, carbonic anhydrase inhibitors, or alpha agonists.
Outcomes
The main outcomes used to evaluate the effects of controlling 24-h IOP were: (a) mean 24-h IOP (the average IOP over the entire 24-h period for each visit) at baseline and 1, 4 and 12 weeks after treatment initiation; (b) peak IOP (the highest IOP over the entire 24-h period for each visit) at baseline and 1, 4, and 12 weeks after treatment initiation. (c) 24-h IOP fluctuation (the peak IOP minus the trough IOP over the entire 24-h period for each visit) at baseline and 1, 4, and 12 weeks after treatment initiation. (d) IOP reduction from baseline at 1, 4, and 12 weeks after treatment initiation, including 24-h reduction (the post-treatment mean 24-h IOP at each follow-up time point minus the baseline mean 24-h IOP), diurnal reduction (the post-treatment mean IOP at 7:00, 10:00, 14:00, and 18:00 for each visit minus the baseline mean IOP at the same times), and nocturnal reduction (the post-treatment mean IOP at 22:00, 2:00, and 5:00 for each visit minus the baseline mean IOP at the same times).
Statistical analysis
All statistical analyses were performed using SPSS (SPSS for Windows, V. 26.0). Parameters with the data that followed a normal distribution were presented as standard ± deviation. Parameters with a skewed distribution of their data were presented as median and quartiles. The data with normal distribution were examined using the Shapiro–Wilk’s W test. Parameters of uncorrected visual acuity (UCVA), best-corrected visual acuity (BCVA), CCT, vertical cup-to-disc ratio, refractive error, RNFL thickness, disc area, VF MD, or VF pattern standard deviation (PSD) had skewed distributed, so a nonparametric Mann–Whitney test was used to compare these parameters. Pearson's chi-squared test was used to analyze categorical variables such as gender and TM pigmental grading. 24-h IOP characteristics (mean, peak, and fluctuation of IOP) obtained at diagnosis and different follow-up times were analyzed using a 2-way repeated-measures analysis of variance (ANOVA) with a group (SLT group and PGA group) as a between-subjects factor and different follow-up times as within-subjects factor. Greenhouse Geisser correction was applied whenever the sphericity assumption was violated. Multivariate analysis of variance process and Bonferroni correction for multiple comparisons were used to detect significant differences between groups and different measurement times for each group. A p-value of < 0.05 was considered statistically significant.
Results
A total of 45 patients (45 eyes) were enrolled. 23 patients (23 eyes) were included in the SLT group, and 22 patients (22 eyes) were in the latanoprost group (Fig. 1). All participants were Han Chinese living in Beijing, China. At 12 weeks, 40 (88.9%) patients (40 eyes) completed follow-up, and 5 (11.1%) patients (5 eyes) dropped out. There were no significant differences in age, sex, UCVA, BCVA, diagnosis, TM pigment grading, CCT, refractive error, RNFL thickness, VF MD, and VF PSD between the two groups at baseline (Table 1). The cup-to-disc ratio measured by OCT of the latanoprost group was greater than that of the SLT group (P = 0.023).
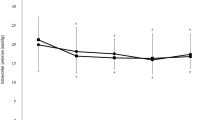
Both SLT and latanoprost eye drops therapy significantly decreased IOP at 7:00, 10:00, 14:00, 18:00, 22:00, 2:00, and 5:00 (all Ps < 0.05) when compared the baseline with the final follow-up visit (Fig. 2). Overall, there was a significant IOP reduction from baseline at each follow-up visit for each treatment group (both Ps < 0.001). For the SLT group, the 24-h IOP reduction at weeks 1, 4, and 12 were 4.0 ± 2.8 mmHg (18.5% ± 10.4%), 2.4 ± 2.3 mmHg (11.0% ± 8.9%), and 3.2 ± 2.4 mmHg (14.3% ± 9.5%), respectively. For the latanoprost group, IOP reduction for the same periods were 5.5 ± 2.7 mmHg (24.7% ± 9.8%), 5.1 ± 2.5 mmHg (23.1% ± 9.3%), and 5.5 ± 2.0 mmHg (25.9% ± 6.8%), respectively. Therefore, IOP reduction for the latanoprost group was significantly higher than that for the SLT group at weeks 4 and 12 (P = 0.001 and P = 0.002, respectively), but not at week 1 (P = 0.097). The diurnal and nocturnal IOP reduction for the latanoprost group was also significantly higher than that for the SLT group at weeks 4 and 12 (all Ps < 0.05), but not at week 1 (both Ps > 0.05). At weeks 12, the IOP reduction was greater in the nocturnal periods than in the diurnal periods in the latanoprost group (6.6 ± 2.8 mmHg vs. 4.9 ± 2.2 mmHg, P = 0.028). In contrast, the IOP reduction was similar in the nocturnal and diurnal in the SLT group (3.2 ± 2.6 mmHg vs. 3.2 ± 3.0 mmHg, P = 0.952) (Table 2, Fig. 2).
