Abstract
Introduction
Intradural extramedullary capillary hemangiomas of the cauda equina are exceedingly rare, with only 20 previous cases reported. In the adult population, these tumors are rare and can arise in the central and peripheral nervous systems from the dura or spinal nerve roots. Intradural capillary hemangiomas of the cauda equina can yield symptoms such as lower extremity weakness, pain, and bladder and bowel dysfunction. The clinical symptomology and surgical management of this rare spinal lesion are reviewed in this case report.
Case presentation
A 50-year-old male presented with progressive bilateral lower extremity weakness for 2 years, with recent bladder and bowel dysfunction. On physical exam, strength was symmetrically impaired in both lower extremities. Pre-operative magnetic resonance imaging (MRI) of the lumbar spine demonstrated a gadolinium-enhanced intradural lesion at the L4 level. Laminectomy was performed and the lesion was resected. Histopathological analysis determined that the tumor demonstrated features consistent with a capillary hemangioma.
Discussion
Clinically, patients with capillary hemangiomas of the cauda equina present with space-occupying compressive deficits, including progressive low back and lower extremity pain, motor deficits, paresthesias, sensory loss, and bowel and bladder dysfunction. Acute presentation can transpire following a hemorrhagic episode, although this is more associated with cavernous rather than capillary hemangiomas. Our patient demonstrated non-acute, progressive weakness, and late-onset bladder and bowel dysfunction. This report demonstrates that this rare lesion should be included in the differential diagnosis of cauda equina lesions.
Similar content being viewed by others
Introduction
Capillary hemangiomas are benign tumors typically encountered as soft tissue or cutaneous lesions in the pediatric population [1]. In the adult population, these tumors are rare and can arise in the central and peripheral nervous systems from the dura or spinal nerve roots [1, 2]. Intradural capillary hemangiomas of the spine can occur in the lower lumbar region, causing cauda equina syndrome symptoms such as lower extremity weakness, pain, and bladder and bowel dysfunction [3, 4]. To date, <20 previous reports describing intradural capillary hemangiomas in the cauda equina have been reported (Table1) [4,5,6,7]. The clinical symptomology and surgical management of this rare spinal lesion are reviewed in this case report.
Case presentation
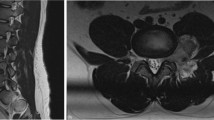
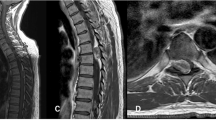
A 50-year-old male presented with progressive bilateral lower extremity weakness for 2 years. He also reported that recently he had developed bladder and bowel dysfunction. His past medical history was relevant for peripheral neuropathy secondary to type 2 diabetes mellitus. On the physical exam, strength was symmetrically impaired in both lower extremities, particularly in the quadriceps (4/5), anterior tibialis (1/5), extensor hallucis longus (1/5), and gastrocnemius (3/5). Sensory examination demonstrated signs of diabetic neuropathy in all four extremities. Patellar and Achilles reflexes were diminished bilaterally at 1+ and 0, respectively. Pre-operative magnetic resonance imaging (MRI) of the lumbar spine demonstrated a gadolinium-enhanced intradural lesion of ~1 cm at the L4 level, as well as short pedicles suggestive of congenital central stenosis at the L3–L5 levels (Fig. 1).
Pre-operative MRI demonstrating enhancement after gadolinium injection (B and E) and compression of the cauda equina at the level of L4 vertebral body. Sagittal (A) and axial (D) T1-weighted images pre-injection show an isointense signal. Sagittal (C) and axial (F) T2-weighted images pre-injection show hyperintense signal.
A L3–L5 laminectomy was performed, and after the thecal sac was opened, an ovoid intradural lesion was identified. Following meticulous arachnoid dissection, the cauda equina was separated from the tumor, except for a nerve root that could be seen entering and exiting the lesion. Intraoperative neurophysiological monitoring (IONM) was performed with somatosensory evoked potentials (SSEPs) and electromyography (EMG), and stimulation of the tumor capsule elicited a response in the anterior tibialis, gastrocnemius, and sacral rootlets. The area with the least conductivity in those groups was opened. The great majority of the lesion was resected. Only the fibrotic capsule, which had the neural tissue along its course, was left behind, and there was no change in IONM signals.
The tumor demonstrated features consistent with a capillary hemangioma, as it contained lobules consisting of small vessels lined by single layers of CD31 and ERG positive endothelial cells (Fig. 2). Mitotic figures were not apparent. S-100 immunohistochemical staining of the tissue sample was also positive at the periphery of the tumor, demonstrating areas of adhesion to the adjacent peripheral nerve root. The patient was discharged on the 5th postoperative day with bilateral improvement in the motor function (quadriceps (5/5), anterior tibialis (right: 2/5; left: 1/5), extensor hallucis longus (1/5), and gastrocnemius (4/5), as well as improvement in sensation in both the lower extremities.
