Abstract
Study design:
Case report and literature review.
Objective:
Intradural-extramedullary cavernoma is a rare condition with only 23 cases reported in the literature. Most cases described adhere to spinal root or spinal cord. We report an example of this rare entity located within the sheets of one cauda equina nerve root.
Setting:
Rome, Italy.
Methods:
The authors report clinical, radiological, surgical, and pathological features of intraroot cavernoma with a literature review.
Results:
Patient was operated. One year after surgery, he was healthy.
Conclusion:
Lumbar intradural cavernous angioma may present with sciatalgia, low-back pain, neurological deficit, or, more rarely with subarachnoid hemorrhage or hydrocephalus. They are treated successfully with surgical resection but preoperative status is a predicting factor for outcome. Sometimes the sacrifice of the spinal root is inevitable because, as in present case, the cavernous angioma is included in the nerve root. These lesions are rare and benign lesions. It is important for neurosurgeons to be aware of the existence of this entity to avoid preoperative misdiagnosis with tumor.
Similar content being viewed by others
Introduction
Central nervous system (CNS) cavernomas are rare vascular malformations consisting of closely packed large sinusoid-like vascular channels with little or no intervening nervous tissue. They can occur anywhere in the CNS, but they favor cerebral hemisphere.1, 2, 3, 4 In the spine, cavernomas are found far more frequently in the vertebral bodies and, when involve intradural space, they occur primarily within the spinal cord.5, 6, 7 Intradural-extramedullary location is very rare, with only 23 cases reported in the literature accessible to us by Medline Research.8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27
We describe a case of cavernoma located within the boundaries of a lumbar nervous root and we discuss its clinical, radiological, and surgical findings.
Case report
A 71-year-old man presented to our institution with low-back pain radiating into the left leg. The pain was exacerbated by the supine position.
On physical examination, the patient was found to have hypoesthesia in the left L4 dermatome and absence of the rotuleus reflex.
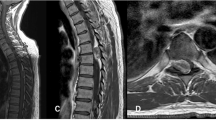
Lumbar MRI showed a left sided intradural-extramedullary nodular mass at the L3 level. The lesion appeared slightly hyperintense on T1- weighted images without contrast enhancement and hypointense on T2-weighted images (Figure 1a–c).
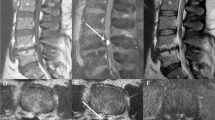
An L3 bilateral laminectomy was performed and the dura was opened under microscopic magnification. A reddish lesion was identified incorporated into one nerve root of the cauda equina (Figure 2a and b).
Histopathological examination revealed typical features of a cavernous angioma within the sheath of a spinal nerve and presence of nervous radicula peripherally to the vascular malformation (Figure 3a–d).
Thin-walled multiple vascular spaces of different diameter. H&E, 2.5 × (a). A large nerve appears at a margin of the lesion. H&E, 2.5 × (b). In the inset (c), a higher magnification of (b) evidences small nerve fibers compressed by hamartomatous vessels and the broader peripherical nervous component. H&E, 10 × . Staining of nerves by immunohistochemistry for protein S-100 in the same field shown in Figure 2. PAP method, 2.5 × (d). Higher magnification evidences nerve fibers outside the lesion and entrapped in the wall of hamartomatous vessels. PAP method, S-100 protein, 10 × (e)
The postoperative period was uneventful and the lumbosciatalgia resolved after operation. One year after surgery, the patient was healthy.
Discussion
Cavernous angioma has been described occurring throughout the entire CNS.1, 2, 3, 4, 6, 15 The most common location of these vascular malformations is the supratentorial cerebral parenchyma. Cauda equina nerve root is a very rare location.4, 9, 10, 11, 12, 13, 15, 16, 17, 18, 19, 21, 22, 23, 24, 25, 26 Pagni et al15 reviewed all intradural cavernous angioma of the spine described in the literature. They concluded that subdural extramedullary cavernous angiomas are the most rare of the cavernomas with only 10 cases documented between 1903 and 1990. Although these vascular malformations are being discovered most frequently because of the widespread use of MRI, they remain still uncommon lesions. A Medline search identified just 24 cases, including the present case (Table 1).8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27
The patients are in their third to seventh decades of life. The most common age at diagnosis is during the third decade. There is a male predominance (M:F ratio 2:1); and the lesions are mostly located in the lumbar region (13 cases – 54%), followed by lower thoracic (seven cases – 29%), cervical region (three cases – 12%), and thoraco-lumbar passage (one case – 4%). Low-back pain and radiculopathy are the main symptoms associated or not with motor deficit or neurologic symptoms secondary to spinal cord compression. However, 37% of patients developed a subarachnoid hemorrhage with acute onset of symptomatology. More rarely (12%), symptoms of intracranial hypertension caused by hydrocephalus have been found.