Profiles of 24-h IOP at baseline and after 12 weeks in the SLT and latanoprost groups. Measurements were taken from 21 in the SLT group (A) and 19 in the latanoprost group (B) in the seated position during the diurnal and nocturnal periods. Error bars represent the standard error of the mean. *Indicated a statistically significant difference between the baseline and week 12 (P < 0.05). IOP, intraocular pressure; SLT, selective laser trabeculoplasty.
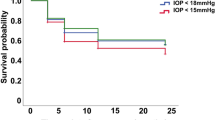
For mean 24-h IOP, the baseline values were comparable between the SLT and the latanoprost groups (P = 0.668). Comparing the mean 24-h IOP between each of the follow-up visits to baseline, IOP significantly dropped at weeks 1, 4, and 12 for the SLT (all Ps < 0.001) and the latanoprost (all Ps < 0.001) groups. Comparing the mean 24-h IOP values between the SLT and latanoprost groups at each follow-up visit, the mean IOP was not significantly different at week 1 (P = 0.361), but the mean IOP was lower in the latanoprost group compared to the SLT group at weeks 4 and 12 (P = 0.043, and 0.026, respectively) (Table 3 and Fig. 3A).
24-h IOP characteristics (mean, peak, and fluctuation of IOP) at baseline and 12-week follow-up visits. (A) 24-h mean IOP over time. (B) Peak IOP over time. (C) 24-h IOP fluctuation over time. *Indicated a significant difference when compared the SLT group with the latanoprost group (P < 0.05). IOP, intraocular pressure; SLT, selective laser trabeculoplasty.
The baseline peak IOP occurred at 2:00 in the SLT and the latanoprost groups, and the values were comparable between the two groups (P = 0.299). Compared to peak IOP at baseline, the peak IOP was significantly lower at weeks 1, 4, and 12 after treatment initiation for the SLT (all Ps < 0.001) and the latanoprost (all Ps < 0.001) groups. The latanoprost was significantly more effective than SLT at lowering peak IOP at weeks 4 and 12 (P = 0.037 and 0.020, respectively) (Table 3 and Fig. 3B).
At baseline, the 24-h IOP fluctuation was comparable between the SLT and latanoprost groups (P = 0.299). In the SLT group, even though 24-h IOP fluctuation showed a significant reduction from baseline at post-treatment week 1(P < 0.001), the value was not significantly different at weeks 4 and 12(P = 0.206 and 0.416, respectively) from baseline. In contrast, in the latanoprost group, 24-h IOP fluctuation showed a sustained reduction through the 12-week follow-up. The values at weeks 1, 4, and 12 were lower than the baseline (P = 0.024, 0.023, and 0.023, respectively). Comparing 24-h IOP fluctuation between the two groups at each follow-up visit, the values were not significantly different at week 1 (P = 0.804), but significantly lower in the latanoprost group compared to the SLT group at weeks 4 and 12 (P = 0.042, and 0.004, respectively) (Table 3 and Fig. 3C). At weeks 12, the nocturnal IOP fluctuation in the latanoprost group was lower than in the SLT group (2.8 ± 2.5 mmHg vs. 5.9 ± 2.7 mmHg, P = 0.001). In contrast, the diurnal IOP fluctuation was similar between the two groups (3.7 ± 1.5 mmHg vs. 3.7 ± 1.7 mmHg, P = 0.619).