Discussion
Vascular tumors represent 2–7% of intraspinal tumors [8]. Intradural extramedullary capillary hemangiomas of the cauda equina are exceedingly rare, with <20 previous cases reported. Of these reported cases, epidemiological findings demonstrate that the highest frequency of tumor occurrence is in males between the age of 40 to 60 [4]. Intradural capillary hemangiomas can arise from the inner surface of the dura, the pia, or from the vasculature of the nerve roots [8].
Clinically, patients with capillary hemangiomas of the cauda equina present with space-occupying compressive deficits, including progressive low back and lower extremity pain, motor deficits, paresthesias, sensory loss, and bowel and bladder dysfunction [7]. Acute presentation can transpire following a hemorrhagic episode, although this is more associated with cavernous rather than capillary hemangiomas [1, 8]. If possible, early resection is recommended due to the risk of hemorrhagic conversion, causing rapid neurological deterioration [4]. Our patient demonstrated non-acute, progressive weakness, and late-onset bladder and bowel dysfunction consistent with typical findings of the cauda equina lesions. The bilateral weakeness that our patient demonstrated was most likely due to the compounding effects that the space occupying tumor had on the patient’s history of lumbar stenosis.
Management is through surgical resection of the tumor, with full or partial resection being determined by the degree of nerve root involvement. Slight worsening of neurological status has been documented immediately after surgery due to surgical manipulation of the cord. Long-term neurological improvement is typically observed post-operatively, as symptoms usually stem from mass effect alone due to the tumor’s non-infiltrative nature [4, 8]. If partial resection is performed, patient follow-up is important to monitor recurrence. In our case, total resection was achieved, and neurological improvement was seen on the 5th post-operative day.
Histopathological findings demonstrate lobules with capillary-sized vessels lined with flattened endothelium. The lesions are typically surrounded by a fibrous capsule. The tumor cells stain strongly for endothelial markers such as CD31, CD34, and ERG, and can stain positive for neuron-specific enolase and S-100 as well [8]. On MRI, capillary hemangiomas characteristically show homogeneous hyperintensity post-gadolinium administration, although this finding is not specific, which makes histopathological analysis critical to definitive diagnosis [1, 4].
In conclusion, there are limited descriptions of intradural extramedullary capillary hemangiomas of the cauda equina in documented literature. This report demonstrates the clinical presentation, as well as the surgical management, and remarks that this rare lesion should be included in the differential diagnosis of cauda equina lesions.
References
Roncaroli F, Scheithauer BW, Krauss WE. Capillary hemangioma of the spinal cord: report of four cases. J Neurosurg Spine. 2000;93:148–51.
Mastronardi L, Guiducci A, Frondizi D, Carletti S, Spera C, Maira G. Intraneural capillary hemangioma of the cauda equina. Eur Spine J. 1997;6:278–80.
Roncaroli F, Scheithauer BW, Krauss WE. Hemangioma of spinal nerve root. J Neurosurg Spine. 1999;91:175–80.
Liu J, Kim K, Lee-Way J, Lee DJ. Intradural extramedullary capillary hemangioma of the cauda equina: case report and literature review. Surg Neurol Int. 2015;6:127.
Fish C, Sy J, Wong JH-Y. Capillary hemangioma of the cauda equina with high mitotic activity: case report and review of the literature. Diagn Pathol Open. 2019;4:3.
Pignotti F, Coli A, Fernandez E, Montano N. Capillary hemangioma of the cauda equina. Surg Neurol Int. 2015;6. https://doi.org/10.4103/2152-7806.162551.
Unnithan AKA, Joseph TP, Gautam A, Shymole V. Case report of lumbar intradural capillary hemangioma. Surg Neurol Int. 2016;7:S139–S141.
Miri SM, Habibi Z, Hashemi M, Meybodi A, Tabatabai SA. Capillary hemangioma of cauda equina: a case report. Cases J. 2009;2:80.
Zander DR, Lander P, Just N, Albrecht S, Mohr G. Magnetic resonance imaging features of a nerve root capillary hemangioma of the spinal cord: Case report. Can Assoc Radiol J. 1998;49:398–400.
Holtzman RN, Brisson PM, Pearl RE, Gruber ML. Lobular capillary hemangioma of the cauda equina. Case report. J Neurosurg. 1999;90 (2 Suppl):S239–41.
Ghazi NG, Jane JA, Lopes MB, Newman SA. Capillary hemangioma of the cauda equina presenting with radiculopathy and papilledema. J Neuroophthalmol. 2006;26:98–102.
Ganapathy S, Kleiner LI, Mirkin LD, Hall L. Intradural capillary hemangioma of the cauda equina. Pediatr Radiol. 2008;38:1235–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hughes, L.P., Largoza, G., Montenegro, T.S. et al. Intradural extramedullary capillary hemangioma of the cauda equina: case report of a rare spinal tumor. Spinal Cord Ser Cases 7, 21 (2021). https://doi.org/10.1038/s41394-021-00383-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-021-00383-9