The preoperative radiological diagnosis of intraroot cavernous angioma is quite difficult, probably because of the rarity of this lesion.
Cavernous angiomas are lesions angiographycally occult, but are easily diagnosed by MRI. MRI is the imaging modality of choice.5, 29 The typical MRI features are those of a well-defined lesion with mixed signal intensity on both T1- and T2-weighted images. They are often surrounded by a hypointense ring on T2-weighted images owing to hemosiderin deposition.8 Enhancement with Gadolinium is variable.28 In the present case, we found no significant contrast enhancement in the cavernous angioma, probably because the intralesional blood flow was too low.
The treatment of choice is surgical removal. The most frequent surgical finding is that the lesion adheres to the nerve roots, dura, or spinal cord extending extraphytically.25 In the present case, cavernous angioma was within one spinal root. This finding was confirmed by histological examination that showed the disarrangement of radicles. A similar pattern of growth is reported only in another two cases.15, 26
Histologically, cavernous angioma must be distinguished from capillary hemangioma. Capillary hemangioma consists of a myriad of small vessels of capillary size. Cavernous angioma consists of large, dilated hyaline vascular channels arranged in diffuse patterns. They often show thrombosis, perivascular hemosiderin deposition, and calcifications.4, 29, 30
Most of the cases surgically treated had excellent results, but in patients with severe preoperative neurological deficits, such as sphincter dysfunction, recovery was not complete.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27 Total excision was obtained in most of the cases. Subtotal removal was performed only in one case in which the cavernoma tightly adhered to the spinal cord.24 In most cases, the lesion has been removed sparing the nerve root, but sometimes this is not possible because the lesion originates within the nerve root. This occurred in our case. However, our patient had a good recovery, even if it was necessary to cut the nerve root.
References
Duke BJ, Levy AS, Lillehei KO . Cavernous angiomas of the cauda equina: case report and review of the literature. Surg Neurol 1998; 50: 442–445.
Giombini S, Morello G . Cavernous angioma of the brain. Account of fourteen personal cases and review of the literature. Acta Neurochir (Wien) 1978; 40: 61–82.
Voight K, Yasargil MG . Cerebral cavernous haemangiomas or cavernomas: incidence, pathology, localization, diagnosis, clinical features and treatment. Review of the literature and report of an unusual case. Neurochir (Stuttg) 1976; 19: 59–68.
Nowak DA, Gumprecht H, Stolze A, Lumena Ch B . Intraneural growth of a capillary haemangioma of the cauda equina. Acta Neurochir (Wien) 2000; 142: 463–468.
Santoro A et al. Intramedullary spinal cord cavernous malformations: report of ten new cases. Neurosurg Rev 2004; 27: 93–98.
D’Andrea G, Ramundo OE, Trillò G, Roperto R, Isidori A, Ferrante L . Dorsal foramenal extraosseous epiduralcavernous hemangioma. Neurosurg Rev 2003; 26: 292–296.
Guthkelch AN . Haemangiomas involving spinal epidural space. J Neurol Neurosurg Psychiatry 1948; 11: 199.
Roger H, Paillas JE, Bonnal J, Vigouroux R . Angiomes de la moelle et des raciness. Acta Neurol Psych Belg 1951; 7: 491–495.
Floris V . Angiomie angiomatosi del sistema nervoso. Lav Neuropsich 1958; 27: 159–379.