To investigate the effectiveness of SLT and latanoprost on NTG and HTG patients, we excluded a total of 8 OHT subjects (6 from the SLT group and 2 from the latanoprost group). We then categorized POAG patients into subgroups based on HTG and NTG in each treatment group. Afterward, we compared the 24-h IOP parameters of both groups before and after interventions.
Patients with NTG experienced a significant reduction in mean 24-h IOP at all follow-up points compared to the baseline in the latanoprost group (all Ps < 0.05). Meanwhile, in the SLT group, the mean 24-h IOP significantly decreased at weeks 1 and 4 (both Ps < 0.05), but the value at weeks 12 did not differ significantly from the baseline (P > 0.05). During various visits, there was no significant difference between groups in weeks 1 and 4 (P = 0.370 and P = 0.095, respectively). However, by weeks 12, the mean IOP in the latanoprost group was significantly lower compared to the SLT group (P = 0.011). During the follow-up visits, it was observed that the peak value of 24-h IOP decreased significantly in the latanoprost group after treatment initiation (all Ps < 0.05). However, there was no significant decrease in the peak value in the SLT group (all Ps > 0.05). By the end of the follow-up visits, it was noted that the peak value in the latanoprost group was significantly lower than the SLT group (P = 0.022). There was no significant difference in the 24-h IOP fluctuation between the baseline and all subsequent visits after treatment initiation in both groups (all Ps > 0.05) (Supplemental Table 1).
HTG patients experienced a notable decrease in both mean 24-h IOP and peak IOP after undergoing SLT and latanoprost treatments, with statistical significance noted at all follow-up points (all Ps < 0.05). During weeks 1, 4, and 12, the latanoprost group showed a remarkable decrease in 24-h IOP fluctuation (all Ps < 0.05). On the other hand, the SLT group did not exhibit any significant change in 24-h IOP fluctuation compared to baseline at weeks 4 and 12 (both Ps > 0.05). At all time points, there were no notable differences in any variables of 24-h IOP between the two groups (all Ps > 0.05) (Supplemental Table 2).
Following the SLT treatment, there were no significant complications reported. Of the 23 participants, 8 (34.8%) experienced minor inflammation (1 + cells) within an hour of the treatment, but none of these cases sustained inflammation during the follow-up. Four patients (17.4%) had IOP spikes, with an increase in IOP ranging from 2.4 to 5.5 mmHg. Three patients in each group received additional topical IOP-lowering drops after four weeks. One SLT case did not achieve the target IOP after adding anti-glaucomatous drugs and underwent trabeculectomy.
Due to the absence of RNFL thickness thinning and VF defect, all of the 8 OHT patients (6 in the SLT group and 2 in the latanoprost group) were excluded when analyzing the changes of RNFL thickness, VF MD, and VF PSD before and after treatment in the two groups. There were 32 POAG patients remaining, with 15 in the SLT group and 17 in the latanoprost group. After treatment, no significant changes were observed in these three parameters for both groups (all Ps > 0.05) (Table 4).
Discussion
In this randomized controlled trial, we compared the short-term efficacy of primary single SLT with 0.005% latanoprost eye drops monotherapy for controlling 24-h IOP in treatment-naïve POAG and OHT. We demonstrated that both SLT and latanoprost eye drops significantly improved 24-h IOP control, including mean, peak, and 24-h fluctuation of IOP. However, latanoprost was more effective. In addition, the nocturnal IOP-lowering efficacy of the latanoprost eye drops was better than SLT during the 12-week follow-up.
The Laser in Glaucoma and Ocular Hypertension Trial (LiGHT) study compared IOP lowering 355 OHT or OAG patients (611 eyes) who received SLT with 362 OHT or OAG patients (622 eyes) who received topical medication for two months30. No difference was found between topical medication and primary SLT (adjusted mean difference = − 0.1 mmHg). In this study, SLT was less effective, and this may be due to the use of different anti-glaucoma medications as well as racial differences. Additionally, single IOP measurements were used in the LiGHT study, but 24-h IOP data was collected in the current study. We point out that single IOP measurements during office hours are insufficient to analyze the actual IOP pathology of a glaucoma patient. Many patients experience peak IOP outside of clinic hours, and peak IOPs occur at nighttime31.
