Abstract
Design
This was a randomised controlled trial.
Intervention
Ozone treatment was delivered by HealOzone machines, one delivering air (control) and the other ozone (test), prepared and coded by the manufacturer (HealOzone; KaVo, Biberach, Germany).
Outcome measure
Pain in response to a tactile stimulus or desiccation was assessed using a 100-mm visual analogue scale (VAS). Also, the global subject's perception of sensitivity was assessed at each visit by using a VAS.
Results
No subjects reported an increase in pain or any adverse effect. All subjects reported a clinically significant reduction in pain, relative to baseline, at each followup visit. The difference between the study groups was not statistically significant, however.
Conclusions
Treatment of hypersensitive teeth with ozone reduces the pain sensation, but this effect cannot be distinguished from the placebo treatment. There was a large placebo effect that narrowed the range over which treatment differences might be detected.
Similar content being viewed by others
Commentary
Dentine hypersensitivity (DH) is defined as, “short, sharp pain arising from exposed dentine in response to stimuli typically thermal, evaporative, tactile, osmotic or chemical and which cannot be ascribed to any other form of dental defect or pathology”.1 Ozone gas or trioxygen is a triatomic molecule consisting of three oxygen atoms (O3). Ozone is a potent microbicide and has been used in dentistry to treat dental caries by killing bacteria in carious lesions instead of restoration (drilling and filling), but the reliability of the evidence has been questioned.2, 3
The study gives a thorough explanation of dentine hypersensitivity, but no information was given about ozone or how it might affect DH. This trial aims to find out if two applications of ozone would reduce DH by 20%.
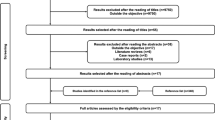
The authors carried out a power calculation based on a 20% difference with a P value set at 0.05. It was sensible to screen 30% more patients in the trial to accommodate any loss resulting from patients not fulfilling all inclusion criteria. Randomisation was robust, although the allocation process was not clearly described. Inclusion and exclusion criteria were checked for all patients during screening, but there was no mention of how long patients had been suffering from DH, even though this could affect response to treatment.
Of 43 recruited patients, 35 completed the trial (20 in the test group and 15 in the control group). The number of teeth tested in the test and control groups were 56 and 35 teeth, respectively. The main outcome was the level of pain after tactile and desiccation stimuli on exposed dentine, assessed using a VAS. Patients also evaluated their dentine sensitivity experience between visits using VAS. The authors used the terms desiccation, and thermal and air stimuli interchangeably: it would have been more accurate to use the term evaporative stimulus.
The results showed a reduction in dentine hypersensitivity in both test and control groups, but the difference between the two groups was not statistically significant. The authors reported that, in both groups, there was a clinically significant reduction in pain at each followup visit. How this clinical significant was derived was not clearly explained.
The problem with averaging values between patients in each group for every test is that it hides individual improvements. Alternatively, data could have been presented on the basis of patients who showed or did not show improvement, as this would be more meaningful for patients. In the case of patients who had more than one tooth included, it was not clear if each tooth was tested individually and data were averaged, or teeth were all tested then patients reported their pain level. 95% confidence intervals and P values were reported.
In conclusion, the findings of this well conducted trial are not unsurprising for while ozone is able to kill bacteria it does not block dentinal tubules which is a key therapeutic aim for DH.
References
Holland GR, Narhi MN, Addy M, Gangarosa L, Orchardson R. Guidelines for the design and conduct of clinical trials on dentine hypersensitivity. J Clin Periodontol 1997; 24: 808–813.
Rickard GD, Richardson RJ, Johnson TM, McColl DC, Hooper L. Ozone therapy for the treatment of dental caries. Cochrane Database Syst Rev 2004; issue 3.
National Institute of Clinical Excellence. Tooth Decay – Healozone. HealOzone for the Treatment of Tooth Decay (Occlusal Pit and Fissure Caries and Root Caries). London: National Institute of Clinical Excellence; 2005: Technology Appraisal AT92.
Author information
Authors and Affiliations
Additional information
Address for correspondence: Dr Amir Azarpazhooh, Department of Endodontics and Community Dentistry Health Services Research Unit, room #521A, Faculty of Dentistry, University of Toronto, 124 Edward Street, Toronto, Ontario, Canada M5G 1G6. E-mail: amir.azarpazhooh@dentistry.utoronto.ca
Azarpazhooh A, Limeback H, Lawrence HP, Fillery ED. Evaluating the effect of an ozone delivery system on the reversal of dentin hypersensitivity: a randomized, double-blinded clinical trial. J Endod 2009; 35: 1–9
Rights and permissions
About this article
Cite this article
Elgalaid, T. Ozone treatment had no effect on tooth hypersensitivity. Evid Based Dent 11, 70 (2010). https://doi.org/10.1038/sj.ebd.6400732
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ebd.6400732