Hirsch JF, Pradat P, David M . Cavernous angioma of the cauda equina. Neurochirurgie 1965; 11: 323–327 (Fr).
Pansini A, Lo Re F . Raro caso di angiocavernoma della cauda. Mem Soc Tos Um Chir 1996; 27: 679–696.
Ortner WD, Kubin H, Pillz P . Ein zervikales kavernoeses angiom. Fortschr Roengtenstr 1973; 118: 475–476.
Heimberger K, Schnaberth G, Koos W, Pendl G, Auff E . Spinal cavernous haemangioma (intradural-extramedullary) underlying repeated subarachnoid haemorrhage. J Neurol 1982; 226: 289–293.
Ueda S, Saito A, Inomori S, Kim I . Cavernous angioma of the cauda equina producing subarachnoid hemorrhage. Case report. J Neurosurg 1987; 66: 134–136.
Pagni CA, Canavero S, Forni M . Report of a cavernoma of the cauda equina and review of the literature. Surg Neurol 1990; 33: 124–131.
Ramos Jr F, de Toffol B, Aesch B, Jan M . Hydrocephalus and cavernoma of the cauda equina. Neurosurgery 1990; 27: 139–142.
Mastronardi L, Ferrante L, Scarpinati M, Gagliardi FM, Celli P, Fortuna A . Intradural extramedullary cavernous angioma: case report. Neurosurgery 1991; 29: 924–926.
Mori K, Ishii H, Tomita Y, Nakajima K, Morimoto K, Maeda M . Intradural-extramedullary spinal cavernous angioma – case report. Neurol Med Chir (Tokyo) 1991; 31: 593–596.
Acciarri N, Padovani R, Pozzati E, Gaist G, Manetto V . Spinal cavernous angioma: a rare cause of subarachnoid hemorrhage. Surg Neurol 1992; 37: 453–456.
Sharma R, Rout D, Radhakrishnan VV . Intradural spinal cavernomas. Br J Neurosurg 1992; 6: 351–356.
Bruni P, Massari A, Greco R, Hernandez R, Oddi G, Chiappetta F . Subarachnoid hemorrhage from cavernous angioma of the cauda equina: case report. Surg Neurol 1994; 41: 226–229.
Cervoni L, Celli P, Gagliardi FM . Cavernous angioma of the cauda equina: report of two cases and review of the literature. Neurosurg Rev 1995; 18: 281–283.
Makino K, Takamura H, Gotoh S, Andoh M . Cauda equina cavernous hemangioma associated with hydrocephalus – case report. No To Shinkei (Jpn) 1995; 47: 783–787.
Rao GP, Bhaskar G, Hemaratnan A, Srinivas TV . Spinal intradural extramedullary cavernous angiomas: report of four cases and review of the literature. Br J Neurosurg 1997; 11: 228–232.
Nozaki K, Inomoto T, Taagi Y, Hasimoto N . Spinal intradural extramedullary cavernous angioma. Case report. J Neurosurg Spine 2003; 99: 316–319.
Falavigna A, Righesso Neto O, Nasser dos Santos JA, Patriani Ferraz FA . Cavernous angioma of the cauda equina: case report. Arq Neuro Psyquiatr 2004; 62: 1–8.
Fontane S, Melanson D, Cosgrove R, Bertrand G . Cavernous hemangiomas of the spinal cord: MR imaging. Radiology 1988; 166: 839–841.
Sindu M, Gilg A, Vighetto A, Jouvet A . Cryptic angioma in the trochlear nerve. Excision of the invaded portion and successful repair with an analogous graft: case report. Neurosurgery 1992; 30: 255–257.
Roncaroli F, Scheitauer BW, Krauss WE . Capillary hemangioma of the spinal cord. J Neurosurg (Spine 1) 2000; 93: 148–151.
Nowak DA, Widenka DC . Spinal intradural capillary haemangioma: a review. Eur Spine J 2001; 10: 464–472.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Caroli, E., Acqui, M., Trasimeni, G. et al. A case of intraroot cauda equina cavernous angioma: clinical considerations. Spinal Cord 45, 318–321 (2007). https://doi.org/10.1038/sj.sc.3101964
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101964