Long-term IOP fluctuation is associated with VF progression8. Elevated nocturnal IOP may have a stronger impact on retinal ganglion cell loss than elevated diurnal IOP32. Our results showed that SLT reduced the amplitude of 24-h IOP fluctuation, but the effect lasted only one week. In contrast, the latanoprost eye drops flattened the circadian IOP curve for the 12-week follow-up period, lowering the nocturnal peak IOP better than SLT. Our results were consistent with previous studies, which showed that PGA produced stable 24-h IOP reduction33,34. So far, the relationship between SLT and IOP fluctuation is unclear. Lee et al.35 found that 24-h IOP fluctuation was significantly reduced in 18 normal tension glaucoma (NTG) patients using a contact lens sensor (CLS) IOP monitor. In contrast, Tojo and colleagues36 reported that the 24-h IOP fluctuation did not significantly change in 10 NTG patients treated with 360° SLT using a CLS monitoring, although nocturnal IOP fluctuation significantly decreased. Aptel et al.37 found that SLT did not affect the 24-h IOP pattern for 14 patients with POAG. Our data showed that the effect of SLT on circadian IOP fluctuation control lasted only one week. Post-SLT, at 4 and 12 weeks, the fluctuation amplitude returned to the level before treatment, and the nocturnal peak IOP control was lost. The explanation might be that the IOP-lowering effect of SLT fades over time38.
Nagar et al.20 compared the effect of 360° SLT with latanoprost on diurnal IOP in 40 patients with OAG and OHT. They found that latanoprost was more likely to diminish diurnal IOP fluctuation. However, they didn’t collect patients’ nocturnal IOP data. Kiddee et al.21 compared the effect of 360° SLT with travoprost in 58 patients with POAG and NTG during the daytime and the nighttime. They found that the lowing-IOP effect of travoprost on IOP reduction in POAG and NTG patients was significant both during the daytime and the nighttime, while the SLT's lowing-IOP effect was significant only during the nighttime rather than daytime. Our data suggested that latanoprost is more effective than SLT in controlling 24-h IOP fluctuation probably due to the attenuation effect of SLT, which is consistent with the results of previous studies20,21. However, it was important to note that Nagar’s study20 only monitored IOP during the daytime, and Kiddee’s study21 was followed for only 8 weeks. During our study, we monitored IOP both during the day and night, and tracked the results over a period of 12 weeks.
In Chinese patients with POAG, the percentage of those with NTG ranges from 51.43 to 83.58%39. When comparing the effectiveness of treatments in NTG patients (6 in the SLT group and 5 in the latanoprost group), the results showed that primary 0.005% latanoprost eye drops might be more effective in reducing the mean and peak value of 24-h IOP in NTG patients compared to single SLT. This finding might be valuable in guiding clinical practice for newly diagnosed NTG patients as it suggests that latanoprost may provide a more lasting and stable treatment option.
This study also had some limitations that warrant discussion. First, GAT measurement in the sitting position was utilized at all time points during the 24-h IOP evaluation. This may fail to represent an individual’s actual IOP variation because people usually slept lying down. Interestingly, even though lying down or taking a head-down tilt position was known to impact IOP40, previous studies reported that IOP was still elevated in the supine posture compared to sitting while sleeping at night41,42,43. The subjects were also awoken for IOP measurements at night, so the normal sleep–wake cycle was interrupted. Changes in diurnal physiology and hormonal levels may also influence IOP results16. Finally, this was a single-center study with relatively small sample size and short-term follow-up.
Conclusion
In conclusion, as a first-line treatment, both SLT and latanoprost eye drops are effective in newly diagnosed POAG and OHT patients. The latanoprost eye drops may be better in decreasing mean and peak 24-h IOP and controlling 24-h IOP fluctuation compared to SLT.
Data availability
The data used and/or analyzed during this study are available from the corresponding author on reasonable request.
References
GBD 2019 Blindness and Vision Impairment Collaborators and Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob. Health. 9, e144–e160. https://doi.org/10.1016/S2214-109X(20)30489-7 (2021).
Cho, H. K. & Kee, C. Population-based glaucoma prevalence studies in Asians. Surv Ophthalmol. 59, 434–447. https://doi.org/10.1016/j.survophthal.2013.09.003 (2014).
Song, P. et al. National and subnational prevalence and burden of glaucoma in China: A systematic analysis. J Glob Health. 7, 020705. https://doi.org/10.7189/jogh.07.020705 (2017).
Lichter, P. R. et al. Interim clinical outcomes in the Collaborative Initial Glaucoma Treatment Study comparing initial treatment randomized to medications or surgery. Ophthalmology 108, 1943–1953. https://doi.org/10.1016/s0161-6420(01)00873-9 (2001).
Leske, M. C. et al. Factors for glaucoma progression and the effect of treatment: the early manifest glaucoma trial. Arch. Ophthalmol. 121, 48–56. https://doi.org/10.1001/archopht.121.1.48 (2003).
Fogagnolo, P. et al. Short- and long-term phasing of intraocular pressure in stable and progressive glaucoma. Ophthalmologica 230, 87–92. https://doi.org/10.1159/000351647 (2013).
Konstas, A. G. et al. Peak intraocular pressure and glaucomatous progression in primary open-angle glaucoma. J. Ocul. Pharmacol. Ther. 28, 26–32. https://doi.org/10.1089/jop.2011.0081 (2012).
Joseph, C. & Coleman, A. L. Intraocular pressure fluctuation a risk factor for visual field progression at low intraocular pressures in the advanced glaucoma intervention study. Ophthalmology 115, 1123-1129.e1123. https://doi.org/10.1016/j.ophtha.2007.10.031 (2008).
Becker, B. Large diurnal fluctuations in intraocular pressure are an independent risk factor in patients with glaucoma. J. Glaucoma. 9, 487–488 (2000).
Nouri-Mahdavi, K. et al. Predictive factors for glaucomatous visual field progression in the Advanced Glaucoma Intervention Study. Ophthalmology 111, 1627–1635. https://doi.org/10.1016/j.ophtha.2004.02.017 (2004).
Guo, Z. Z., Chang, K. & Wei, X. Intraocular pressure fluctuation and the risk of glaucomatous damage deterioration: A meta-analysis. Int. J. Ophthalmol. 12, 123–128. https://doi.org/10.18240/ijo.2019.01.19 (2019).
European Glaucoma Society Terminology and Guidelines for Glaucoma, 5th Edition. Br. J. Ophthalmol. 105, 1–169. https://doi.org/10.1136/bjophthalmol-2021-egsguidelines (2021).
Gazzard, G. et al. Selective laser trabeculoplasty versus eye drops for first-line treatment of ocular hypertension and glaucoma (LiGHT): A multicentre randomised controlled trial. Lancet 393, 1505–1516. https://doi.org/10.1016/S0140-6736(18)32213-X (2019).
Liu, Y., Fan, X. & Wu, L. Selective laser trabeculoplasty lowered the untreated fellow eye long-term intraocular pressure: A 3-year observational study. Lasers Med. Sci. 37, 1487–1493. https://doi.org/10.1007/s10103-021-03253-w (2022).
Gazzard, G. et al. Selective laser trabeculoplasty versus drops for newly diagnosed ocular hypertension and glaucoma: the LiGHT RCT. Health Technol. Assess. 23, 1–102. https://doi.org/10.3310/hta23310 (2019).
Mansouri, K., Tanna, A. P., De Moraes, C. G., Camp, A. S. & Weinreb, R. N. Review of the measurement and management of 24-hour intraocular pressure in patients with glaucoma. Surv. Ophthalmol. 65, 171–186. https://doi.org/10.1016/j.survophthal.2019.09.004 (2020).
Nagar, M., Ogunyomade, A., O’Brart, D. P., Howes, F. & Marshall, J. A randomised, prospective study comparing selective laser trabeculoplasty with latanoprost for the control of intraocular pressure in ocular hypertension and open angle glaucoma. Br. J. Ophthalmol. 89, 1413–1417. https://doi.org/10.1136/bjo.2004.052795 (2005).
Mcilraith, I., Strasfeld, M., Coley, G. & Hutnik, C. M. L. Selective laser trabeculoplasty as initial and adjunctive treatment for open-angle glaucoma. J. Glaucoma. 142, 364–364. https://doi.org/10.1097/00061198-200604000-00009 (2006).
Katz, L. J. et al. Selective laser trabeculoplasty versus medical therapy as initial treatment of glaucoma: A prospective, randomized trial. J. Glaucoma. 21, 460–468. https://doi.org/10.1097/IJG.0b013e318218287f (2012).
Nagar, M., Luhishi, E. & Shah, N. Intraocular pressure control and fluctuation: The effect of treatment with selective laser trabeculoplasty. Br. J. Ophthalmol. 93, 497–501. https://doi.org/10.1136/bjo.2008.148510 (2009).
Kiddee, W. & Atthavuttisilp, S. The effects of selective laser trabeculoplasty and travoprost on circadian intraocular pressure fluctuations: A randomized clinical trial. Medicine Baltimore 96, e6047. https://doi.org/10.1097/MD.0000000000006047 (2017).
World Medical, A. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 310, 2191–2194. https://doi.org/10.1001/jama.2013.281053 (2013).
Ganeshrao, S. B., Senthil, S., Choudhari, N., Durgam, S. S. & Garudadri, C. S. Comparison of visual field progression rates among the high tension glaucoma, primary angle closure glaucoma, and normal tension glaucoma. Investig. Opthalmol. Vis. Sci. 60, 889–900. https://doi.org/10.1167/iovs.18-25421 (2019).
Mills, R. P. et al. Categorizing the stage of glaucoma from pre-diagnosis to end-stage disease. Am. J. Ophthalmol. 141, 24–30. https://doi.org/10.1016/j.ajo.2005.07.044 (2006).
Ray, W. A. & Oday, D. M. Statistical analysis of multi-eye data in ophthalmic research. Investig. Ophthalmol. Vis. Sci. 26, 1186–1188 (1985).
Society, A.-P. G. Asia Pacific Glaucoma Guidelines 3rd edn. (Kugler Publications, Amsterdam, 2016).
Damji, K. F., Behki, R., Wang, L. & Target, I. O. P. W. P. Canadian perspectives in glaucoma management: setting target intraocular pressure range. Can. J. Ophthalmol. 38, 189–197. https://doi.org/10.1016/s0008-4182(03)80060-1 (2003).
Kent, S. S. et al. A randomized clinical trial of selective laser trabeculoplasty versus argon laser trabeculoplasty in patients with pseudoexfoliation. J. Glaucoma 24, 344–347. https://doi.org/10.1097/ijg.0b013e31829e55e4 (2015).
McIlraith, I., Strasfeld, M., Colev, G. & Hutnik, C. M. Selective laser trabeculoplasty as initial and adjunctive treatment for open-angle glaucoma. J. Glaucoma 15, 124–130. https://doi.org/10.1097/00061198-200604000-00009 (2006).
Garg, A. et al. Primary selective laser trabeculoplasty for open-angle glaucoma and ocular hypertension: clinical outcomes, predictors of success, and safety from the laser in glaucoma and ocular hypertension trial. Ophthalmology 126, 1238–1248. https://doi.org/10.1016/j.ophtha.2019.04.012 (2019).
Cheng, J., Kong, X., Xiao, M. & Sun, X. Twenty-four-hour pattern of intra-ocular pressure in untreated patients with primary open-angle glaucoma. Acta Ophthalmol. 94, e460-467. https://doi.org/10.1111/aos.12963 (2016).
Kwong, J. M. et al. The dark phase intraocular pressure elevation and retinal ganglion cell degeneration in a rat model of experimental glaucoma. Exp. Eye Res. 112, 21–28. https://doi.org/10.1016/j.exer.2013.04.008 (2013).
Mansouri, K., Medeiros, F. A. & Weinreb, R. N. Effect of glaucoma medications on 24-hour intraocular pressure-related patterns using a contact lens sensor. J Clin. Exp. Ophthalmol. https://doi.org/10.1111/ceo.12567 (2015).
Dya, B., Jhkl, A., Nw, B. & Rnw, A. Correlation between office-hour and peak nocturnal intraocular pressure in patients treated with prostaglandin analogs. Am. J. Ophthalmol. 215, 112–117. https://doi.org/10.1016/j.ajo.2020.02.010 (2020).
Lee, J. W. Y., Fu, L., Chan, J. C. H. & Lai, J. S. M. Twenty-four-hour intraocular pressure related changes following adjuvant selective laser trabeculoplasty for normal tension glaucoma. Medicine (Baltimore) 93, e238. https://doi.org/10.1097/MD.0000000000000238 (2014).
Tojo, N., Oka, M., Miyakoshi, A., Ozaki, H. & Hayashi, A. Comparison of fluctuations of intraocular pressure before and after selective laser trabeculoplasty in normal-tension glaucoma patients. J. Glaucoma. 23, e138-143. https://doi.org/10.1097/IJG.0000000000000026 (2013).
Aptel, F., Musson, C., Zhou, T., Lesoin, A. & Chiquet, C. 24-Hour intraocular pressure rhythm in patients with untreated primary open angle glaucoma and effects of selective laser trabeculoplasty. J. Glaucoma. 26, 272–277. https://doi.org/10.1097/IJG.0000000000000604 (2017).
Garg, A. & Gazzard, G. Selective laser trabeculoplasty: Past, present, and future. Eye (Lond). 32, 863–876. https://doi.org/10.1038/eye.2017.273 (2018).
Zhao, J. et al. Prevalence of normal-tension glaucoma in the chinese population: A systematic review and meta-analysis. Am. J. Ophthalmol. 199, 101–110. https://doi.org/10.1016/j.ajo.2018.10.017 (2019).
Balasubramanian, S. et al. Thigh cuffs as a countermeasure for ocular changes in simulated weightlessness. J. Ophthalmol. S0161642017329834. https://doi.org/10.1016/j.ophtha.2017.10.023 (2017).
Lee, Y. R. et al. Circadian (24-hour) pattern of intraocular pressure and visual field damage in eyes with normal-tension glaucoma. Investig. Ophthalmol. Vis. Sci. 53, 881–887. https://doi.org/10.1167/iovs.11-7846 (2012).
Kiuchi, T., Motoyama, Y. & Oshika, T. Relationship of progression of visual field damage to postural changes in intraocular pressure in patients with normal-tension glaucoma. Ophthalmology 113, 2150–2155. https://doi.org/10.1016/j.ophtha.2006.06.014 (2006).
Mansouri, K., Weinreb, R. N. & Liu, J. H. K. Effects of aging on 24-hour intraocular pressure measurements in sitting and supine body positions. Investig. Ophthalmol. Vis. Sci. 53(1), 112–116. https://doi.org/10.1167/iovs.11-8763 (2012).
Funding
The research was supported by the Capital Characteristic Clinical Project of Beijing Municipal Science and Technology Commission (Z18110000171808[XX]); National Institutes of Health, Bethesda, MD (R01EY030501 [ASH]); an unrestricted grant from Research to Prevent Blindness (New York, NY) [UCSD]; Construction Project of Famous Traditional Chinese Medicine Expert Experiences (Like Xie) Inheritance Studio, Shijingshan District, Beijing ([2020] No. 5[LX]); and the Research Grants Program of Eye Hospital, China Academy of Chinese Medical Sciences (201516[XX]).
Author information
Authors and Affiliations
Contributions
X.X. and L.X. designed the study. W.S., S.C. and W.W. collected all data. Y.Z. and L.Z. analysed and interpreted the data. Y.S. wrote the first draft of the paper. X.X. and A.S.H. revised the work. Y.S., Y.Z., and W.S. are co-first authors. All authors approved the final version of the manuscript. Y.S. and X.X. had full access to all data and takes responsibility for data integrity and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shi, Y., Zhang, Y., Sun, W. et al. 24-Hour efficacy of single primary selective laser trabeculoplasty versus latanoprost eye drops for Naïve primary open-angle glaucoma and ocular hypertension patients. Sci Rep 13, 12179 (2023). https://doi.org/10.1038/s41598-023-38550-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-38550-7
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.